HIV RISK REDUCTION INTERVENTIONS IN POPULATIONS WITH SERIOUS
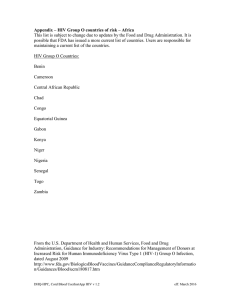
advertisement

HIV RISK REDUCTION INTERVENTIONS IN POPULATIONS WITH SERIOUS MENTAL ILLNESS: A CRITICAL REVIEW OF THE “SECOND GENERATION” by Annie Mae Marie Watson BS in Biochemistry, Allegheny College, 2006 Submitted to the Graduate Faculty of Graduate School of Public Health in partial fulfillment of the requirements for the degree of Master of Public Health University of Pittsburgh 2013 :de UNIVERSITY OF PITTSBURGH GRADUATE SCHOOL OF PUBLIC HEATLH This essay is submitted by Annie Watson on 2013 and approved by Essay Advisor: Beth A.D. Nolan, PhD _______________________________________ Assistant Professor Department of Behavioral and Community Health Sciences Graduate School of Public Health University of Pittsburgh Essay Reader: Jeremy Martinson, DPhil _______________________________________ Assistant Professor Department of Infectious Diseases and Microbiology and Human Genetics Associate Director, Bioscience of Infectious Diseases Graduate School of Public Health University of Pittsburgh ii Copyright © by Annie Watson 2013 iii Beth A. D. Nolan, PhD HIV RISK REDUCTION INTERVENTIONS IN POPULATIONS WITH SERIOUS MENTAL ILLNESS: A CRITICAL REVIEW OF THE “SECOND GENERATION” Annie Watson, M.P.H. University of Pittsburgh, 2013 ABSTRACT There is a disparity between the HIV prevalence in the seriously mentally ill (SMI) population (8%) as compared to the general population (0.6%) in the United States. In order to identify interventions for HIV prevention for people with SMI, a literature search was conducted in PubMed and PsychInfo. For PubMed, the following Medical Subject Headings (MeSH) terms were used: HIV Infections, Prevention and control, and Mental Disorders. For PsychInfo the following terms were used in the search: Mental Disorders and HIV. Sixteen independent studies were found after being subjected to inclusion and exclusion criteria. The most notable finding of this study was that effective gender-specific interventions have been designed and implemented in SMI populations. Also HIV prevention interventions have demonstrated changes in attitudes and HIV related risk behaviors in this population. However analysis by some of the studies revealed that the intervention outcomes can be impacted by individual differences (i.e. race, psychiatric diagnosis, and reported substance use). The issue of exploring subpopulations among people with SMI is the next suggested step in combatting this issue. This essay is of public health significance because it explores the issue of reducing HIV related risk behaviors in people with mental illness in order to reduce their chance of contracting this deadly virus. iv TABLE OF CONTENTS 1.0 INTRODUCTION ........................................................................................................ 1 1.1 HIV AND PUBLIC HEALTH THEORIES ...................................................... 2 1.1.1 HIV Overview .................................................................................................. 2 1.1.2 Public Health Theories of Behavioral Change .............................................. 2 1.2 HIV AND SMI...................................................................................................... 3 1.2.1 SMI .................................................................................................................... 3 1.2.2 HIV Risk Factors ............................................................................................. 5 1.2.3 HIV Prevalence ................................................................................................ 7 1.3 INTERVENTIONS (1988 - 1996) ....................................................................... 7 1.3.1 1.4 METHODS ......................................................................................................... 10 1.4.1 2.0 Review Procedure .......................................................................................... 10 RESULTS .................................................................................................................... 12 2.1.1 3.0 Intervention study Review .............................................................................. 7 Overview ......................................................................................................... 12 2.2 MALES AND FEMALES ................................................................................. 14 2.3 MALES ............................................................................................................... 21 2.4 FEMALES .......................................................................................................... 24 DISSCUSSION ........................................................................................................... 27 v 3.1.1 Differences in the Intervention by Gender .................................................. 27 3.1.2 Race & Ethnicity ............................................................................................ 29 3.1.3 Psychiatric Diagnosis ..................................................................................... 30 3.1.4 Dosage of Intervention .................................................................................. 30 3.1.5 Theory ............................................................................................................. 31 3.1.6 Limitations ..................................................................................................... 32 3.1.6.1 Limitations to the literature search ................................................... 33 3.1.6.2 Limitations to the research studies .................................................... 33 3.1.7 Future Directions ........................................................................................... 34 3.1.7.1 Literature Search ................................................................................ 35 3.1.7.2 HIV Prevention Studies ...................................................................... 35 3.1.8 Conclusions..................................................................................................... 38 APPENDIX...................................................................................................................................41 BIBLIOGRAPHY ....................................................................................................................... 43 vi LIST OF TABLES Table 1. HIV Intervention Studies ......................................................................................... 40 vii PREFACE Acknowledgements: My Family for all their love and support (Joan Watson, Joanie ‘Vina’ Watson; Roman Watson-Bush, Dr. Richard Watson, Jennie Watson, Benji Watson, and Teddy Watson); My essay advisor Dr. Beth Nolan; My mentor Dr. Vishwajit Nimgaonkar; Dr. Martha Terry; My Inspiration Dr. DeGenna Natacha; David Roofeh; Dr. Mikhil Bamne; Dr. Hader Mansour; Dr. Jeremy Martinson; NAMI Southwestern Pennsylvania and Mim Schwartz. viii 1.0 INTRODUCTION There is a disparity between the prevalence of human immunodeficiency virus (HIV) in the population of those with serious mental illness (SMI): 8% (Meade & Sikkema, 2005) as compared to the general population 0.7% (The World Bank, 2011) in the United States (US). Due to this disproportion disease burden the National Institute of Mental Health (NIMH) consider those with SMI to be part of an HIV vulnerable population (1993). The purpose of this essay is to critically review studies that have conducted HIV prevention interventions in those with SMI. The essay will first give brief information about HIV, then frame HIV as a public health issue in this population and discuss a previous review of HIV interventions that have been conducted in those with SMI. The methodology used in this literature review and then an extensive review of all of the identified intervention studies will be presented. Finally, themes in the literature will be identified, limitations to the field and this literature review will be discussed, future directions will be suggested and finally conclusions about the field will be made. 1 1.1 HIV AND PUBLIC HEALTH THEORIES 1.1.1 HIV Overview Awareness of HIV that can develop into acquired immune deficiency syndrome (AIDS) first occurred in the US in 1981, but the identification of the virus and knowledge about transmission were not determined until later (AVERT, 2013). HIV is primarily spread through unprotected sex with an infected partner, sharing needles and other intravenous (IV) drug equipment with an infected individual and vertical transmission from an infected mother to a child. Despite major advances in the diagnosis and treatment of HIV infection, there is no cure (CDC, 2012). Therefore, evidence based effective HIV primary prevention programs continue to be important against the HIV epidemic (The White House, 2010). 1.1.2 Public Health Theories of Behavioral Change The use of behavioral health theory is considered to be the best practice and essential to establishing effective evidence-based HIV prevention programs by the U.S. government organizations such as the Center for Disease Control (CDC) (Jacobs, Jones, Gabella, Spring, & Brownson, 2012) and NIMH (2012). HIV prevention programs target behavioral change at one or more of these levels: individual, interpersonal, community and structural and environmental factors. Evidence based HIV interventions have utilized behavioral change theories or models such as Social Cognitive Theory (Bandura, 1986), Social Learning Theory (Bandura, 1977), AIDS Risk Reduction Model (Catania, Kegeles, & Coates, 1990), Information-Motivation2 Behavioral Model (Fisher & Fisher, 1992), Health Belief Model (Rosenstock, Strecher, & Becker, 1988), Stages of Change (Transtheoretical) Model (Prochaska, DiClemente, & Norcross, 1992), and the Theory of Gender and Power (Connell, 1987) to design and evaluate their interventions (Holtgrave et al., 1995; Lyles et al., 2007; Traube, Holloway, & Smith, 2011; Washington State Department of Health, n.d). Many other competing behavioral health theories are also used and research is still being conducted to determine which of the multitude of theories are the more effective at targeting this public health issue (Holtgrave et al., 1995; Lyles et al., 2007; Traube et al., 2011). 1.2 HIV AND SMI 1.2.1 SMI The most widely accepted definition of severe mental illness (SMI) was defined by NIMH in 1987 and uses three criteria: the type of mental illness, the duration of the mental illness, and the level of functional impairment (severity) experienced by the affected individual (1987). The mental health diagnosis must be either a type of non-organic psychosis (e.g. schizophrenia, schizoaffective disorder) or personality disorder (e.g. borderline personality disorder). Therefore the onset of symptoms cannot be preceded by organic causes like brain trauma or drug induced psychosis. The individual must have a prolonged duration of the illness; operationally defined as the presence of symptoms for two of more years and can be established through previous hospitalization or outpatient treatment history. The functional impairment is defined by dangerous or disturbing social behavior, moderate impairment in work and occupational 3 activities and mild impairment in basic needs (National Institute of Mental Health, 1987; Parabiaghi, Bonetto, Ruggeri, Lasalvia, & Leese, 2006; Ruggeri, Leese, Thornicroft, Bisoffi, & Tansella, 2000). Frequently a measure of dysfunction known as the Global Assessment of Functioning (GAF) scale (American Psychiatric Association, 1987) is used to establish severity of the functional impairment (Ruggeri et al., 2000). However, this definition of SMI continues to be evaluated. The most debated part of the NIMH definition is the required mental health diagnostic criteria of non-organic psychosis and personality disorder. Alternative definitions include only the severity and duration criteria, in recognition of the fact that other mental health disorders (e.g. major depression, panic disorder, and obsessive compulsive disorder) can cause impairment and long term mental health services utilization (Parabiaghi et al., 2006; Ruggeri et al., 2000). For the purpose of this literature review the definition of SMI will be liberal, where at least one of the three NIMH criteria should be mentioned as inclusion criteria for study participants. The symptoms of schizophrenia, schizoaffective disorder, bipolar disorder, and major depressive disorder commonly can lead to severe life impairment that lasts longer than six months. It is estimated that 2.6% of US adults meet criteria for SMI (Kessler, 1996). On average 29% of this population has a co-occurring substance abuse issue, but the percentage in the subpopulations grouped by mental health diagnosis varies (Regier et al., 1990). Many individuals with SMI face social economic issues such as homelessness (approximately 30%) (SAMHSA, 2011). Contrary to stigma-biased beliefs, this population is sexually active, with 60.07% reporting sexual activity in the last twelve months, and 45.91% reporting sexual activity in the past three months (Meade & Sikkema, 2005). The type and methodological measurement of the 4 sexual activity varied across the reviewed studies (Meade & Sikkema, 2005). While the epidemiological factors that puts those with SMI at greater risk of sexually transmitted diseases such as HIV are complex, the types of sexual interactions and substance abuse are contributing factors (Meade & Sikkema, 2005). 1.2.2 HIV Risk Factors Meade and Sikkema (2005) conducted a systematic review of the sexual risk factors in this population, then weighed data from the studies, and reported mean HIV risk prevalence. The authors found that the primary risk factors included: unprotected intercourse, multiple sexual partners, high-risk partners (e.g. IV drug users), anonymous sexual partners, and use of drugs and/or alcohol before sex. Forty three percent of the SMI population self-reported that they had two or more partners within the past year before the original study data was collected. Forty six percent of the SMI population surveyed had never used a condom within this same time period (41.76% in the past three months before the original study data was collected). Twenty two percent of the SMI population in the reviewed studies admitted to having a lifetime history of sex trade (Meade & Sikkema, 2005). An increase in HIV risk was associated with indirect evidence of unhealthy substance use (e.g. alcohol use, illicit drug use, substance use disorder) (Carey, Carey, Maisto, Gordon, & Vanable, 2001; Kalichman, Kelly, Johnson, & Bulto, 1994; Rosenberg et al., 2001). Living in an urban area increases the HIV risk (Brunette et al., 1999), while homelessness might be a modifying or confounding risk factor (Meade & Sikkema, 2005). Other factors that increase the susceptibility of this population to HIV are the severity and symptomology of psychopathology. Studies examining the association between symptoms 5 (psychopathology, cognitive, excitement, positive and negative symptoms) have found that current symptoms are associated with sexual risk factors, though specific results varied across studies (Cournos et al., 1994; Horwath, Cournos, McKinnon, Guido, & Herman, 1996; McKinnon, Cournos, Sugden, Guido, & Herman, 1996; Rosenberg et al., 2001). Although most studies also found no association between the primary Axis I psychiatric diagnosis (e.g. schizophrenia, bipolar disorder, major depressive disorder; (American Psychiatric Association, 2000) and HIV risk (e.g. Brunette et al., 1999; Carey et al., 1999; Carey et al., 2001), there are differences in HIV risk factors by psychiatric diagnosis. Most studies find that people with schizophrenia spectrum disorders were significantly less likely to be sexually active as compared to those with other major psychiatric disorders (e.g. Carey et al., 1999; Carey et al., 2001). A diagnosis of unipolar depression was associated with injection drug use (McDermott, Sautter, Winstead, & Quirk, 1994). There is an association between having both a primary psychiatric diagnosis and a personality disorder with greater HIV risk (Sacks, Perry, Graver, Shindledecker, & Hall, 1990). Other factors that increased HIV risk directly or an HIV risk factor are trauma exposure (Rosenberg et al., 2001), social relationship status (i.e. single or in a relationship) (Grassi, Pavanati, Cardelli, Ferri, & Peron, 1999; Kalichman et al., 1994; Kelly et al., 1992) and cognitive–behavioral factors (e.g. self-efficacy and lower motivation for condom use; e.g. Carey, Carey, Weinhardt, & Gordon, 1997; Kelly et al., 1995; McDermott et al., 1994; Meade & Sikkema, 2005). Given the unique and complex HIV risk factors, it is not surprising that HIV seroprevalence of adults with SMI in the US is higher than the rest of the general US population (Cournos & McKinnon, 1997). 6 1.2.3 HIV Prevalence The studies conducted to date have estimated the seroprevalence of adults with SMI range from 4% to 23% of the US population with SMI (Cournos & McKinnon, 1997). The lowest rate of HIV infection (4%) was found among patients on a long-term stay acute psychiatric unit (Meyer et al., 1993). The highest rate of HIV infection (22.9%) was found in a unit treating patients with a dual-diagnosis of severe mental illness and substance use disorder (Silberstein et al., 1994). The second highest HIV seroprevalence (19.4%) population was among homeless, nonhospitalized males receiving community psychiatric treatment (Susser, Valencia, & Conover, 1993). Cournos and McKinnon (1997), estimated the aggregated seroprevalence of HIV in SMI populations from several studies to be 8.1% for males and 6.4% for females, which is higher than the CDC’s (2011) estimated prevalence of the general US population of 0.52% for males and 0.16% for females. Based on this difference in HIV prevalence, the NIMH identified the SMI population as one of the AIDS groups of concern (1993). 1.3 INTERVENTIONS (1988 - 1996) 1.3.1 Intervention study Review This is not the first literature review of intervention studies targeting SMI individuals to reduce their HIV related risk behaviors (e.g. unprotected sexual intercourse and multiple sexual partners); a systematic review identified studies published between 1988 and 1996 (Kelly, 1997). All of the studies used public health theories [e.g. the Social Learning Theory (Bandura, 1977) or 7 Cognitive Behavioral Theory (Bandura, 1986), the Theory of Reasoned Action (Fishbein & Ajzen, 1975) to develop and evaluate the HIV risk reduction interventions (Kelly, 1997). These studies were conducted primarily on mixed gender participants, while only one was conducted on HIV negative adults (Susser et al., 1996). None of the studies were conducted on female only populations (Kelly, 1997). Of the reviewed studies (Kelly, 1997), three were randomized control trials (RCT) of the adult SMI participants (Kalichman, Sikkema, Kelly, & Bulto, 1995; Kelly et al., 1996; Susser et al., 1996). Kelly (1997) concluded that: “relatively intensive, theoretically-based, and culturally-tailored behavior change programs can impact so as to reduce sexual risk practices even among persons with long histories of mental illness and other coexisting problems” (p. 306-307). Effective interventions were intensive (6 to 15 hours long; Kalichman et al., 1995; Susser et al., 1996). They had multiple theoretical construct outcomes (e.g. attitudes towards HIV prevention related behaviors, behavioral intention, and self-efficacy; Kalichman et al., 1995; Kelly et al., 1996; Susser et al., 1996). Many studies tailored their intervention to SMI participants by using small group formats and cognitive and behavioral skills building to improve and encourage use of HIV preventative skills in real world situations, as this has been found to be effective format in other psychosocial rehabilitation programs (Wallace, Liberman, MacKain, Blackwell, & Eckman, 1992) Kelly (1997) suggested that HIV prevention programs would benefit from more RCT design (previously the studies were mostly anecdotal reports or uncontrolled pre-post evaluation 8 design), use of realistic risk situations, instead of “generic” ones, more external validation measures, increased use of behavioral change endpoints and larger samples. Other suggestions included targeting more interventions levels (individual and community), having longer followup periods and having gender specific interventions (Kelly, 1997). Kelly speculated that people with SMI would probably benefit the most from and HIV program if their other basic and psychiatric needs were met though community resources. Community or system level interventions have been found to be effective for other AIDS-vulnerable populations (Danya International, 2012; Kelly, 1997). Longer follow-up periods are necessary to establish maintenance of behavior change, which is important if people with SMI are continuously as risk for contraction of HIV infection. As females with SMI have different HIV risk profile than males with SMI (e.g. economic dependence on the male partner, relationship power imbalance, and whom partner resistance to condom use; e.g. Amaro, 1995; Ickovics & Rodin, 1992; Nyamathi, Bennett, Leake, Lewis, & Flaskerud, 1993) separate interventions designed specifically for males or females could target these unique HIV risk factors. Kelly advocated for using the individual format, so that HIV infection in SMI individuals could be offered screening as part of routine admission to psychiatric facilities, as high rates of undetected HIV infection have been found in those receiving inpatient services (Sacks, Dermatis, Looser-Ott, Burton, & Perry, 1992). Also, HIV testing and counseling is usually preformed on a one-on-one basis (Kelly, 1997). Kelly’s (1997) review of the HIV interventions conducted with SMI participants found that HIV risk behavior could be reduced in this population, but there were several aspects in the scientific design and implementation that could be improved. Individuals with SMI have a higher prevalence of HIV than the general population (Meade & Sikkema, 2005), as such they are considered to be an HIV vulnerable population by the NIMH 9 (National Institute of Mental Health, 1993). Previous research in this area found that HIV interventions were an effective way to reduce HIV risk behaviors in this population, but the field would benefit from more well-designed studies (Kelly, 1997). A recent study found that an HIV intervention conducted in an SMI population was cost effective when considering the long-term cost of treatment of HIV in these individuals (Pinkerton, Johnson-Masotti, Otto-Salaj, Stevenson, & Hoffmann, 2001). A critical review of the outcomes, study design, and the participants’ characteristics will further the objectives of the NIMH and systematically explore this important public health issue facing this marginalized population. 1.4 METHODS 1.4.1 Review Procedure A systematic review of the published literature was performed to identify empirical studies on HIV prevention interventions among adults with SMI in the United States and internationally. PsychInfo and PubMed, two online databases in the social and health sciences, were searched for English publications. For PubMed, the following Medical Subject Headings (MeSH) terms were used: HIV Infections, Prevention and control, and Mental Disorders. For PsychInfo the following terms were used in the search: Mental Disorders and HIV. Additionally, studies were obtained through bibliographic review of acquired publications. The inclusion criteria were: (1) sample of adults with SMI, (2) the population studied had a primary psychiatric diagnosis that is not alcohol or substance abuse, (3) presentation of 10 quantitative data, (4) assessment of at least one knowledge acquisition or behavioral outcome (e.g., an increase in HIV risk knowledge, decrease in sexual activity, decrease number of partners, and increase in condom use for males or females), (5) studies appeared in a peer reviewed journal, and (6) those studies not published in a previous comprehensive review. The exclusion criteria were: (1) studies that reported aggregate results of populations with a SMI and without (for example many studies conducted in correctional facilities), (2) studies with anecdotal or qualitative data collected in a non-systematic way, and (3) publications reviewed by J. A. Kelly in 1997 were excluded because critical analysis and commentary has already been concluded (Kelly, 1997); with the exception of a study by Susser and colleagues (Susser et al., 1998) of which some of the unpublished results (Susser et al., 1996) were reviewed by Kelly (1997). The first round exclusion of search results was based on the title, second round exclusion was based on the abstract, and then finally the exclusion criteria were applied to the entire paper. Multiple publication using the same data were counted as one study. Findings on the outcomes of the HIV intervention in SMI populations were compiled. 11 2.0 RESULTS An overview of the HIV intervention studies conducted on SMI populations that were found as part of this critical literature review will be presented, then the studies will be presented based on the gender of the participants (Males and Females, Males, and Females) with a brief summary of the main findings given. 2.1.1 Overview A PubMed database search using “HIV Infections AND prevention and control AND Mental Disorders NOT Needle NOT opioid” yielded 4,145 results on January 25, 2012. A PsychInfo database search using “Mental Disorders AND HIV” yielded 6,719 results on February 1, 2012. After applying exclusion and inclusion criteria, only 16 independent studies were found (Table 1). Two studies yielded two publications from the same data or a subset thereof (Otto-Salaj, Kelly, Stevenson, Hoffmann, & Kalichman, 2001; Pinkerton et al., 2001). Sample sizes ranged from seven (Jordan & Selwyn, 2008) to 408 participants (Carey et al., 2004). Ten of the studies were RCTs (Berkman, Cerwonka, Sohler, & Susser, 2006; Berkman et al., 2007; Carey et al., 2004; Collins, Geller, Miller, Toro, & Susser, 2001; Collins et al., 2011; The National Institute Of Mental Health Multisite HIV Prevention Trial Group, 2006; Hajagos, Geiser, Parker, & Tesfa, 1998; Otto-Salaj et al., 2001; Susser et al., 1998; Weinhardt, Carey, Carey, & Verdecias, 12 1998). Studies recruited participants from outpatient clinics (50%) (Collins et al., 2011; Weinhardt et al., 1998; Berkman et al., 2007; Carey et al., 2004; The National Institute Of Mental Health Multisite HIV Prevention Trial Group, 2006; Kalichman, Malow, Devieux, Stein, & Piedman, 2005; Otto-Salaj et al., 2001; Rosenberg et al., 2004), inpatient units (19%) (Collins et al., 2001; Williams, Donnelly, & Proesher, 2001; Meyer, Cournos, Empfield, Agosin, & Floyd, 1992) and other community programs (31%) (Berkman et al., 2006; Collins et al., 2011; Jordan & Selwyn, 2008; Sikkema et al., 2007; Susser et al., 1998); 37.5% of studies were implemented at multiple sites (Carey et al., 2004; Collins et al., 2011; The National Institute Of Mental Health Multisite HIV Prevention Trial Group, 2006; Otto-Salaj et al., 2001; Rosenberg et al., 2004; Sikkema et al., 2007). Although the geographic location was not an exclusion criteria, all of the 16 studies were conducted in the United States, primarily in New York (11 studies) (Collins et al., 2001; The National Institute Of Mental Health Multisite HIV Prevention Trial Group, 2006; Weinhardt et al., 1998; Berkman et al., 2006; Berkman et al., 2007; Carey et al., 2004; Collins et al., 2011; Hajagos et al., 1998; Jordan & Selwyn, 2008; Meyer et al., 1992; Susser et al., 1998), other urban areas (five studies) (The National Institute Of Mental Health Multisite HIV Prevention Trial Group, 2006; Kalichman et al., 2005; Otto-Salaj et al., 2001; Sikkema et al., 2007; Williams et al., 2001), one in a rural area (Rosenberg et al., 2004). The majority of the participants had a diagnosis of SMI for all studies except one of the studies that discussed SMI criteria without collecting a formal psychiatric diagnosis The National Institute of Mental Health Multisite HIV Prevention Trial Group, 2006). Thirty one percent collected psychiatric diagnosis data through a diagnostic interview (e.g., The Structured Clinical Interview for DSM-IV; Berkman et al., 2006; Berkman et al., 2007; Carey et al., 2004; Collins et al., 2011; First, Gibbon, Spitzer, Williams & Benjamin, 1997; Susser et al., 1998) and 56% relied on 13 medical charts, clinician report, or clinical referrals (Collins et al., 2001; The National Institute Of Mental Health Multisite HIV Prevention Trial Group, 2006; Hajagos et al., 1998; Jordan & Selwyn, 2008; Kalichman et al., 2005; Meyer et al., 1992; Otto-Salaj et al., 2001; Rosenberg et al., 2004; Sikkema et al., 2007; Weinhardt et al., 1998; Williams et al., 2001), a diagnosis was not collected for one of the studies (The National Institute Of Mental Health Multisite HIV Prevention Trial Group, 2006), and one study did not provide enough details (Jordan & Selwyn, 2008); 13% included some measure of functional impairment in their criteria (Carey et al., 2004; The National Institute Of Mental Health Multisite HIV Prevention Trial Group, 2006). Table 1 reports the study details and eligibility criteria beyond a diagnosis of SMI, except specific high risk HIV risk criteria that varied across studies (e.g., homelessness, substance dependence, HIV negative) and participant characteristics by study. 2.2 MALES AND FEMALES There were eight studies that included both males and females as participants. Of these, only one of the interventions included medical services including testing and counseling for the results of an HIV blood test as part of their methodology (Rosenberg et al., 2004). The rest used solely knowledge and skills based approaches to HIV prevention behavior. The smallest study was completed in a community psychiatric facility, referred to as a Clubhouse. The initial ten session behavioral skill and decision making centered intervention was shortened to six sessions to increase study retention. Although the total enrollment of three iterations of the intervention was 47 SMI individuals, only seven of these completed pre- and 14 post- intervention surveys. Due to the small number of completed surveys, a formal statistical analysis could not be completed, however HIV knowledge and self-efficacy (a person’s belief in their own ability to perform the HIV prevention behavior; (Glanz, 2008) scores increased from pre- to post- intervention testing (Jordan & Selwyn, 2008). In another small study, 12 patients recruited from an inpatient psychiatric unit located in New York participated in a program that consisted of 75 minute sessions held once a week, for seven weeks (Meyer et al., 1992). The program used the Health Belief Model (Rosenstock et al., 1988) to modify the participants’ perceived susceptibility/risk of getting HIV, perceived severity of HIV, perceived barriers to reducing HIV risk behaviors, the perceived benefits of reducing HIV risk behaviors, and self-efficacy. The study used informational materials, educational videotapes, discussions, role play and other educational games. Some of the titles of the topics included AIDs Knowledge, Heterosexual/Homosexual Transmission and IV Drug Use. Increasing the participants’ sense of self-efficacy of procuring and using condoms was part of the program. Due to the small sample size Meyer and colleagues (1992) were unable to access their pilot study for statistical significance, so efficacy could not be established. However, the mean scores on the AIDs Knowledge Questionnaire did improve; the questionnaire was developed by the Meyer and colleagues (1992). The health belief model was not the only public heath theory used in HV interventions with SMI populations. Another intervention used both the social learning theory (Bandura, 1977) and the Transtheoretical model of behavior change (Prochaska et al., 1992) to promote readiness to change HIV prevention behavior among a sample of psychiatric patients recruited from an inpatient unit (Williams et al., 2001). There were 50 participants who completed the four, 30 minute long intervention sessions titled Facts for Life. Facts for Life consisted of repetitive 15 iterations of material, role-playing, simple assignments, and skills training. The Rhode Island Change Assessment (McConnaughy, DiClemente, Prochaska, & Velicer, 1989) was administered pre- and post-intervention and differences in scores were evaluated using two-tailed t-tests. Differences of readiness for change were noted between male and female participants. Females had a significant change in the domain of pre-contemplation, while males had significant change in the domain of action. The type of SMI diagnosis was associated with different intervention outcomes, significant changes in the domain of contemplation was found for patients diagnosed with a psychotic disorder and in the domain of action for those with a mood disorder (Williams et al., 2001). Instead of recruiting participants from inpatient psychiatric units, a study by Otto-Salaj and colleagues (2001) recruited 189 males and females from five community outpatient programs in Milwaukee, WI. All participants had at least one of five study specific HIV high risk criteria and were randomly assigned to attend either a seven-session, small-group, cognitivebehavioral, HIV risk reduction intervention derived from social cognitive theory (Bandura, 1986) or a time-matched, comparison intervention. The intervention was held biweekly and a “booster” session was held at month-one and month-three. Self-reported measures for HIV risk behavior, knowledge, high-risk sexual behavior, risk reduction behavioral intentions and condom attitudes were assessed at baseline, immediately post-intervention, and then every three months postintervention for one year. Changes in high-risk sexual behavior were measured by frequency of protect and unprotected sexual intercourse and the number of sexual partners. Gender was an important demographic variable that impacted the intervention outcomes. When compared to male controls, the males in the intervention group had a significant change in HIV risk knowledge scores between baseline and the three, six, and nine-month follow-up. When 16 compared to the female controls, the females in the intervention group had significant changes in attitudes toward condom use, risk reduction behavioral intentions, and sexual behavior between baseline and the three, six and nine-month follow-up The most notable sexual behavior change was the percentage of condom protected vaginal intercourse occasions in the female intervention group increased significantly, compared to the controls. The attitude and behavioral changes associated with the intervention were not maintained to the 12-month follow-up (Otto-Salaj et al., 2001). Although cost is an important factor in program planning, this was the only study to publish a formal cost-effectiveness analysis of the HIV prevention intervention on the SMI participants. Data was analyzed using the entire participant group and due to the above noted differences in gender, only the females were used for this analysis. Two analyses were conducted one with all the females and another with only a subset that self-reported being sexually active in the three months prior to the intervention. The authors modeled the costs of HIV related medical costs that could be saved given the intervention’s small effect on reducing HIV risk to calculate the cost per quality-adjusted life year saved (QALYS). The QALYS was $136,295 for all the females in the intervention and $71,367 per QALYS for the sexually active females. The QALYS for the intervention was between the $60,000 to $180,000, which is the range that is generally considered to be cost-effective and fundable by society (Tengs et al., 1995). Due to the difference in the QALYS, the authors suggested screening for recent sexual activity to increase the cost-effectiveness, but also acknowledge that this type of screening could potentially lead to exclusion of some high risk individuals (Pinkerton et al., 2001). In another randomized control trial (RCT), outpatients with SMI participated in a 10session HIV-risk-reduction intervention (HIV-R) and a substance use reduction intervention (SUR). The 221 female and 187 male participants were assigned to the HIV-R, SUR or the 17 treatment as usual group. The HIV-R was designed using the information-motivation-behavioral skills theory (IMB; Fisher & Fisher, 1992). The participants self-reported historical occasions of unprotected vaginal sex, number of sexual partners, and communication skills regarding safer sex at pre-, post-intervention and 3 and 6-month follow-ups. The history of a sexually transmitted infection (STI) was also collected at baseline and 6-month follow-up. All the constructs of the IMB (Fisher & Fisher, 1992) were assessed. Compared to the control group, the HIV-R group significantly decreased the occasions of unprotected vaginal sex and number of sexual partners, and increased the communication skills regarding safer sex with a partner. The SUR group improved in all but the later variable. The HIV-R group significantly improved HIV knowledge, increased positive condom attitudes, had stronger condom use intentions and improved behavioral skills relative to patients in the SUR and control conditions. The HIV-R group reported fewer new STIs than the control group. Gender difference in HIV-R outcomes were noted, with females benefiting the most. The type of SMI diagnosis also impacted the HIVR outcomes, with individuals with Major Depressive Disorder benefiting the most (Carey et al., 2004). A one-hour medical model of HIV prevention known by the action verbs: screen, test, immunize, reduce risk, and refer (STIRR), was evaluated at two community mental health centers. The intervention consists of HIV risk screening, testing for HIV and hepatitis, immunization for hepatitis A and B, risk-reduction counseling and treatment referral for bloodborne infections. Changes in AIDS risk was only assessed at one of the sites, where 50 participants completed the AIDS Risk Inventory (measures self-reported HIV knowledge, motivation, and risk behaviors) (Chawarski, Pakes, & Schottenfeld, 1998). Results were analyzed with paired t-test and the intervention was associated with significant increased HIV 18 knowledge and motivation to reduce risk in the participants. Although a formal cost-utility analysis was not performed for this intervention, the direct cost for the intervention were about $220 plus the cost of the Hepatitis A and hepatitis B vaccine per individual (Rosenberg et al., 2004). A study using the IMB model (Fisher & Fisher, 1992) recruited only participants (N = 320; 150 females and 170 males) who were considered to have a SMI and unhealthy alcohol or drug use who were attending a community based treatment abuse programs located in MiamiDade Florida. Assessments for all the IMB (Fisher & Fisher, 1992) constructs were used with the primary outcomes focused on condom use during vaginal intercourse. Direct observations of participants’ condom skills were assessed. A measure of sexual risk behavior was also included. The results of the intervention differed by gender. Males showed only significant changes in HIV knowledge scores in response to the intervention between baseline and 6-month follow-up. Females showed significant changes in condom attitudes, risk reduction behavioral intentions, and reported reductions in sexual risk behaviors between baseline and 6-month follow-up. The study developed a theoretical model of HIV prevention in SMI based on the data collected. Briefly, a positive personal attitude about condoms, perceived pro-condom norms, and increasing condom self-efficacy is associated with increased condom use in SMI population, especially in females (Kalichman et al., 2005). A study using the social cognitive theory (Bandura, 1986) was conducted at two community supportive housing programs (SHP) for people with SMI. The intervention consisted of an initial six-sessions (nine hours total) of HIV prevention skills group training and then a four month intervention targeted at changing social norms surrounding HIV prevention. Peer leaders from the residents of the SHPs and the staff of the SHPs were trained to implement the social 19 norms intervention. A total of 28 residents (17 males and 11 females) answered questions about sexual behavior, substance abuse, HIV knowledge, condom self-efficacy, sexual communication self-efficacy, condom attitudes, safer sex norms and risk reduction behavioral intentions at baseline, after skills training, and after the social norms intervention. There were significant differences between the baseline and the post assessment (after the skills training intervention) and the baseline and the follow-up (after the skills training and social norms intervention) in the areas of condom use, sexual communication, condom attitudes, and behavioral intentions. After both the skills training and social norms intervention the participants reported significant changes in HIV knowledge. Self-reported sexual activity was low in the population, so behavioral analysis was not feasible (Sikkema et al., 2007). All eight studies that included both males and females as participants were successful in demonstrating a changes in HIV risk knowledge (Kalichman et al., 2005; Sikkema et al., 2007; Carey et al., 2004; Williams et al., 2001; Otto-Salaj et al., 2001; Pinkerton et al., 2001; Jordan & Selwyn, 2008; Meyer et al., 1992), but due to a small sample size two studies were unable to demonstrate statistical efficacy (Jordan & Selwyn, 2008; Meyer et al., 1992). Only four (Williams et al., 2001; Otto-Salaj et al., 2001; Carey et al., 2004; Kalichman et al., 2005) of the eight studies were able to demonstrate differences in HIV risk behavior in a subset of their subjects (i.e. male or female). In these four studies, a difference was noted between males and females in study outcomes, with females generally benefiting more from the interventions (Williams et al., 2001; Otto-Salaj et al., 2001; Carey et al., 2004; Kalichman et al., 2005). As such, the following sections provide information of interventions by gender. 20 2.3 MALES There were five studies that included just males as participants. Of these, three used variations of a cognitive-behavioral intervention based on social learning theory known as “Sex, Games, and Videotapes” (SexG), while the other two used a similar multi-faceted approach to HIV prevention behavior. A randomized clinical trial with an 18 months follow-up assigned participants to one of two intervention groups: a15-session, experimental group intervention known as “Sex, Games, and Videotapes” (SexG) or to a 2-session control intervention. The participants had a SMI, and were recruited from a psychiatric program in a homeless shelter. A total of 97 males participated, but only a subset of 59 participants who were sexually active was used for the sexual risk behavior outcomes. Compared to the control cohort, the intervention cohort had a three times lower sexual risk index as measured by the Sexual Risk Behavior Assessment Schedule (SERBAS; Meyer-Bahlburg, Ehrhardt, Exner, & Gruen, 1991) at the 6-month follow-up. Essentially, the SERBAS measures number of protected and unprotected sexual interactions (vaginal, anal, and oral) and sexual partners and then a sexual risk index score is derived. Therefore a lower sexual risk index indicates less unprotected sex with casual and occasional partners. The differences on the SERBAS between the two cohorts decreased by the 18-month follow-up (Susser et al., 1998). The data from this study was analyzed to determine the impact of a lifetime history of substance dependence on the efficacy of SexG intervention. When compared to the controls, no significant reduction in HIV risk, as measured by the SERBAS, was found in the substance (alcohol/drugs)-dependent males (Berkman et al., 2005). To increase the feasibility of implementing the SexG intervention in the community mental health settings, Berkman and colleagues (2006) developed a shorter version, with six21 sessions known as SexG-Brief. The results of an RCT with 92 male participants did not show any significant differences in HIV risk behaviors, although a decreasing trend was noted (a twofold reduction in sexual risk scores for those in the intervention group at the 6-month followup as compared to the control group). The participants were recruited from a homeless shelter and three transitional living communities for males with SMI in New York City (Berkman et al., 2006). Based on the results of interventions with SexG and SexG-Brief, Berkman and colleagues (2007), developed another version of the intervention, Enhanced SexG (E-SexG), with 10sessions, peer advocacy, and three month booster sessions (total of three). To test the efficacy of E-SexG intervention, 149 eligible participants were recruited from eight psychiatric outpatient clinics in the New York metropolitan area and were randomly assigned to the experimental or control conditions. Participants completed assessments pre-intervention and post-intervention, and every 3-months, for one year. The SERBAS-MOI (Meyer-Bahlburg et al., 1991) was used to assess sexual risk behavior and vaginal episodes equivalent scores were analyzed as the primary outcome. Similar to the results with the SexG-Brief intervention, there was no significant change between the control and experimental group (Berkman et al., 2007). The SexG intervention is not the only HIV risk reduction intervention being conducted in an all-male SMI population, there are two other interventions. One of these is applied an intervention known as Project LIGHT (Living in Good Health Together). This intervention consisted of seven, 90-minute sessions about HIV knowledge, personal risk assessment, risk reduction problem solving skills, condom use skills, assertiveness with sexual partners, strategies for risk reduction, and relapse prevention. The efficacy of Project LIGHT was tested using a RCT, where the control parameter was a one-session video about HIV. The participants 22 completed assessments of four sexual risk behaviors at baseline and at three-month intervals after the intervention for one year. Ninety nine eligible participants were recruited from outpatient mental health clinics in New York City, NY and Los Angeles, CA. Compared to the control group, the intervention group had significantly fewer sexual risk acts at the 12-month follow-up. The most significant benefit of the intervention was seen in the African American participants, who had significant changes in condom use (The National Institute Of Mental Health Multisite HIV Prevention Trial Group, 2006). The other is a two-session intervention that provided HIV knowledge, risk assessment, and condom application skills. In this RCT study 75 males from a psychiatric inpatient unit were assigned to one of four groups: control-individual; control-group; intervention-individual; or intervention-group. The participants completed the “Facts about AIDS” assessment pre-, immediately post-intervention, and two weeks after the intervention. The greatest improvement in HIV knowledge between baseline and posttest was found in the intervention-individual group, where participants had one-on-one interaction with the intervention staff. The authors concluded that the delivery of education, either individually or in a group, was important for the HIV intervention outcomes (Hajagos et al., 1998). Three of the five intervention studies conducted on male participants with SMI to reduce their risk of contracting HIV used variations of SexG. Only the original 15-session SexG intervention (Susser et al., 1998) was successful in reducing the sexual risk behavior of males with SMI, but decreasing trends were noted in the other two studies (Berkman et al., 2006; Berkman et al., 2007). The treatment group in the other intervention known as ProjectLight, also had a significant decrease in the number of risky sexual acts (vaginal or anal intercourse without a condom) as compared to the controls (The National Institute of Mental Health Multisite HIV 23 Prevention Trial Group, 2006). Hajagos and collegues, (1998) did not test reduction in sexual risk behaviors, but individuals in the intervention one-on-one sessions showed increased HIV knowledge in the as compared to the controls. 2.4 FEMALES There were three studies that included just females as participants. The three studies were RCTs using interventions designed to empower females to make safer sex choices. Of these, two used the same intervention known as “Ourselves, Our Bodies, and Our relatives” that included information about the female condom, while the other intervention concentrated primarily on female assertiveness and the use of the male condom to increase HIV prevention behavior. A RCT study designed to increase the sexual assertiveness skills of females recruited 20 female outpatients from a community psychiatric facilities in NY. The females completed ten, 75-minute sessions designed to decrease their HIV behavioral risk by using constructs derived from IMB and social cognitive theory. Assessments were conducted at baseline, post intervention, at a two-month follow-up, and at a four-month follow-up. The assessments included the Sexual Assertiveness Simulation, HIV-Knowledge Questionnaire, Perceived Risk Questionnaire, Behavioral Intentions Questionnaire, and Timeline Follow back Sexual Behavior Interview. Compared with controls, females in the intervention group increased their sexual assertiveness skills, HIV knowledge, and frequency of protected intercourse; the most significant changes were seen at the two-month follow-up (Weinhardt et al., 1998). 24 A RCT design was also used to the 10-session HIV risk reduction intervention, “Ourselves, Our Bodies, Our Realities.” The intervention is 50 minute program based on the social cognitive theory. This study targeted empowerment of SMI females by teaching about female-initiated HIV protection methods including the female condoms and a spermicide (Advantage 24). The participants were 35 females recruited from inpatients from a state hospital in NYC, NY. The control design was a two-session HIV education program. The Subjective Norms of Women-Controlled Methods (SNOW-CM; Geller, n.d.) and the SERBAS were conducted at baseline, post-intervention, and at a six week follow-up. Very limited sexual behavior was reported on the SERBAS; therefore analysis of change in sexual risk behavior could not be determined. Compared to controls, the experimental group had significant changes in attitudes to female condom, at the six week follow-up. Trending but non-significant changes in attitudes were noted for the male condoms (Collins et al., 2001). Another RCT tested the efficacy of the “Ourselves, Our Bodies, and Our relatives,” on 79 females recruited from two transitional living facilities and four day treatment programs in NYC, NY. The SERBAS for mentally ill sheltered women (SERBAS-A-MIS-F; Meyer-Bahlburg et al., 1991) and SNOW-CM (Geller, n.d.) were assessed at baseline, post-intervention and at followup periods. The primary sexual risk behavior outcome was the vaginal episode equivalent (VEE), the number of unprotected oral, vaginal, and anal sexual acts. To evaluate the longevity of the benefits of the intervention, the follow-up period was extended from the six-week period used in the pilot study to three-months and six-months. No significant changes were noted in the sexual risk behavior, VEE scores, between the control and experimental group at pre- and postintervention. When compared with the controls, the significant changes were noted in female 25 condom knowledge, insertion, and use with a partner at 3-month follow-up. Difference in female condom insertion between the two groups, persisted at six-months (Collins et al., 2011). All three of the female only interventions were effect as measured by their respective evaluated outcomes. The initial implementation of “Ourselves, Our Bodies, and Our relatives,” resulted in an increase in positive attitudes towards the use of the female condom in the treatment participants as compared to the controls, but change in sexual behavior could not be assessed due to the limited amount of sexual behavior at baseline (Collins et al., 2001). In the follow-up study, behavior and attitudes were measured (Collins et al., 2001). The treatment females were not only significantly more knowledgeable about female condoms, but they also were more likely to have inserted one and used it with a sexual partner at the three month follow-up. However, the number of times the treatment group had unprotected oral, anal, and vaginal intercourse as compared to the controls did not decrease significantly at the three month follow-up (Collins et al., 2001). Similarly, Weinhardt and colleagues (1998), detected a trending but non-significant decrease in the frequency of unprotected intercourse in the treatment group as compared to the controls. However, this intervention did significantly increase sexual assertiveness, HIV- related knowledge, and protected sex at the two month follow-up. 26 3.0 DISCUSSION The purpose of this literature review examine HIV prevention intervention studies conducted on SMI populations by doing a critical literature review in PubMed and PsychInfo since 1996. Sixteen independent studies were identified; of these studies eight were conducted on mixed gender, five on all male, and three on all female SMI participants. These participants were recruited from different settings including mental health outpatient clinics, inpatient units and other community programs. One major theme emerged from the study results: HIV intervention outcomes varied based on gender. Four other interesting themes emerged: (1) results varied based on race/ethnicity (2) psychiatric diagnosis and (3) efficacy changes based on the “dosage” of the program, and (4) there were several different public health theories used in these studies. Finally, limitations and future directions are discussed. 3.1.1 Differences in the Intervention by Gender After reviewing HIV intervention studies conducted before 1996, Kelly and colleagues (1997) recommended that future researcher studies examine study outcomes to see if there are differences due to gender. Kelly and colleagues (1997) theorized that since females with SMI had different HIV risk profiles than males (e.g. Amaro, 1995; Ickovics & Rodin, 1992; Nyamathi et al., 1993), separate interventions designed specifically for each gender could target these 27 unique HIV risk factors and be more effective. Four (Carey et al., 2004; Kalichman et al., 2005; Otto-Salaj et al., 2001; Williams et al., 2001) of the eight studies (Carey et al., 2004; Kalichman et al., 2005; Otto-Salaj et al., 2001; Williams et al., 2001) (Jordan & Selwyn, 2008; Meyer et al., 1992; Rosenberg et al., 2004; Sikkema et al., 2007) that conducted an intervention using a mixed gender population noted differences in the outcome results between the two genders. In general, when gender differences were reported in differential outcomes, females benefited more than males from the interventions (Carey et al., 2004; Kalichman et al., 2005; Otto-Salaj et al., 2001; Williams et al., 2001), except in one study where males made more significant changes in their HIV prevention behavioral actions, than females (Williams et al., 2001). Effective gender specific interventions had been designed. The original 15-session SexG intervention (Susser et al., 1998) and ProjectLight (The National Institute Of Mental Health Multisite HIV Prevention Trial Group, 2006) were successful in reducing the sexual risk behavior of males with SMI. Another male intervention was successful in increasing HIVrelated knowledge in males with SMI (Hajagos et al., 1998). All three of the interventions designed specifically for females had significant changes in at least one of the HIV-related prevention intervention outcomes that were tested. None of the three interventions significantly decreased the number of unprotected sexual occasions. Two of these interventions educated females about the female condoms; significant changes were noted in the attitudes of the participants in the test group when compared to the controls towards this “safe sex” method (Collins et al., 2001; Collins et al., 2011). In one of the two studies, the participants in the test group increased their use of the female condom with a partner at the threemonth follow-up significantly as when compared to the controls (Collins et al., 2011). Similarly in another study, a significant change in HIV risk behavior (increased frequency of protected 28 intercourse) was noted in the SMI females participants in the test group as compared to the control group (Weinhardt et al., 1998). 3.1.2 Race & Ethnicity The first of three minor findings that emerged was reported in one study where that the results of the intervention varied by race and ethnicity. The study found the most significant benefit of the intervention was seen in African American participants who had significant changes in condom use as compared to Caucasian and Hispanic participants, and participants’ of other races. The study was still effective in the overall group, with significant decreases in the number of unprotected sexual risk acts reported in the participants in the test group as compared to the control group (The National Institute Of Mental Health Multisite HIV Prevention Trial Group, 2006). The difference in condom use among African Americans versus other participants was not observed in a previous study by this group that was conducted in a non SMI population (The National Institute of Mental Health Multisite HIV Prevention Trial Group, 1998). However, the HIV risk factor profile is unique for African American populations (e.g. lifetime history of incarcerations, low social economic status and multiple partners within the same time period (Adimora, Schoenbach, & Floris-Moore, 2009). Researchers have suggested that behavioral interventions for African Americans to reduce sexual risk of HIV should have a culturally relevant design and reflect the unique racial and ethnic attributes of this population (Darbes, Crepaz, Lyles, Kennedy, & Rutherford, 2008; Johnson et al., 2009). An example of a culturally sensitive HIV intervention is Sister to Sister, that specifically targets African American Women (Danya International, 2012). 29 3.1.3 Psychiatric Diagnosis The second minor theme that emerged was from three studies that reported intervention outcomes differences by mental health diagnostic type, but the interventions were still effective in the overall group (Hajagos et al., 1998; Williams et al., 2001; Carey et al., 2004). While the studies varied in reported outcomes, a difference between people diagnosed with schizophrenia and other diagnoses was noted (Hajagos et al., 1998); sometimes the same differences were noted with other psychotic disorders (Williams et al., 2001; Carey et al., 2004). Carey and colleagues (2004) theorized that this difference is due to greater cognitive and social impairment among participants who had a more severe psychotic disorder and suggested that programs be designed tailored to the needs of this subset of SMI individuals and change the delivery format to one-on-one instead of a group format. Indeed, cognitive impairment has been noted among people with SMI (Wykes & Dunn, 1992), especially people with Schizophrenia (Bowie & Harvey, 2005; Elvevåg & Goldberg, 2000; Gur et al., 2007). It has been found to predict long term rehabilitation outcomes; the people with more severe cognitive impairment generally have worse outcomes (McGurk & Mueser, 2004; Wykes & Dunn, 1992). 3.1.4 Dosage of Intervention The final minor theme was that three studies were conducted using the “Sex, Games, and Videotapes” intervention on an all-male population (Berkman et al., 2006; Berkman et al., 2007; Susser et al., 1998). The issue of the intervention’s efficacy versus feasibility of implementation into community mental health settings was explored by this group. Only the study of participants in the intervention with the most sessions (15) had significantly lower sexual risk index scores as 30 measured by the Sexual Risk Behavior Assessment Schedule (SERBAS; Meyer-Bahlburg et al., 1991) than the controls (Susser et al., 1998). This importance of dosage and duration on intervention outcomes in people with SMI has also been found in studies that promote healthy lifestyles for weight loss, where the most effective programs reviewed lasted three months or longer (Bartels & Desilets, 2012). 3.1.5 Theory Primarily two different theories were cited by the authors in their efforts to design these interventions. The Information-Motivation-Behavioral skills (IMB) model (Fisher & Fisher, 1992), was used in three of the 16 studies (Carey et al., 2004; Kalichman et al., 2005; Weinhardt et al., 1998). Nine of the 16 studies used either the Bandura’s Social learning theory (1977) or his later derivative the Social cognitive theory (1986) (Collins et al., 2001; Collins et al., 2011; OttoSalaj et al., 2001; Sikkema et al., 2007; Weinhardt et al., 1998; Berkman et al., 2006; Berkman et al., 2007; Susser et al., 1998; Williams et al., 2001). Three of the studies did not mention a specific theory that was used in their program design (Hajagos et al., 1998; Rosenberg et al., 2004; The National Institute Of Mental Health Multisite HIV Prevention Trial Group, 2006). Many other effective HIV behavioral intervention strategies have been listed at the CDC’s The Diffusion of Effective Behavioral Interventions project (DEBI; Danya International, 2012). Besides using the IMB model (Fisher & Fisher, 1992) and the social learning theory (Bandura, 1977) / social cognitive theory (Bandura, 1986), these interventions use theories like AIDS Risk Reduction Model (Catania et al., 1990) and the Theory of Gender and Power (Connell, 1987) to target HIV risk behavior (Danya International, 2012). Six of the 16 studies either did not test for or did not demonstrate reductions (significant or trending) in HIV related risk behaviors (Jordan 31 & Selwyn, 2008; Meyer et al., 1992; Rosenberg et al., 2004; Berkman et al., 2007; Hajagos et al., 1998; Collins et al., 2001). Therefore the use of more diverse theory driven strategies might be needed to target HIV related risk behaviors in the SMI population. Also in recognition of the heterogeneity of the people that are diagnosed with SMI, an intervention project that has been tried on multiple types of populations (e.g. IV drug users, African Americans, Caucasians, nongay identified men who have sex with men, and female sex workers) and can encompass the convergent and divergent HIV risk factors and behaviors among this heterogeneous population, might be useful to try; one such CDC DEBI program is Peers Reaching Out and Modeling Intervention Strategies. The program uses several behavior change theories to target communitylevel HIV risk behavior change through the use of peer advocates and role model stories (Danya International, 2012). People with SMI can be trained to be peer leaders. Peer advocates were already used in by Sikkema and colleagues (2007) in their intervention, although the efficacy of their involvement as measured by change in peers norms from baseline to follow-up was not established in the small study. Also community mental health peer advocates organizations have been established in this population to combat stigma including the Peer Support and Advocacy Network (n.d.) as well as the Peers Envisioning and Engaging in Recovery Services (PEERS; 2013). 3.1.6 Limitations In this section the limitation of the literature review of HIV prevention interventions conducted on SMI individuals will be presented; they include the lack of a public policy database search, the use of only HIV instead of other sexually transmitted infections (STI) in the search terms, 32 and the types of interventions included in the review. Then the subject inclusion criteria limitations of the research studies will be detailed. 3.1.6.1 Limitations to the literature search The databases, PsychInfo and PubMed, used to search for the HIV intervention studies are not public policy databases. The use of public policy databases might have provided current HIV prevention programming policies that impact feasibility of program implementation. This literature review focused on the prevention of HIV in SMI individuals; therefore it did not include the early intervention studies for people who already have HIV. However, recent attention has been given to the mental health of people with HIV and the interrelationship between HIV and mental health might be complex, dynamic, and reciprocal (e.g. Rabkin, McElhiney, & Ferrando, 2004; Ickovics et al., 2001; Perry, 1994). Lastly, other STIs were not included in the search terms, but people with a history of STIs are more at high risk of HIV than those without (Laga et al., 1993; Wasserheit, 1992). 3.1.6.2 Limitations to the research studies There was one overarching limitation to this body of literature: the varied inclusion criteria for participants. The inclusion criteria that are study limitations are the varied percentage of participants with unhealthy substance use and recruitment of only psychiatric inpatients. Different selection criteria, including unhealthy substance use, were used for the participants in the 16 HIV intervention research studies. Three of the 16 studies included only participants that had both a diagnosis of SMI and unhealthy substance use (Carey et al., 2004; Kalichman et al., 2005; Rosenberg et al., 2004). One of the 16 studies examined and found different outcomes based on the presence or absence of a lifetime history of substance 33 dependence (Berkman et al., 2005) and Carey and colleagues (2004) found that people with SMI assigned to a substance use reduction intervention reported fewer and casual sexual partners than the control group. Substance use, especially IV drug use, is considered to increase HIV risk in the general population (AIDS.gov, 2011) and in the SMI population (Meade & Sikkema, 2005). Four studies of 16 studies used participants who were on psychiatric inpatient units (Collins et al., 2001; Hajagos et al., 1998; Meyer et al., 1992; Williams et al., 2001). Only one of these studies assessed behavioral change by measuring change in action of HIV prevention behaviors (Williams et al., 2001). Due to the small number of females reporting sexual activity in one of these studies behavior change was unable to be assessed (Collins et al., 2001). This limitation was recognized by Collins and colleagues (2001) and in a follow-up study the recruited population was SMI people receiving outpatient services so behavioral changes could be studied (Collins et al., 2011). HIV intervention programs conducted in this setting might need to increase the time of their follow-up assessment, so they can assess these cohorts in outpatient settings. Two of the studies did not evaluate behavior change as part of their objectives (Hajagos et al., 1998; Meyer et al., 1992). 3.1.7 Future Directions In this section future directions for the follow-up literature reviews will be presented. They included: the use of public policy databases for literature searches, the inclusion of other STIs in the search terms, and intervention studies of people who are HIV positive. Subsequently future recommendations for the HIV prevention in SMI field will be presented based on the sixteen studies detailed in this review. There are two major suggestions: (1) tailoring interventions to SMI people with cognitive impairment and (2) designing more interventions for 34 SMI people with unhealthy substance use. Also three other possible directions that include the use of more diverse public health theories in intervention design, testing the association between dosage of intervention sessions and study outcomes and designing interventions that are integrated across multiple different types of mental health facilities. 3.1.7.1 Literature Search Future literature searches could be expanded in several ways. First, databases like Political Science Complete could be used to examine public programing that is available or being planned for HIV prevention in the SMI populations to examine the theoretical and scientific reasoning for these services. Also it could be used to examine the educational programs that are available to train providers to discuss HIV prevention skills with their patients with SMI, as this is an important issue if the eventual goal is sustainable implementation of HIV prevention programming at psychiatric hospitals and community mental health facilities. The relationship between HIV and mental health could be further explored by including HIV intervention studies that target mental health symptom management to improve quality of life for participants. Lastly, studies of prevention of other STIs in SMI populations could be included. 3.1.7.2 HIV Prevention Studies HIV prevention research could be improved in several ways. Since three studies reported intervention outcomes differences by mental health diagnostic type (Hajagos et al., 1998; Williams et al., 2001; Carey et al., 2004) and greater cognitive and social impairment among people with a more severe psychotic disorder has been known to predict long term rehabilitation outcomes (Wykes & Dunn, 1992), future studies could explore different ways to tailor the HIV prevention to this subpopulation by doing formative research before implementation. 35 Collaborations between HIV prevention and cognitive remediation (i.e. through Cognitive Enhancement Therapy; Eack, 2012) researchers working with this population could facilitate designing more appropriate HIV intervention programing. Since the highest rate of HIV infection was found in a study of people with SMI and unhealthy substance use (Silberstein et al., 1994) and substance use has been identified as a risk factor for HIV infection in SMI people (Meade & Sikkema, 2005), this subpopulation could benefit from more targeted HIV interventions,. Individuals with SMI who have unhealthy substance use might require HIV intervention programs that are different than the people with only a SMI, and possibly require an integrated programing to reduce both substance use and HIV risk behaviors. The CDC (2002) has made the recommendation that “HIV Prevention Should be an Integral Component of Substance Abuse Treatment” (CDC, 2002, p.1) for IV drug users in the general public, but also recognized the challenges it presents (e.g. lack of access, shortage of well trained staff, and continued drug use). A study by Solomon and colleagues (2007) found that HIV case managers in a community mental health center, that services people with SMI and unhealthy substance use and other individuals, received basic sexually transmitted disease training, but had no formal training on teaching HIV prevention to their consumers. To help with this issue, Solomon and colleagues are conducting an intervention where the case managers are trained to deliver an HIV prevention intervention to people with SMI and unhealthy substance use. At this writing, it is unknown if the results of the intervention have been published. However, focus group data of the case managers revealed a change in their perceived attitudes’ towards the mental health consumers, most notably they recognized that their consumers were having sex, and their own HIV prevention skills (Tennille, Solomon, & Blank, 2010). The results of the study by Solomon and colleagues (2007) will provide more information about the 36 relationship between substance use, SMI and HIV prevention. Since almost a third of people with SMI have a co-occurring substance abuse issue, further HIV intervention studies tailored to this subpopulation are warranted (Regier et al., 1990). Besides tailoring programming to subpopulations of people with SMI, there are other areas that could be further explored in this field. More diverse public health theories could be used to design interventions for people with SMI to target HIV risk behavior. Also the issue of feasibility versus efficacy of a HIV intervention program could be explored by randomly assigning participants to different number of sessions (i.e. dosage) to see the impact it has on study outcomes. Another is changing study recruitment, such as using outpatient or community participants, to increase the chances that the HIV intervention studies are able to demonstrate significant HIV risk reduction behavior change. This is suggested because only one of the four studies who recruited participants from psychiatric inpatient units was able to assess change in HIV behavioral outcomes (Collins et al., 2001; Hajagos et al., 1998; Meyer et al., 1992; Williams et al., 2001). Like Kelly (1997), a more mental health system-level approach to HIV prevention for people with SMI may be beneficial. The interventions studies in this review have conducted in psychiatric inpatient units (Collins et al., 2001; Williams et al., 2001; Meyer et al., 1992) mental health facilities providing outpatients services (Collins et al., 2011; Weinhardt et al., 1998; Berkman et al., 2007; Carey et al., 2004; The National Institute Of Mental Health Multisite HIV Prevention Trial Group, 2006; Kalichman et al., 2005; Otto-Salaj et al., 2001; Rosenberg et al., 2004) and places within the community programs that people with SMI utilize (Berkman et al., 2006; Collins et al., 2011; Jordan & Selwyn, 2008; Sikkema et al., 2007; Susser et al., 1998). However, none of the studies used an integrated approach where multiple different types of 37 facilities were involved, such as an inpatient hospital and outpatient facilities. This integrated approach to expansion of HIV interventions to multiple different types of mental health facilities could eventually lead to a more complex, broadly encompassing social ecological perspective approach to targeting HIV risk in the SMI population. The social ecological approach promotes behavioral HIV change at several levels: Individual, interpersonal, community and structural and environmental; suggested approaches to designing and implementing this type of HIV prevention intervention exist (Latkin & Knowlton, 2005; Moore et al., 2010; Weeks et al., 2009). 3.1.8 Conclusions Studies have found that people with SMI have a higher HIV prevalence than the general population (Cournos & McKinnon, 1997). To learn more about the HIV prevention interventions that are designed for this HIV high risk population, a literature search was conducted in PsychInfo and PubMed. Sixteen intervention studies that meet inclusion and exclusion criteria were found. A critical examination of these studies revealed that HIV prevention interventions can change HIV related attitudes and risk behavior. The HIV prevention studies in this review combined education and behavioral skills activities, which has been found to be an effective way to promote behavior change in the SMI population in another health promotion subject (Bartels & Desilets, 2012). HIV intervention prevention programs conducted with SMI individuals is a fledgling field, but advances (e.g. more RCT designed studies, larger samples, longer follow-up periods) have been made in the field since the Kelly (1997) critically reviewed the available studies and made recommendations for future directions. The greatest change has occurred in the design of gender specific interventions; previously there were no specific programs available for females (Kelly, 1997). 38 A future area of improvement is based on changes in the study outcomes due to psychiatric diagnosis noted in three of the studies (Hajagos et al., 1998; Williams et al., 2001; Carey et al., 2004) and presence unhealthy substance use noted in one study (Berkman et al., 2005) these interventions appear to still need further development in designing specific HIV educational programing for SMI subpopulation. Further research on these subpopulations and specifically tailored programming is recommended to decrease the HIV risk behavior in the SMI population. Like Kelly (1997), a more mental health system-level approach to HIV prevention for people with SMI may be beneficial, with the eventual goal being a design and implementation of an social ecological approach to HIV prevention (Latkin & Knowlton, 2005; Moore et al., 2010; Weeks et al., 2009). High risk for HIV infection is public health issue for people with SMI, while interventions have been developed that effectively change HIV risk related behaviors in this population, the heterogeneity of the subjects continues to impact outcomes and the HIV risk reduction needs of this diverse individuals are still not completely met. , 39 APPENDIX: TABLE Table 1. Intervention Studies Study Name of Intervention (Jordan & Selwyn, 2008) (Meyer et al., 1992) (Williams et al., 2001) (Otto-Salaj et al., 2001; Pinkerton et al., 2001) RCT (YES/No) Gend er Sample# No M/F No M/F Criteria (Besides SMI) Theory Main Findings 7 Not provided Knowledge and self-efficacy scores increased from pre- to post intervention (statistical significance not established). 12 Health Belief Model (Rosenstock et al., 1988) The mean scores of the AIDs Knowledge Questionnaire improved from pre- to post intervention (Statistical Significance not established). Social Learning Theory (Bandura, 1977) and Transtheoretical Model of Behavior Change (Prochaska et al., 1992) Significant changes in scores from pre- to post intervention were found in the domain of: precontemplation for females, action for males, contemplation for patients diagnosed with a psychotic disorder, and action of those with a mood disorder. Social Cognitive Theory (Bandura, 1986) The intervention was associated with significant change in HIV risk knowledge scores between baseline and 3-,6-,and 9-month follow-up for males and attitudes toward condom use, risk reduction behavioral intentions, and sexual behavior between baseline and 3-, 6-, and 9month follow-up for females. 50 Facts for Life No M/F (32M, 18F ) Yes M/F 189 (87M, 102F) 40 Table 1 Continued (Carey et al., 2004) (Rosenberg et al., 2004) HIV-riskreduction intervention (HIV-R) Yes M/F 408 (187M, 221F) substance use in the past 12 months Information-motivationbehavioral skills theory ((Fisher & Fisher, 1992). The HIV intervention (HIV-R) was associated with significant decreases in the occasions of unprotected vaginal sex and the number of sexual partners. Also, significant increases in communication skills regarding safer sex with a partner, HIV knowledge, positive condom attitudes, condom use intentions, and behavioral skills. The HIV-R group reported fewer new STIs than the control group. Screen, test, immunize, reduce risk, and refer (STIRR) No M/F 50 unhealthy substance use diagnosis Medical model The intervention was associated with significant increases in HIV knowledge and motivation to reduce HIV risk behaviors. 320 (150M, 170F) could not be HIV positive; receiving treatment for unhealthy substance abuse Information-motivationbehavioral skills theory (Fisher &Fisher, 1992) The intervention was associated with significant change in HIV knowledge scores between baseline and the 6-month follow-up for men and changes in condom attitudes, risk reduction behavioral intentions, and reported reductions in sexual risk behaviors between baseline and 6month follow-up for women. Social Cognitive Theory (Bandura, 1986) Participants reported significant increases in condom use, sexual communication, positive attitudes towards condom use, and behavioral intentions were observed after the skills training intervention (with and without the social norms part of the intervention). Participants reported significant increases in HIV knowledge only after both the skills training and social norms intervention. (Kalichman et al., 2005) No (Sikkema et al., 2007) No M/F M/F 28 (17M, 11F) (Susser et al., 1998; Berkman et al., 2005) “Sex, Games, and Videotapes” (SexG) Yes M 97; 59 sexually active homeless Social Learning Theory (Bandura, 1977) The intervention was associated with significantly lower sexual risk index scores at the 6-month follow-up. When compared to the controls, no significant HIV risk reduction was found in the substance-dependent men. (Berkman et al., 2006) SexG-Brief. Yes M 92; 56 sexually active homeless Social Learning Theory (Bandura, 1977) The intervention was not associated with any significant changes in HIV risk behaviors, although a decreasing trend was noted. 41 Table 1 Continued (Berkman et al., 2007) Enhanced SexG (E-SexG) (The National Institute Of Mental Health Multisite HIV Prevention Trial Group, 2006) Project LIGHT (Living in Good Health Together) (Hajagos et al., 1998) (Collins et al., 2011). Yes Yes (Weinhardt et al., 1998) (Collins et al., 2001) Yes Yes “Ourselves, Our Bodies, Our Realities.” “Ourselves, Our Bodies, and Our Realities.” Yes Yes M M M F F F 149 Social Learning Theory (Bandura, 1977) The intervention was not associated with any significant changes in HIV risk behaviors. 99 Combined (Cognitive behavioral theory, theory of reasoned action, and HIV specific theories) The intervention group had significantly fewer sexual risk acts at the 12-month follow-up than the control 75 No theory Participants in the individually delivered intervention group had the most significant improvement in HIV knowledge between baseline and posttest. 30 Information-motivationbehavioral skills theory (Fisher &Fisher, 1992) and Social Cognitive Theory (Bandura, 1986) The intervention was associated with significant increases in sexual assertiveness skills, HIV knowledge, and frequency of protected intercourse; the most significant changes were seen at the 2-month follow-up. Social Cognitive Theory (Bandura, 1986) The intervention was associated with significant increases in positive attitudes towards female and male condoms, but not the Advantage 24, from the baseline to 6 week follow-up. Social Cognitive Theory (Bandura, 1986) The intervention was associated with significant increases in female condom knowledge, insertion, and use with a partner from the baseline to 3-month follow-up. No significant changes were noted in the sexual risk behavior (unprotected sexual acts). HIV negative 35 79 42 BIBLIOGRAPHY Adimora, A. A., Schoenbach, V. J., & Floris-Moore, M. A. (2009). Ending the epidemic of heterosexual HIV transmission among African Americans. Am J Prev Med, 37(5), 468471. doi: 10.1016/j.amepre.2009.06.020 AIDS.gov. (2011). Substance Use/Abuse. Retrieved May 10th, 2013, from http://aids.gov/hivaids-basics/prevention/reduce-your-risk/substance-abuse-use/ Amaro, H. (1995). Love, sex, and power. Considering women's realities in HIV prevention. Am Psychol, 50(6), 437-447. American Psychiatric Association. (1987). Diagnostic and Statistical Manual of Mental Disorders (3rd edn, revised) (DSM-III-R). Washington, DC:. American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: American Psychiatric Association. AVERT. History of AIDS up to 1986. HIV and AIDS Topics. Retrieved March, 26, 2013 AVERT. (2013). History of AIDS up to 1986. HIV and AIDS Topics. Retrieved March, 26, 2013, from http://www.avert.org/aids-history-86.htm Bandura, A. (1977). Social Learning Theory. Morristown, N.J: General Learning Press. Bandura, A. (1986). Social Foundations of Thought and Action: A Social Cognitive Theory Englewood Cliffs, N.J: Prentice-Hall. Bartels, S., & Desilets, R. (2012). Health Promotion Programs for People with Serious Mental Illness (Prepared by the Dartmouth Health Promotion Research Team). Washington, D.C. : Retrieved from http://www.integration.samhsa.gov/Health_Promotion_White_Paper_Bartels_Final_Doc ument.pdf. Berkman, A., Cerwonka, E., Sohler, N., & Susser, E. (2006). A randomized trial of a brief HIV risk reduction intervention for men with severe mental illness. Psychiatric Services, 57(3), 407-409. doi: 10.1176/appi.ps.57.3.407 Berkman, A., Pilowsky, D. J., Zybert, P. A., Herman, D. B., Conover, S., Lemelle, S., . . . Susser, E. (2007). HIV prevention with severely mentally ill men: A randomised controlled trial. Aids Care-Psychological and Socio-Medical Aspects of Aids/Hiv, 19(5). doi: 10.1080/09540120701213989 Berkman, A., Pilowsky, D. J., Zybert, P. A., Leu, C. S., Sohler, N., & Susser, E. (2005). The impact of substance dependence on HIV sexual risk-reduction among men with severe mental illness. AIDS Care, 17(5), 635-639. doi: 10.1080/09540120412331291797 Bowie, C. R., & Harvey, P. D. (2005). Cognition in schizophrenia: impairments, determinants, and functional importance. Psychiatr Clin North Am, 28(3), 613-633, 626. doi: 10.1016/j.psc.2005.05.004 43 Brunette, M. F., Rosenberg, S. D., Goodman, L. A., Mueser, K. T., Osher, F. C., Vidaver, R., . . . Drake, R. E. (1999). HIV risk factors among people with severe mental illness in urban and rural areas. Psychiatr Serv, 50(4), 556-558. Carey, M. P., Carey, K. B., Maisto, S. A., Gleason, J. R., Gordon, C. M., & Brewer, K. K. (1999). HIV Risk Behavior among Outpatients at a State Psychiatric Hospital: Prevalence and Risk Modeling. Behav Ther, 30(3), 389-406. doi: 10.1016/S0005-7894(99)80017-3 Carey, M. P., Carey, K. B., Maisto, S. A., Gordon, C. M., Schroder, K. E. E., & Vanable, P. A. (2004). Reducing HIV-risk behavior among adults receiving outpatient psychiatric treatment: Results from a randomized controlled trial. Journal of Consulting and Clinical Psychology, 72(2). doi: 10.1037/0022-006x.72.2.252 Carey, M. P., Carey, K. B., Maisto, S. A., Gordon, C. M., & Vanable, P. A. (2001). Prevalence and correlates of sexual activity and HIV-related risk behavior among psychiatric outpatients. J Consult Clin Psychol, 69(5), 846-850. Carey, M. P., Carey, K. B., Weinhardt, L. S., & Gordon, C. M. (1997). Behavioral risk for HIV infection among adults with a severe and persistent mental illness: patterns and psychological antecedents. Community Ment Health J, 33(2), 133-142. Catania, J. A., Kegeles, S. M., & Coates, T. J. (1990). Towards an understanding of risk behavior: an AIDS risk reduction model (ARRM). Health Educ Q, 17(1), 53-72. CDC. (2002). LINKING HIV PREVENTION SERVICES AND SUBSTANCE ABUSE TREATMENT PROGRAMS Retrieved from http://www.cdc.gov/idu/facts/HIVPrevServFin.pdf. CDC. (2011). HIV Surveillance Report, Volume 23. Table 17 A. Retrieved June 07, 2012, from http://www.cdc.gov/hiv/library/reports/surveillance/2011/surveillance_Report_vol_23.ht ml CDC. (2012). Basic Information about HIV and AIDS. Retrieved April 12, 2012, from http://www.cdc.gov/hiv/topics/basic/index.htm#hiv Chawarski, M. C., Pakes, J., & Schottenfeld, R. S. (1998). Assessment of HIV risk. J Addict Dis, 17(4), 49-59. doi: 10.1300/J069v17n04_05 Collins, P. Y., Geller, P. A., Miller, S., Toro, P., & Susser, E. S. (2001). Ourselves, our bodies, our realities: An HIV prevention intervention for women with severe mental illness. Journal of Urban Health-Bulletin of the New York Academy of Medicine, 78(1). doi: 10.1093/jurban/78.1.162 Collins, P. Y., von Unger, H., Putnins, S., Crawford, N., Dutt, R., & Hoffer, M. (2011). Adding the Female Condom to HIV Prevention Interventions for Women with Severe Mental Illness: A Pilot Test. Community Mental Health Journal, 47(2), 143-155. doi: 10.1007/s10597-010-9302-8 Connell, R. W. (1987). Gender and Power. Stanford, California: Stanford University Press. Cournos, F., Guido, J. R., Coomaraswamy, S., Meyer-Bahlburg, H., Sugden, R., & Horwath, E. (1994). Sexual activity and risk of HIV infection among patients with schizophrenia. Am J Psychiatry, 151(2), 228-232. Cournos, F., & McKinnon, K. (1997). HIV seroprevalence among people with severe mental illness in the United States: a critical review. Clin Psychol Rev, 17(3), 259-269. Danya International, I. (2012). Effective Interventions: HIV Prevention that works. Retrieved May 10th, 2013, from http://www.effectiveinterventions.org/en/HighImpactPrevention/Interventions.aspx 44 Darbes, L., Crepaz, N., Lyles, C., Kennedy, G., & Rutherford, G. (2008). The efficacy of behavioral interventions in reducing HIV risk behaviors and incident sexually transmitted diseases in heterosexual African Americans. AIDS, 22(10), 1177-1194. doi: 10.1097/QAD.0b013e3282ff624e Eack, S. M. (2012). Cognitive remediation: a new generation of psychosocial interventions for people with schizophrenia. Soc Work, 57(3), 235-246. Elvevåg, B., & Goldberg, T. E. (2000). Cognitive impairment in schizophrenia is the core of the disorder. Crit Rev Neurobiol, 14(1), 1-21. First, M., M, G., RL, S., Williams, J., & LS., B. (1997). Structured Clinical Interview for DSMIV Axis II Personality Disorders, (SCID-II). Washington, D.C: American Psychiatric Press, Inc. Fishbein, M., & Ajzen, I. (1975). Belief, Attitude, Intention, and Behavior: An Introduction to Theory and Research. . Reading, MA: Addison-Wesley. Fisher, J. D., & Fisher, W. A. (1992). Changing AIDS-risk behavior. Psychol Bull, 111(3), 455474. Geller, P. (n.d.). Use of female-controlled HIV prevention methods among women with mental illness. Columbia University and the New York State Psychiatric Institute. Glanz, K., Rimer, B., Viswanath, K. (2008). Health Behavior and Health Education: Theory, Research, and Practice (4 ed.). San Francisco, CA: Jossey-Bass. Grassi, L., Pavanati, M., Cardelli, R., Ferri, S., & Peron, L. (1999). HIV-risk behaviour and knowledge about HIV/AIDS among patients with schizophrenia. Psychol Med, 29(1), 171-179. Gur, R. E., Nimgaonkar, V. L., Almasy, L., Calkins, M. E., Ragland, J. D., Pogue-Geile, M. F., . . . Gur, R. C. (2007). Neurocognitive endophenotypes in a multiplex multigenerational family study of schizophrenia. Am J Psychiatry, 164(5), 813-819. doi: 10.1176/appi.ajp.164.5.813 Hajagos, K., Geiser, P., Parker, B., & Tesfa, A. (1998). Safer-sex education for persons with mental illness. J Psychosoc Nurs Ment Health Serv, 36(8), 33-37. Holtgrave, D. R., Qualls, N. L., Curran, J. W., Valdiserri, R. O., Guinan, M. E., & Parra, W. C. (1995). An overview of the effectiveness and efficiency of HIV prevention programs. Public Health Rep, 110(2), 134-146. Horwath, E., Cournos, F., McKinnon, K., Guido, J. R., & Herman, R. (1996). Illicit-drug injection among psychiatric patients without a primary substance use disorder. Psychiatr Serv, 47(2), 181-185. Ickovics, J. R., Hamburger, M. E., Vlahov, D., Schoenbaum, E. E., Schuman, P., Boland, R. J., . . . Group, H. E. R. S. (2001). Mortality, CD4 cell count decline, and depressive symptoms among HIV-seropositive women: longitudinal analysis from the HIV Epidemiology Research Study. JAMA, 285(11), 1466-1474. Ickovics, J. R., & Rodin, J. (1992). Women and AIDS in the United States: epidemiology, natural history, and mediating mechanisms. Health Psychol, 11(1), 1-16. Jacobs, J., Jones, E., Gabella, B., Spring, B., & Brownson, R. (2012). Tools for Implementing an Evidence-Based Approach in Public Health Practice. . Preventing Chronic Disease. Johnson, B. T., Scott-Sheldon, L. A., Smoak, N. D., Lacroix, J. M., Anderson, J. R., & Carey, M. P. (2009). Behavioral interventions for African Americans to reduce sexual risk of HIV: a meta-analysis of randomized controlled trials. J Acquir Immune Defic Syndr, 51(4), 492501. doi: 10.1097/QAI.0b013e3181a28121 45 Jordan, W. B., & Selwyn, P. A. (2008). HIV prevention in the clubhouse. Psychiatric Services, 59(8). doi: 10.1176/appi.ps.59.8.933 Kalichman, S., Malow, R., Devieux, J., Stein, J. A., & Piedman, F. (2005). HIV risk reduction for substance using seriously mentally ill adults: Test of the information-motivationbehavior skills (IMB) model. Community Mental Health Journal, 41(3). doi: 10.1007/s10597-005-5002-1 Kalichman, S. C., Kelly, J. A., Johnson, J. R., & Bulto, M. (1994). Factors associated with risk for HIV infection among chronic mentally ill adults. Am J Psychiatry, 151(2), 221-227. Kalichman, S. C., Sikkema, K. J., Kelly, J. A., & Bulto, M. (1995). Use of a brief behavioral skills intervention to prevent HIV infection among chronic mentally ill adults. Psychiatr Serv, 46(3), 275-280. Kelly, J. A. (1997). HIV risk reduction interventions for persons with severe mental illness. Clinical Psychology Review, 17(3). doi: 10.1016/s0272-7358(97)00020-2 Kelly, J. A., McAuliffe, T. L., Sikkema, K., Murphy, D. A., Somlai, A. M., Mulry, G., . . . Fernandez, M. (1996). “Practicing what you preach’? HIV risk reduction behavior changes afier teachingsmerely mentally ill adults to advocate AIDS prevention to peers. Medical College of Wisconsin. Unpublished manuscript. Kelly, J. A., Murphy, D. A., Bahr, G. R., Brasfield, T. L., Davis, D. R., Hauth, A. C., . . . Eilers, M. K. (1992). AIDS/HIV risk behavior among the chronic mentally ill. Am J Psychiatry, 149(7), 886-889. Kelly, J. A., Murphy, D. A., Sikkema, K. J., Somlai, A. M., Mulry, G. W., Fernandez, M. I., . . . Stevenson, L. Y. (1995). Predictors of high and low levels of HIV risk behavior among adults with chronic mental illness. Psychiatr Serv, 46(8), 813-818. Kessler, R. C., Berglund, P. A., Zhao, S., Leaf, P. J., Kouzis, A. C., Bruce, M. L., et al. (1996). The 12-month prevalence andcorrelates of serious mental illness. . Washington, DC: US Government Printing Office. Laga, M., Manoka, A., Kivuvu, M., Malele, B., Tuliza, M., Nzila, N., . . . Alary, M. (1993). Nonulcerative sexually transmitted diseases as risk factors for HIV-1 transmission in women: results from a cohort study. AIDS, 7(1), 95-102. Latkin, C. A., & Knowlton, A. R. (2005). Micro-social structural approaches to HIV prevention: a social ecological perspective. AIDS Care, 17 Suppl 1, S102-113. doi: 10.1080/09540120500121185 Lyles, C. M., Kay, L. S., Crepaz, N., Herbst, J. H., Passin, W. F., Kim, A. S., . . . Team, H. A. P. R. S. (2007). Best-evidence interventions: Findings from a systematic review of HIV behavioral interventions for US populations at high risk, 2000-2004. American Journal of Public Health, 97(1). doi: 10.2105/ajph.2005.076182 McConnaughy, E. A., DiClemente, C. C., Prochaska, J. O., & Velicer, W. F. (1989). Stages of change in psychotherapy: A follow-up report. Psychtherapy, 26, 494-503. McDermott, B. E., Sautter, F. J., Winstead, D. K., & Quirk, T. (1994). Diagnosis, health beliefs, and risk of HIV infection in psychiatric patients. Hosp Community Psychiatry, 45(6), 580-585. McGurk, S. R., & Mueser, K. T. (2004). Cognitive functioning, symptoms, and work in supported employment: a review and heuristic model. Schizophr Res, 70(2-3), 147-173. doi: 10.1016/j.schres.2004.01.009 46 McKinnon, K., Cournos, F., Sugden, R., Guido, J. R., & Herman, R. (1996). The relative contributions of psychiatric symptoms and AIDS knowledge to HIV risk behaviors among people with severe mental illness. J Clin Psychiatry, 57(11), 506-513. Meade, C. S., & Sikkema, K. J. (2005). HIV risk behavior among adults with severe mental illness: A systematic review. Clinical Psychology Review, 25(4). doi: 10.1016/j.cpr.2005.02.001 Meyer, I., Cournos, F., Empfield, M., Agosin, B., & Floyd, P. (1992). HIV prevention among psychiatric inpatients: A pilot study risk reduction study. Psychiatric Quarterly (New York), 63(2). doi: 10.1007/bf01065989 Meyer, I., McKinnon, K., Cournos, F., Empfield, M., Bavli, S., Engel, D., & Weinstock, A. (1993). HIV seroprevalence among long-stay patients in a state psychiatric hospital. Hosp Community Psychiatry, 44(3), 282-284. Meyer-Bahlburg, H., Ehrhardt, A., Exner, T., & Gruen, R. (1991). Sexual Risk Behavior Assessment Schedule-Adult Armory Interview (SERBAS-A-ARMM-1). Programof Developmental Psychoendocrinology. New York State Psychiatric Institute and Department of Psychiatry, College of Physicians and Surgeons of Columbia. New York, NY. Meyer-Bahlburg, H., Ehrhardt, A., Exner, T. M., & Gruen, R. S. (1991). Sexual Risk Behavior Assessment Schedule Adult Armory Interview. . New York: New York State Psychiatric Institute and Columbia University. Moore, D., Carr, C. A., Williams, C., Richlen, W., Huber, M., & Wagner, J. (2010). An ecological approach to addressing HIV/AIDS in the African American community. J Evid Based Soc Work, 7(1), 144-161. doi: 10.1080/15433710903176047 National Institute of Mental Health. (1987). Towards a Model for a Comprehensive CommunityBased Mental Health System. . Washington, DC. National Institute of Mental Health. (1993). AIDS research: An NIMH blueprint for the second decade. . Rockville MD: U.S. Dept. of Health and Human Services, Public Health Service, National Institutes of Health, National Institute of Mental Health. National Institute of Mental Health. (2012). Division of AIDS Research (DAR). Retrieved March 26, 2013, from http://www.nimh.nih.gov/about/organization/dar/index.shtml Nyamathi, A., Bennett, C., Leake, B., Lewis, C., & Flaskerud, J. (1993). AIDS-related knowledge, perceptions, and behaviors among impoverished minority women. Am J Public Health, 83(1), 65-71. Otto-Salaj, L. L., Kelly, J. A., Stevenson, L. Y., Hoffmann, R., & Kalichman, S. C. (2001). Outcomes of a randomized small-group HIV prevention intervention trial for people with serious mental illness. Community Mental Health Journal, 37(2). Parabiaghi, A., Bonetto, C., Ruggeri, M., Lasalvia, A., & Leese, M. (2006). Severe and persistent mental illness: a useful definition for prioritizing community-based mental health service interventions. Soc Psychiatry Psychiatr Epidemiol, 41(6), 457-463. doi: 10.1007/s00127006-0048-0 Peer Support and Advocacy Network's. (n.d.). Retrieved May 10th, 2013, from http://www.peer-support.org/index.html Peers Envisioning and Engaging in Recovery Services (PEERS). (2013). Retrieved May 10th, 2013, from http://www.peersnet.org/ Perry, S. W. (1994). HIV-related depression. Res Publ Assoc Res Nerv Ment Dis, 72, 223-238. 47 Pinkerton, S. D., Johnson-Masotti, A. P., Otto-Salaj, L. L., Stevenson, L. Y., & Hoffmann, R. G. (2001). Cost-effectiveness of an HIV prevention intervention for mentally ill adults. Mental health services research, 3(1). doi: 10.1023/a:1010112619165 Prochaska, J. O., DiClemente, C. C., & Norcross, J. C. (1992). In search of how people change. Applications to addictive behaviors. Am Psychol, 47(9), 1102-1114. Rabkin, J. G., McElhiney, M. C., & Ferrando, S. J. (2004). Mood and substance use disorders in older adults with HIV/AIDS: methodological issues and preliminary evidence. AIDS, 18 Suppl 1, S43-48. Regier, D. A., Farmer, M. E., Rae, D. S., Locke, B. Z., Keith, S. J., Judd, L. L., & Goodwin, F. K. (1990). Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA, 264(19), 2511-2518. Rosenberg, S., Brunette, M., Oxman, T., Marsh, B., Dietrich, A., Mueser, K., . . . Vidaver, R. (2004). The STIRR model of best practices for blood-borne diseases among clients with serious mental illness. Psychiatric Services, 55(6). doi: 10.1176/appi.ps.55.6.660 Rosenberg, S. D., Trumbetta, S. L., Mueser, K. T., Goodman, L. A., Osher, F. C., Vidaver, R. M., & Metzger, D. S. (2001). Determinants of risk behavior for human immunodeficiency virus/acquired immunodeficiency syndrome in people with severe mental illness. Compr Psychiatry, 42(4), 263-271. doi: 10.1053/comp.2001.24576 Rosenstock, I. M., Strecher, V. J., & Becker, M. H. (1988). Social learning theory and the Health Belief Model. Health Educ Q, 15(2), 175-183. Ruggeri, M., Leese, M., Thornicroft, G., Bisoffi, G., & Tansella, M. (2000). Definition and prevalence of severe and persistent mental illness. Br J Psychiatry, 177, 149-155. Sacks, M., Dermatis, H., Looser-Ott, S., Burton, W., & Perry, S. (1992). Undetected HIV infection among acutely ill psychiatric inpatients. Am J Psychiatry, 149(4), 544-545. Sacks, M. H., Perry, S., Graver, R., Shindledecker, R., & Hall, S. (1990). Self-reported HIVrelated risk behaviors in acute psychiatric inpatients: a pilot study. Hosp Community Psychiatry, 41(11), 1253-1255. SAMHSA. (2011). Mental Illness and Homelessness. http://homeless.samhsa.gov/ResourceFiles/hrc_factsheet.pdf. Sikkema, K. J., Meade, C. S., Doughty-Berry, J. D., Zimmerman, S. O., Kloos, B., & Snow, D. L. (2007). Community-level HIV prevention for persons with severe mental illness living in supportive housing programs: a pilot intervention study. Journal of prevention & intervention in the community, 33(1-2). doi: 10.1300/J005v33n01_10 Silberstein, C., Galanter, M., Marmor, M., Lifshutz, H., Krasinski, K., & Franco, H. (1994). HIV-1 among inner city dually diagnosed inpatients. Am J Drug Alcohol Abuse, 20(1), 101-113. Solomon, P. L., Tennille, J. A., Lipsitt, D., Plumb, E., Metzger, D., & Blank, M. B. (2007). Rapid assessment of existing HIV prevention programming in a community mental health center. J Prev Interv Community, 33(1-2), 137-151. doi: 10.1300/J005v33n01_11 Susser, E., Valencia, E., Berkman, A., Sohler, N., Conover, S., Torres, J., . . . Miller, S. (1996). HIV sexual risk reduction in impaired populations: A controlled trial among homeless men. . Columbia University, New York, NY. Susser, E., Valencia, E., Berkman, A., Sohler, N., Conover, S., Torres, J., . . . Miller, S. (1998). Human immunodeficiency virus sexual risk reduction in homeless men with mental illness. Archives of General Psychiatry, 55(3). doi: 10.1001/archpsyc.55.3.266 48 Susser, E., Valencia, E., & Conover, S. (1993). Prevalence of HIV infection among psychiatric patients in a New York City men's shelter. Am J Public Health, 83(4), 568-570. Tengs, T. O., Adams, M. E., Pliskin, J. S., Safran, D. G., Siegel, J. E., Weinstein, M. C., & Graham, J. D. (1995). Five-hundred life-saving interventions and their cost-effectiveness. Risk Anal, 15(3), 369-390. Tennille, J., Solomon, P., & Blank, M. (2010). Case managers discovering what recovery means through an HIV prevention intervention. Community Ment Health J, 46(5), 486-493. doi: 10.1007/s10597-010-9326-0 The National Institute Of Mental Health Multisite HIV Prevention Trial Group. (2006). HIV prevention with persons with mental health problems. Psychol Health Med, 11(2), 142154. doi: K26X82157260164Q [pii] 10.1080/13548500500445094. The NIMH Multisite HIV Prevention Trial: reducing HIV sexual risk behavior. The National Institute of Mental Health (NIMH) Multisite HIV Prevention Trial Group. (1998). Science, 280(5371), 1889-1894. The White House. (2010). NATIONAL HIV/AIDS STRATEGY. The World Bank. (2011). Prevalence of HIV, total (% of population ages 15-49). Traube, D. E., Holloway, I. W., & Smith, L. (2011). Theory development for HIV behavioral health: empirical validation of behavior health models specific to HIV risk. AIDS Care, 23(6), 663-670. doi: 10.1080/09540121.2010.532532 Wallace, C. J., Liberman, R. P., MacKain, S. J., Blackwell, G., & Eckman, T. A. (1992). Effectiveness and replicability of modules for teaching social and instrumental skills to the severely mentally ill. Am J Psychiatry, 149(5), 654-658. Washington State Department of Health. (n.d). Theories and Models. Retrieved December, 20, 2012, from http://www.doh.wa.gov/YouandYourFamily/IllnessandDisease/HIVAIDS/Prevention/Int erventions/TheoriesandModels.aspx Wasserheit, J. N. (1992). Epidemiological synergy. Interrelationships between human immunodeficiency virus infection and other sexually transmitted diseases. Sex Transm Dis, 19(2), 61-77. Weeks, M. R., Convey, M., Dickson-Gomez, J., Li, J., Radda, K., Martinez, M., & Robles, E. (2009). Changing drug users' risk environments: peer health advocates as multi-level community change agents. Am J Community Psychol, 43(3-4), 330-344. doi: 10.1007/s10464-009-9234-z Weinhardt, L. S., Carey, M. P., Carey, K. B., & Verdecias, R. N. (1998). Increasing assertiveness skills to reduce HIV risk among women living with a severe and persistent mental illness. Journal of Consulting and Clinical Psychology, 66(4). doi: 10.1037/0022-006x.66.4.680 Williams, E., Donnelly, J., & Proesher, E. (2001). An HIV/AIDS risk-reduction program for mentally ill hospital patients: Assessing readiness for change. American Journal of Orthopsychiatry, 71(3). doi: 10.1037/0002-9432.71.3.385 Wykes, T., & Dunn, G. (1992). Cognitive deficit and the prediction of rehabilitation success in a chronic psychiatric group. Psychol Med, 22(2), 389-398. 49