ELECTRONIC CIGARETTES COULD SAVE AMERICA: A REVIEW ON ELECTRONIC NICOTINE
advertisement

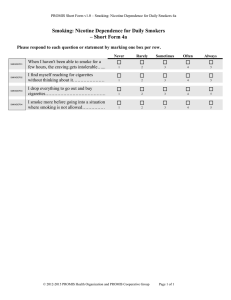
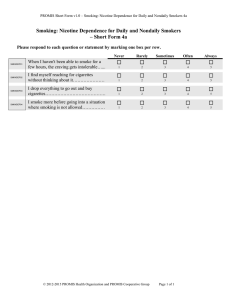
ELECTRONIC CIGARETTES COULD SAVE AMERICA: A REVIEW ON ELECTRONIC NICOTINE DELIVERY DEVICES AS A TOOL FOR SMOKING CESSATION by Ali Ayyash BS, University of Pittsburgh, 2013 Submitted to the Graduate Faculty of Epidemiology Graduate School of Public Health in partial fulfillment of the requirements for the degree of Master of Public Health University of Pittsburgh 2013 UNIVERSITY OF PITTSBURGH Graduate School of Public Health This essay is submitted by Ali Ayyash on December 14, 2013 and approved by Essay Advisor: Zmuda Joseph, PhD MPH MS Associate Professor of Epidemiology Associate Professor of Human Genetics Graduate School of Public Health University of Pittsburgh Essay Reader: Hillary Tindle, MD MPH Assistant Professor of Medicine Assistant Professor of Epidemiology Graduate School of Public Health University of Pittsburgh ii Copyright © by Ali Ayyash 2013 iii Joseph Zmuda PhD MPH MS ELECTRONIC CIGARETTES COULD SAVE AMERICA: A REVIEW ON ELECTRONIC NICOTINE DELIVERY DEVICES AS A TOOL FOR SMOKING CESSATION Ali Ayyash, MPH University of Pittsburgh, 2013 ABSTRACT Background: Electronic cigarettes (e-cigarettes) have recently emerged on the world stage as a new, popular nicotine delivery device. Approximately 1 in 5 current U.S. adult smokers have ever tried e-cigarettes and Google searches for the devices have increased dramatically over the past decade. While current FDA approved therapies are effective at helping smokers abstain from the habit, a majority of individuals attempting to quit fail or eventually relapse. Ecigarettes may provide an effective means of smoking cessation as it can administer nicotine and emulate the psychological stimuli associated with physically puffing on a cigarette. Methods: Sources on electronic cigarettes as a smoking cessation device were found using Pubmed and Google search. Results: 8 studies provide evidence that electronic cigarettes can help smokers cut back or quit smoking. 5 studies describe nicotine delivery of e-cigarettes and the ability of the device to reduce nicotine withdrawal symptoms and cravings. 3 studies reveal the effects on health and self-efficacy of e-cigarettes in tobacco smokers trying to quit. 3 studies describe the role of e-cigarettes in smoking cessation among special populations including smokers with depression, and schizophrenia. Discussion: Several qualitative and quantitative studies suggest that e-cigarettes may help tobacco smoker’s cutback or quit smoking regular tobacco cigarettes. Evidence also reveals that people who use e-cigarettes to iv quit tobacco cigarettes experience improved health and greater self-efficacy. E-cigarettes may also serve to decrease withdrawal symptoms and cravings in former smokers and may prove effective as cessation devices in special populations. The public health importance of this research is that e-cigarettes may help smokers quit smoking, and ultimately alleviate the burden of smoking related diseases across the world. v TABLE OF CONTENTS 1.0 Introduction 1.1 Smoking and public health…………………………………………………………………………………….1 1.2 What’s being done?.................................................................................................3 1.3 Nicotine Addiction…………………………………………………………………………………………………3 1.4 What are electronic cigarettes?...............................................................................5 1.5 Safety of electronic cigarettes……………………………………………………………………………….6 2.0 Methods……………………………………………………………………………………………………………………………8 3.0 Results (review of 19 pieces of literature)………………………………………………………………………….9 3.1 E-cigarettes as a tool to quit or reduce the use of tobacco cigarettes…………………….9 3.2 E-cigarettes as aids in avoiding Relapse, suppressing cravings and delivering nicotine…………………………………………………………………………………………………………………12 Improved health and self-efficacy with e-cigarette use…………………………………………14 3.3 E-cigarette efficacy in special populations…………………………………………………………….15 4.0 Discussion…………………………………………………………………………………………………………………………17 4.1 Concerns……………………………………………………………………………………………………………….19 4.2 Regulations……………………………………………………………………………………………………………20 4.3 Limitations…………………………………………………………………………………………………………….21 Bibliography……………………………………………………………………………………………………………………..23 vi 1.0 Introduction A recent article published in the New York Times brings attention to the growing popularity of electronic cigarettes as increasing numbers of tobacco smokers are switching to the device[1]. With bans on smoking indoors, smokers across the US now have a means of getting their nicotine fix while at work, in restaurants, or in night clubs[1]. The popularity of electronic cigarettes is further evidenced by the increasing number of Google searches for the product[2] and it’s use by celebrities around the country[1]. E-cigarettes look like tobacco cigarettes but do not contain tobacco or undergo combustion to generate usable forms of nicotine. When activated manually or by inhalation, the devices release a vapor that looks similar to smoke. Whether these devices are a safe replacement for tobacco cigarettes has been an ongoing debate for the past decade, but there is no question that their viability as an alternative nicotine source should be addressed given the increasing demand for the devices and scale of the US tobacco epidemic. This review will provide information on electronic cigarettes as a smoking cessation device by first highlighting the burden of tobacco smoke on public health. Next, an assessment will be made on what’s currently being done to alleviate the smoking epidemic and how e-cigarettes may assist as a smoking cessation device. Finally, the limitations and gaps in current studies on e-cigarette devices are addressed, and areas in need of future research are proposed in order to promote these devices as smoking cessation aids. 1.1 Smoking and public health Cigarette smoking is one of the largest preventable causes of death and disease in the United States[3] accounting for more than 440,000 deaths per year[4]. This number is 1 estimated to be more than deaths caused by HIV, illegal drug use, alcohol use, motor vehicle injuries, suicides, and murders combined[5]. While smoking rates have significantly decreased in the past 50 years, the number of smokers still remains high. It is estimated that the US national prevalence of smoking was 19% in 2011[6] and that the majority of smokers are adults between the ages of 25-44 years old[3]. The direct adverse effects of smoking are well documented. The 2004 Surgeon General report has summarized the existing relationship between smoking and a number of health related diseases. They include: lung cancer, laryngeal cancer, oral cavity and pharyngeal cancer, esophageal cancer, pancreatic cancer, bladder and kidney cancer, cervical cancer, gastric cancers, acute myeloid leukemia, cardiovascular disease, and several pulmonary disorders[7]. Similarly, smokers have a 2 to 4 times greater risk of coronary heart disease and stroke than nonsmokers[8]. Smoking related diseases presents a clear burden to the realm of public health by resulting in thousands of additional hospital admissions each year, costing massive amounts of money. Smoking cost the US $96 billion in health care expenditures per year between 2001 and 2004 and a $97 billion loss in productivity per year[4]. Smoking not only inflicts direct harm on the smoker, but also on those exposed to second and third-hand smoke. Cigarette smoke contains more than 7,000 different chemicals[9]. Hundreds of these chemicals are toxic and 70 are known to be carcinogenic[10]. Secondhand smoke causes an estimated 46,000 premature deaths from heart disease and 3,400 deaths from lung cancer in non-smokers per year[4]. Children and infants are also greatly affected by cigarette smoke. Second hand smoke increases the risk for sudden infant death 2 syndrome[9]. Second hand smoke alone is estimated to cost the US an additional $10 billion a year[11]. 1.2 What’s being done? In 2000, the first set of US clinical practice guidelines was established for treating tobacco dependent patients. These guidelines composed a review of over 3,000 articles to provide guidance for clinicians to treat tobacco use and dependence. In 2008, the guidelines were revised to include information from 2,700 additional sources[12]. These guidelines are now the standard for clinicians on how to provide treatment to smokers in the health care setting. The Joint Commission, the accrediting body for US hospitals, has also provided a set of quality measures that enhance and extend health care practices to hospitalized smokers. The new 2012 measures moved to provide cessation therapy to all hospitalized smokers[13]. These measures require hospitals to identify and document the tobacco use status of all admitted patients, provide evidence based counseling and FDA approved medication when appropriate, and follow-up with patients to obtain and document patient tobacco use status 15-30 days after discharge[12, 13] . 1.3 Nicotine Addiction The policies addressing tobacco use stem from the addictive properties of nicotine found in tobacco. Nicotine affects the pleasure pathways of the brain by increasing dopamine levels. The reaction between nicotine and dopamine is thought to underlie the pleasurable 3 sensations experienced by smokers, making the chemical addictive[14]. Nicotine dependence is identified as a chronic relapsing disorder with the majority of users continuing to use tobacco for many years and cycle through periods of remission and relapse[12]. It is estimated that 70% of current smokers want to quit smoking[12]. Although half of smokers attempt to quit smoking every year, most attempts will fail. Approximately 80% of smokers that try to quit without pharmacotherapy or counseling relapse within the first month and only 3% to 5% actually remain abstinent at six months[15]. This is largely a result of nicotine dependence, and the behavioral and psychological cues that trigger cravings and reinforce the smoking behavior[16]. Evidence has shown that both counseling and pharmacotherapy are effective at helping smokers quit. Nicotine replacement therapies (NRT) can double quit rates[17]. The FDA approved NRT products include: a transdermal nicotine patch, gum, inhaler, lozenge, and nasal spray. The non-nicotine first-line medications for smoking abstinence are bupropion SR (brand name Zyban) and varenicline tartrate (brand name Chantix)[12]. Along with pharmacotherapy, behavioral intervention such as counseling of either brief (3 minutes or less) or long (greater than 3 minutes) duration can help assist smokers to quit. The combination of medication and counseling is more effective than either medication or counseling alone [12, 18]. Although there is clear evidence that smoking cessation therapies such as NRT and behavioral methods do increase cessation, long-term quit rates are low[17]. Most NRT delivers nicotine to the bloodstream and then the brain more slowly than smoking[19]. Furthermore, most NRT, with the exception of the nicotine inhaler, fail to provide the physical and sensory stimuli provided by a cigarette. Many people also find certain NRT’s difficult to use or 4 unsatisfying [20, 21]. Electronic cigarettes could fill this void by providing smokers with nicotine while simultaneously fulfilling the psychological and sensory stimulus provided by tobacco cigarettes. 1.4 What are electronic cigarettes? Electronic nicotine delivery systems (ENDS), also known as electronic cigarettes or ecigarettes, have emerged in the past decade as a new popular alternative to smoking. Google searches for ‘electronic cigarettes’ have increased dramatically over the past few years[2] and the product is often seen in use by celebrities around the country [1]. It is estimated that between 2.1-3.3 percent of people in the United States have ever-used an electronic cigarette[22]. Electronic cigarettes resemble regular cigarettes but contain no tobacco. Unlike regular cigarettes, electronic cigarettes do not utilize combustion and instead, emit a vapor that appears similar to cigarette smoke. These devices are usually composed of three parts: a battery, an atomizer and a cartridge. A standard lithium ion battery powers the device. The atomizer activated manually by a switch or automatically when the user inhales from the device. When activated, the atomizer heats and subsequently vaporizes the liquid, called an eliquid, found within the cartridge. The cartridge holds the liquid that is vaporized by the atomizer and is often easily disposable or refillable[23]. 5 1.5 Safety of electronic cigarettes Electronic cigarette liquids are largely composed of propylene glycol, glycerol or both[24]. Other substances found in the liquids include nicotine, flavors and aromatics for taste and smell, tobacco-specific impurities, aldeyhydes and chlorinated solvents, and other additives[23]. Since propylene glycol and glycerol are the major contributors to e-liquid formulas, it is important to carefully review current information about their safety. Propylene glycol is a substance that is commonly used by the chemical, food, and pharmaceutical industries to absorb excess water and retain moisture within products[25]. The FDA has approved propylene glycol as a product that is generally safe when ingested[25]. A recent study performed on the varying organic forms of propylene glycol also concluded that they provide a “very low risk to human health.”[26] However, there are still few studies that analyze vaporized propylene glycol exposure. One 3-month study conducted on rats did yield similar safety conclusions between vaporized propylene glycol exposure and other ingested propylene glycol substituents. The researchers found that vaporized propylene glycol did not result in significant differences in the respiratory rates, minute volumes, or tidal volumes of the animals. They did however, detect a significant difference in mean body weight of exposed and unexposed females. The researchers also reported nasal irritation, bleeding, and ocular discharge resulting from the hydrophilic/phobic effects of propylene glycol on the nose and eyes[27]. A similar study also found minimal biological effects in rats after 90 days of exposure[28]. Glycerol, the other major component found in e-liquids, is often used in the food, pharmaceutical and agricultural industries[29]. The substance is recognized by the FDA as 6 generally safe when ingested[30], although there is no data on glycerol ingestion in the form of vapor. E-liquids often contain flavorings to enhance the taste and smell of the vapor produced by electronic cigarettes. Most of these flavorings are generic food additives that are generally safe when swallowed. However, in online forums of electronic cigarettes users, cinnamon flavored e-liquids have been known to cause irritating effects in users[23]. Overall, it is important to consider that heating a substance can alter the chemical composition of that substance and there is limited knowledge about the effects of these inhaled combusted flavorings. Two chemicals are of particular interest in the safety assessment of electronic cigarettes: tobacco- specific nitrosamines (TSNAs) and diethylene glycol (DEG). TSNAs are a group of known carcinogens found in tobacco and tobacco smoke. This group of chemicals has been known to induce tumors in animals and are likely the cancer causing agents found in tobacco cigarettes[31]. DEG is a colorless, odorless liquid that has a fatal dose of 1ml/kg. The substance is highly toxic and has been the cause of mass poisonings, usually as a result of contamination in pharmaceutical products in third world countries. Upon ingestion, the substance is rapidly absorbed and can lead to serious complications including death[32]. The presence of either tobacco-specific nitrosamines or diethylene glycol in e-cigarettes is concerning due to their negative impact on health. In 2011, Cahn and Siegel performed a review of 16 studies evaluating the chemical composition of several electronic cigarette brands. 14 out of the 16 studies found no tobacco 7 specific nitrosamines and 15 of the 16 found no DEG. 2 of the studies found trace amounts of TSNA levels at magnitudes of 500 to 1400 times less than concentrations found in regular cigarettes[33-35]. The maximum TSNA level reported in these studies was 8.2ng/g. This value is similar in magnitude to TSNA levels found in similar nicotine-level nicotine patches (8ng/g)[36]. A 2009 FDA report evaluated the chemical composition of three different brands of electronic cigarettes. DEG was identified in trace amounts in 1 of the 18 e-liquid cartridges studied[34]. While this detected quantity of DEG is small and poses little risk when consumed, it brings to light the current variability among e-liquids and the need to study the safety of ecigarette devices. Given the limited data on the safety of e-cigarettes, one should proceed with caution when recommending the devices as a smoking cessation tool. 2.0 Methods A keyword search was performed in Google (https://www.google.com/) and Pubmed (http://www.ncbi.nlm.nih.gov/pubmed/ using the terms: “electronic cigarettes cessation”, “electronic cigarette”,“nicotine replacement therapy electronic cigarette.” Each keyword search was narrowed down to ‘clinical trial’ article types in PubMed. Article titles and abstracts were scanned for content on electronic cigarette usage and smoking withdrawal symptoms and cessation. After the search, 8 articles were narrowed down using this method relating electronic cigarette usage and smoking cessation and withdrawal. 11 more references in the seminal literature by Jean Francois Etter titled “The Electronic Cigarette: An Alternative to Tobacco?” were also identified and used for a total of 19 total pieces of literature. 8 3.0 Results 3.1 E-cigarettes as a tool to quit or reduce the use of tobacco cigarettes Electronic cigarettes may serve as smoking cessation devices because of their ability to help smokers in the process of quitting. The most compelling piece of evidence to date in support of reduction or quitting by electronic cigarettes was a randomized controlled trial conducted in 2013. 300 randomly selected tobacco cigarette smokers who smoked ≥10 cigarettes/day for 5 years that were not intending to quit were assigned to one of three groups[37]. Group A received 7.2 mg nicotine cartridge for 12 weeks. Group B received 6 weeks of 7.2 mg nicotine cartridges followed by 6 weeks of 5.4mg nicotine cartridges, and Group C received 12 weeks of non-nicotine cartridges. The researchers found statistically significant reductions in cigarettes smoked per day from baseline in all three groups. Quit rates of 11, 17, and 4% were observed among the 3 groups respectively at 12 weeks and rates of 13, 9, and 4% were observed at 52 weeks. These quit rates are consistent with FDA approved firstline medication monotherapies[38]. At the end of the study, 73.1% of individuals who quit smoking regular cigarettes had quit all forms of smoking, indicating that these individuals had not substituted their tobacco use. Further evidence to suggest that electronic cigarettes can help reduce regular tobacco cigarette consumption in addicted smokers[39] was indicated by a study conducted on hospital staff members not intending to quit in the next 30 days who smoked ≥15 cigarettes per day for the past 10 years. Participants were invited to use a brand-name electronic cigarette for 6months. After the 6-month period, the 40 participants were categorized into 4 groups: 9 reducers, heavy reducers, quitters and failures. Reducers experienced a 50% reduction in cigarettes/day in the 30 days before the final study visit. Heavy reducers experienced an 80% reduction and quitters abstained from smoking for the 30 days prior to the final visit. Failures were labeled as participants who did not meet criteria for the 3 previously described categories. The researchers found that 32.5% of the 40 smokers were reducers and 38% of the reducers were heavy reducers. Overall, the study saw 9/40 quitters, yielding a total of 22/40 participants who either reduced or abstained from smoking regular cigarettes after 6-months of electronic cigarette use. The findings are suggestive of the idea that e-cigarettes may be able to decrease tobacco cigarette consumption in smokers not intending to quit. Surveys have also provided information on e-cigarette’s as an aid to quit or reduce tobacco smoking. Findings suggest that e-cigarettes may hold promise as a smoking-cessation method. In one study utilizing a sampling frame of all first time online purchasers of ‘Blu’ ecigarettes in a cross-sectional online survey[40], among the 222 respondents, a 6-month point prevalence of smoking abstinence of 31% was detected. Furthermore, 66.8% of respondents reported a reduction in daily tobacco cigarette use. 48.8% of participants reported abstinence from smoking for a period of time. The results from this online survey suggest that e-cigarettes may enable 6-month abstinence in tobacco cigarette smokers. An online survey of 3587 adult electronic cigarette users recruited from several ecigarette websites found similar results on the effects of electronic cigarettes on cessation and the profile, utilization patterns, satisfaction and perceived efficacy among electronic cigarette users[41]. In this survey, participants often used electronic cigarettes to reduce their cigarette 10 consumption. Many individuals participating in the survey were able to reduce their regular cigarette consumption or quit using e-cigarettes. Another online survey in 2010 aimed to describe the opinions and reasons behind using electronic cigarettes [41]. It was seen that participants often used electronic cigarettes like they would nicotine replacement therapies: as a tool to reduce or stop smoking regular cigarettes. Goniewicz et al. also yielded similar conclusions about the smoking characteristics of electronic cigarette users[42]. In an online survey of 179 people, Goniewicz’s team found that participants primarily used electronic cigarettes as a stop-smoking aid and the majority of the people participating in the study had been able to quit tobacco cigarettes using electronic cigarettes. These surveys suggest that ecigarettes may help smokers reduce or cut back smoking. Additional evidence of electronic cigarettes as a smoking cessation device has been found through qualitative research approaches [43, 44]. In a series of interviews with a convenience sample of 15 e-cigarette users from the MidWest Vapefest convention and meetings of the MidWest Vapers Group in St. Louis, MO, researchers talked with vendors and users of electronic cigarettes to understand the experiences of e-cigarette users. Individuals in the sample who had previously used the nicotine inhaler felt that the FDA approved device was unsatisfying as a nicotine substitute. A large portion of the sample also reported using lower nicotine concentration e-cigarettes over time. Participants indicated that they were able to go long periods of time without using their e-cigarette while they were unable to do so while smoking regular tobacco cigarettes. These findings suggest that e-cigarettes may help smokers wean off tobacco cigarettes. The study also primarily demonstrated the existence of a learning curve with e-cigarette usage. A face-to-face survey with 104 experienced e-cigarette users 11 yielded similar results through quantitative approaches. Of all the e-cigarette users interviewed, 78% had not used any tobacco in the 30 days prior to the study despite the fact that the participants had previously smoked an average of 25 cigarettes per day and had tried to quit smoking an average of 9 times prior to e-cigarette use. Almost all of the participants felt that e-cigarettes had helped them quit smoking. 3.2 E-cigarettes as aids in avoiding relapse, suppressing cravings and delivering nicotine Approximately 75% to 80% of smokers who attempt to quit relapse before achieving 6 months of abstinence[45]. Evidence has shown that individuals experiencing more severe withdrawal from nicotine abstinence are more likely to relapse[45]. Therefore, it is essential to review the data on electronic cigarettes as a means for alleviating nicotine withdrawal symptoms. Three studies quantified nicotine exposure of electronic cigarettes using blood measurements. One study conducted 4 different laboratory sessions with 32 participants from outpatient services who smoked at least 15 cigarettes per day [46]. Participants were asked to take 10 puffs of one of the following per study visit: a regular lit cigarette of the users preferred brand, a sham (unlit cigarette), an 18mg NPRO name brand electronic cigarette, or a 16mg Hydro name brand electronic cigarette. Physiologic measurements were then monitored by blood taken from a forearm catheter. A subjective questionnaire was also administered. The study found that the two electronic cigarette brands tested do not significantly expose electronic cigarette-naïve users to nicotine or carbon monoxide, but do reduce withdrawal symptoms. 12 Another study conducted with the same 4-group design aimed to measure the effects of electronic cigarettes on cravings and blood nicotine levels[47]. The study on 16 addicted cigarette smokers indicated that regular tobacco cigarettes were much more effective at increasing plasma nicotine relative to electronic cigarettes. The electronic cigarettes however, did provide some relief of cravings from tobacco abstinence. A study was conducted[48] to compare tobacco cigarette and e-cigarette effects on blood nicotine levels in 11 newly sampled experienced e-cigarette users[48]. It was found that experienced e-cigarette users who used their preferred electronic cigarette and e-liquid were able to increase their plasma nicotine to levels similar to regular cigarettes using an e-cigarette. These experienced participants also indicated that the electronic cigarettes helped alleviate withdrawal symptoms. This evidence suggests that e-cigarettes may be able to provide nicotine at levels similar to regular cigarettes, making the transition to e-cigarettes more favorable. Two studies provide evidence in support of e-cigarettes as a tool for reducing withdrawal symptoms [21, 49]. Dawkins et al. looked at the effects of e-cigarettes on desire to smoke, withdrawal symptoms, and cognition[49]. Using a mixed study design with a group of 86 tobacco smokers, individuals were randomized to a nicotine containing e-cigarette, a nonnicotine e-cigarette, or just holding the e-cigarette. After abstaining for 1 hour, participants using the electronic cigarette indicated a reduction in cravings over time relative to the just hold group regardless of nicotine content. Nicotine content was more important among males than females in reducing withdrawal symptoms. 13 Like Dawkins, Bullen also looked at the effect of electronic cigarettes on nicotine withdrawal but did so by comparing the effects of the device to an FDA approved nicotine inhaler [21]. The study conducted by Bullen et al., is one of the first to compare the effects of electronic cigarettes and traditional nicotine replacement therapies on desire to smoke and withdrawal. 40 adult smokers from the New Zealand community not trying to quit or were not planning to quit in the next 30 days who smoked 10 or more cigarettes per day completed the study. They were each randomized to one of four groups: 16 mg Ruyan V8 electronic cigarette, 0 mg Ruyan electronic cigarette, 10 mg nicotine inhaler, and their usual preferred cigarette. Individuals used one of these items for a day, and then were crossed over to a different item on a different day. Bullen’s team found that the usual cigarette caused a significantly greater reduction in desire to smoke than the other products however, there was a greater decrease in the desire to smoke over 1 hour with people using the 16mg electronic cigarette vs. the 0mg nicotine electronic cigarette. There was little to no difference in withdrawal symptoms between the 16mg electronic cigarette and the 10mg inhaler. This finding indicates that the ecigarette’s ability to suppress withdrawal symptoms may be similar to those of conventional NRT such as the nicotine inhaler. 3.3 Improved health and self-efficacy with e-cigarette use Qualitative data from e-cigarette users suggests that current and former tobacco cigarette users experience improvements in health from using electronic cigarettes. In Etter’s internet survey of electronic cigarette users, participants who formerly used tobacco cigarettes indicated improvements in their breathing and respiration, and reductions in coughing, sore 14 throats, and expectoration [41]. Similar results were found in an internet survey of 303 electronic cigarette users recruited from e-cigarette websites among participants who completely replaced tobacco cigarette smoking with e-cigarette use [50]. These individuals saw improvements in their sense of taste, smell, and ability to exercise. McQueen’s interviews with electronic cigarette users also revealed that participants who switched from tobacco cigarettes to electronic cigarettes felt an improved quality of life through improved taste, smell, physical activity and breathing[43]. Evaluating the self-efficacy of e-cigarette users is also vital to make predictions on a smoker’s ability to quit smoking. A survey of 1567 Hawaiian tobacco smokers recruited from a Hawaiian newspaper indicated that individuals who had ever used an e-cigarette for smoking cessation had greater confidence in their ability to quit tobacco cigarettes than participants who had never used an e-cigarette [51]. These results were also found in the 2010 Etter and Bullen survey on the profiles of e-cigarette users where users of e-cigarettes had greater confidence in their ability to quit smoking than non-users of e-cigarettes [52]. 3.4 E-cigarette efficacy in special populations Three sources of literature reveal information on the efficacy of e-cigarettes as smoking cessation aids among special populations of tobacco smokers. A prospective 12-month study performed by Caponnetto et al. recruited 14 schizophrenic individuals from a Psychiatric Rehabilitation Center[53]. All of the participants in the study had smoked ≥20 cigarettes/day for at least the past 10 years and were not intending to quit. Individuals were invited to use a Categoria name brand e-cigarette for 12 months. Participant outcomes were then organized 15 into two categories: those who experienced sustained 50% reduction in the number of cigarettes per day for the 30 days prior to week 52 and those who experienced sustained abstinence for the 30 days prior to week 52. Overall, 9/14 participants quit or reduced their tobacco cigarette consumption over the course of the study (50% reducers and 14.3% quitters). Substantial reductions in exhaled carbon monoxide, a marker of continued tobacco smoking, were also observed among participants. Caponnetto also provides qualitative data supporting electronic cigarettes as a smoking cessation device in special populations through case reports. The aim of these reports was to provide objective measures of smoking cessation in smokers with histories of relapse that have experimented with electronic cigarettes. The first is a case of three heavy smokers with a history of relapse. These patients had all been managed for nicotine dependence in the past using first line treatments. All 3 patients were able to use electronic cigarettes to maintain abstinence from smoking regular cigarettes for six months or longer[54]. The second case study describes two patients with documented depression and history of relapse with tobacco cigarettes. After using electronic cigarettes, both patients were able to remain abstinent for at least 6 months[55]. This is the first report of heavy smokers with depression who were able to quit smoking using an electronic cigarette when they couldn’t with counseling and NRT. Both of these pieces of literature provide evidence to the fact that electronic cigarettes may provide as a means of cessation in populations of people who are heavy smokers and have struggled with quitting in the past. 16 4.0 Discussion Tobacco cigarettes are one of the leading causes of death and disease in the United States [3]. Most cigarette smokers want to quit, but are unable to maintain abstinence even when using FDA approved therapies such as counseling and first-line medications. Although these methods have been proven effective as cessation tools[12], many smokers find these therapies unappealing[43, 56]. With the exception of the nicotine inhaler, the FDA approved first-line medications are also unable to simulate the sensory and psychological stimulation provided by regular tobacco cigarettes. The electronic cigarette on the other hand, looks and is used like a cigarette and thus has the ability to deliver nicotine while providing smokers with a physical experience similar to tobacco cigarettes. The small but growing body of literature on the subject of electronic cigarettes and smoking cessation reveal several interesting findings about the devices. People who use electronic cigarettes often do so with the intention of quitting or reducing their tobacco smoking habits[41, 52] and a large portion of users are able to successfully quit or cutback using the device [40, 44, 50, 52, 54, 55]. People who use ENDS for cessation purposes report improvements in tobacco smoking symptoms such as improved breathing, reduced coughing, increased physical fitness, and better sense of taste and smell[41, 50] E-cigarettes may also work as a cessation tool in certain populations of people including heavy smokers with a history of relapse, smokers with a history of depression, and smokers with schizophrenia [53-55]. Findings from the first randomized controlled trial were released in 2013 regarding the efficacy of e-cigarettes on smoking reduction and abstinence. The trial 17 found cessation rates similar to current FDA approved nicotine replacement therapies. This study also found that the vast majority of individuals who experimented with e-cigarettes and subsequently quit tobacco cigarettes did so by cutting out all nicotine, indicating that people may not be replacing one product for another[37]. As a randomized clinical trial, these findings provide groundbreaking evidence that ENDS may serve as a way to cut back or quit regular tobacco cigarettes. People have also reported using electronic cigarettes in order to avoid relapsing to regular cigarettes [52]. According to current evidence, electronic cigarettes have been able to reduce the cigarette cravings among former smokers[49] and perform as well as the nicotine inhaler in reducing cravings[21]. The reduction in desire may be greater in nicotine containing e-liquids [21]. This suggests that such tools could be used to prevent former smokers from relapsing back to tobacco cigarettes. It should be noted that there can be great variability in nicotine plasma levels of ecigarette users. Experienced e-cigarette users who use their own particular brand of e-cigarette and e-liquid may be able to effectively increase their plasma nicotine levels to values similar to that of cigarettes while novice users may not [46-48]. This finding potentially supports the idea that there is a learning curve to using electronic cigarettes and effective nicotine dosing is reliant on overcoming this curve [44]. Therefore, in order to adopt e-cigarettes as a smoking cessation treatment, there would need to be a form of standardization among electronic cigarette devices and liquids that could administer uniform dosages of nicotine and cater to the needs of both beginner and experienced users. 18 4.1 Concerns There are several concerns with the mass adoption of ENDS as a tool for smoking cessation. A large number of these arguments are rooted in the discussion of harm reduction as a tool to alleviate the worldwide smoking epidemic. Although the majority of e-cigarette use occurs among current and former smokers[41, 52] attempting to quit or stay quit from regular cigarettes, there is a fear that e-cigarettes may hinder cessation efforts among current smokers by causing those who might have quit smoking to instead become addicted to e-cigarettes[57]. Such concerns are justified according to a study that found that approximately half of individuals using e-cigarettes had become addicted to the device after using them to quit[42]. If the devices simply shift addictive habits in individuals, then serious evaluations on the safety and addictive properties of ENDS should be studied although ENDS contain very few to none of the dangerous chemicals found in regular cigarettes [33, 34]. Another fear associated with ENDS adoption is that individuals, specifically nonsmokers, will start using ENDs due to their promotion as a safer alternative to cigarettes. It is difficult to speculate on the future use of e-cigarettes among non-smokers, but similar nicotine replacement products such as the nicotine gum and patch have gained traction among nonsmokers[58]. A similar effect may be seen if e-cigarettes are adopted as a valid alternative for smoking cessation. This issue also relates directly to the current evidence suggesting that ecigarettes are gaining popularity among children and adolescents. It is estimated that approximately 1.78 million middle and high-school students nationwide have tried e-cigarettes and that e-cigarette use among this same group doubled between 2011 and 2012 [59]. Seeing 19 as e-cigarettes may be addictive and are growingly popular in younger populations, it is important to implement regulations that will decrease access of such products to youth populations. This evidence reinforces the need to thoroughly understand the health risks and addictive properties of ENDs. 4.2 Current Regulations Current legislation specifically allows the Food and Drug Administration (FDA) to regulate tobacco products that are “made or derived from tobacco.” Being as e-cigarettes are tobacco free devices, they are not regulated under the same criteria as regular cigarettes. Similarly, the FDA does not hold ENDS to the same regulation standards as drugs and pharmaceuticals because e-cigarettes are not marketed as therapeutic devices. Therefore ecigarettes are subject to the same standards of other consumer products[60]. Arguments for medicinal regulation of e-cigarettes are aimed at increasing consumer safety[61]. Medicinal regulation would ensure safety product labeling as well as standardization between e-liquid chemical compositions[61]. Such regulation would place ecigarettes on equal terms with NRT, increasing competition between the two groups. Again, it is vital to further explore the health risks of e-cigarettes, and then compare those risks to traditional NRT to determine whether such regulation is appropriate. The arguments for regulating electronic cigarettes as tobacco products are somewhat more compelling from a public health perspective. Such regulation would allow for rigorous taxation of the products and an increase in standardization among e-liquids. These efforts would generate money for the government and unify the health risks among different e20 cigarette brands. Legislation promoting tobacco regulations on e-cigarettes have received a lot of opposition from smaller e-cigarette manufacturers as it would drive up costs for smaller companies and allow bigger e-cigarette companies to control the market[62]. 4.3 Limitations It is important to consider the limitations of the previous research studies. Several of the studies utilized internet surveys as the method of data collection. Internet surveys often include people who have a computer or access to the internet and are thus likely to be more educated or have a higher income and may not appropriately represent all smokers. Another limitation is that participants of these internet surveys were often self-selected from forums or websites promoting electronic cigarettes. This could potentially influence the opinions of participants on e-cigarette use. The brands of e-cigarettes tested were usually very limited within studies bringing up another limitation considering that there are several hundred brands of e-cigarettes. Several of the clinical studies were limited by poor follow-up rates. It is possible that the individuals who did not attend final study visits were less optimistic about e-cigarettes or failed to abstain/cut-back their usually cigarette smoking habits. Finally, this review included information from qualitative research. Qualitative forms of research can be limited by non generalizable data or bias that should be taken into consideration when interpreting the results. Despite these limitations, current evidence regarding the ability of electronic cigarettes to reduce cigarette cravings, reduce smoking, and abstain from smoking regular cigarettes is 21 compelling. It is vital that more research be done on the safety of these products prior to their promotion as smoking cessation aids. Currently, electronic cigarettes are not regulated by pharmaceutical or tobacco standards, which results in great variability of the efficacy of nicotine delivery among different e-cigarette brands[61]. In order to promote these items as a cessation tool in the future, it is important to first ensure the long and short-term safety from first, second, and third hand smoke from these devices. It would then be essential to create a method of standardization for the products to reduce variability and toxicity among different products. Finally, it would be essential to educate the public on the devices and biological nature of nicotine addiction for future promotion. 22 Bibliography 1. 2. 3. 4. 5. 6. 7. 8. 9. 10. 11. 12. 13. 14. 15. 16. 17. 18. 19. Kurutz, S., Confounding a Smoking Ban, and Bouncers, in The New York Times. 2013: New York. Yamin, C.K., A. Bitton, and D.W. Bates, E-cigarettes: a rapidly growing Internet phenomenon. Ann Intern Med, 2010. 153(9): p. 607-9. CDC, Current Cigarette Smoking Among Adults- United States, 2011, in MMWR. 2012. p. 889894. CDC, Smoking-Attributable Mortality, Years of Potential Life lost, and Productivity Losses- United States. 2000-2004. 2008. p. 1226-1248. CDC. Health Effects of Cigarette Smoking. Smoking and Tobacco Use 2013 [cited 2013 8/14]; Available from: http://www.cdc.gov/tobacco/data_statistics/fact_sheets/health_effects/effects_cig_smoking/. CDC, 2011 National Health Interview Survey (NHIS) Public Use Data Release. 2012, U.S. Department of Health and Human Services: Hyattsville, Maryland. Services, U.S.D.o.H.a.H., The Health Consequences of Smoking: A Report of the Surgeon general. . U.S. Department of Health and Human Services,Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2004 Atlanta, GA. Secondhand Smoke Exposure and Cardiovascular Effects:Making Sense of the Evidence. 2010: The National Academies Press. The Health Consequences of Involuntary Exposure to Tobacco Smoke: A Report of the Surgeon General. U.S. Dept. of Health and Human Services, Centers for Disease Control and Prevention, Coordination Center for Health Promotion, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health: Atlanta, GA. How tobacco smoke causes disease: the biology and behavioral basis for smoking attributable disease : a report of the Surgeon General. . Dept. of Health and Human Services, Public health Service, Office of Surgeon General, 2010. : Rockville, MD. p. 704. Donald Behan, M.E., Yijia Lin, Economic Effects of Environmental Tobacco Smoke. 2005, Society of Actuaries: Schaumburg, IL. Fiore MC, J.C., Baker TB, et al. , Treating Tobacco Use and Dependence: 2008 Update. , in Clinical Practice Guideline. 2008, U.S. Department of Health and Human Services. Public Health Service: Rockville, MD. Fiore, M.C., E. Goplerud, and S.A. Schroeder, The Joint Commission's New Tobacco-Cessation Measures — Will Hospitals Do the Right Thing? New England Journal of Medicine, 2012. 366(13): p. 1172-1174. NIDA, Tobacco Addiction, in National Institute on Drug Abuse Research Report Series. 2012. Hughes, J.R., J. Keely, and S. Naud, Shape of the relapse curve and long-term abstinence among untreated smokers. Addiction, 2004. 99(1): p. 29-38. Buchhalter, A.R., et al., Tobacco abstinence symptom suppression: the role played by the smoking-related stimuli that are delivered by denicotinized cigarettes. Addiction, 2005. 100(4): p. 550-9. Stead, L.F., et al., Nicotine replacement therapy for smoking cessation. Cochrane Database Syst Rev, 2012. 11: p. CD000146. Rigotti, N.A., M.R. Munafo, and L.F. Stead, Smoking cessation interventions for hospitalized smokers: a systematic review. Arch Intern Med, 2008. 168(18): p. 1950-60. Le Houezec, J., Role of nicotine pharmacokinetics in nicotine addiction and nicotine replacement therapy: a review. Int J Tuberc Lung Dis, 2003. 7(9): p. 811-9. 23 20. 21. 22. 23. 24. 25. 26. 27. 28. 29. 30. 31. 32. 33. 34. 35. 36. 37. 38. 39. 40. 41. 42. 43. 44. Walker, N., et al., Does improved access and greater choice of nicotine replacement therapy affect smoking cessation success? Findings from a randomized controlled trial. Addiction, 2011. 106(6): p. 1176-85. Bullen, C., et al., Effect of an electronic nicotine delivery device (e cigarette) on desire to smoke and withdrawal, user preferences and nicotine delivery: randomised cross-over trial. Tob Control, 2010. 19(2): p. 98-103. King, B.A., et al., Awareness and ever-use of electronic cigarettes among u.s. Adults, 2010-2011. Nicotine Tob Res, 2013. 15(9): p. 1623-7. Etter, J.-F., The Electronic Cigarette: An Alternative to Tobacco? 2012, Geneva, Switzerland: JeanFrançois Etter. Chemical Composition of "Instead" Electronic Cigarette Smoke Juice and vapor. 2009, Alliance Technologies: Mommouth Junction, NJ. FDA, Propylene Glycol, in Database of Select Committee on GRAS Substances (SCOGS) Reviews. U.S. Food and Drug Administration. Fowles, J.R., M.I. Banton, and L.H. Pottenger, A toxicological review of the propylene glycols. Crit Rev Toxicol, 2013. 43(4): p. 363-90. Suber, R.L., et al., Subchronic nose-only inhalation study of propylene glycol in Sprague-Dawley rats. Food Chem Toxicol, 1989. 27(9): p. 573-83. Gaworski, C.L., M.J. Oldham, and C.R.E. Coggins, Toxicological considerations on the use of propylene glycol as a humectant in cigarettes. Toxicology, 2010. 269(1): p. 54-66. Drugs.com. Glycerol. July 13; Available from: http://www.drugs.com/inactive/glycerol-231.html. FDA, Glycerin and Glycerides. U.S. Food and Drug Administration. Hecht, S.S. and D. Hoffmann, Tobacco-specific nitrosamines, an important group of carcinogens in tobacco and tobacco smoke. Carcinogenesis, 1988. 9(6): p. 875-84. Schep, L.J., et al., Diethylene glycol poisoning. Clin Toxicol (Phila), 2009. 47(6): p. 525-35. Cahn, Z. and M. Siegel, Electronic cigarettes as a harm reduction strategy for tobacco control: a step forward or a repeat of past mistakes? J Public Health Policy, 2011. 32(1): p. 16-31. Westenberger, B.J., Evaluation of e-cigarettes. 2009, U.S. Food and Drug Administration. Laugesen, M., Safety Report on the Ruyan e-cigarette Cartridge and Inhaled Aerosol, in Health New Zealand Ltd. 2008. Stepanov, I., et al., Tobacco-specific nitrosamines in new tobacco products. Nicotine Tob Res, 2006. 8(2): p. 309-13. Caponnetto, P., et al., EffiCiency and Safety of an eLectronic cigAreTte (ECLAT) as tobacco cigarettes substitute: a prospective 12-month randomized control design study. PLoS One, 2013. 8(6): p. e66317. Smith, S.S., et al., Comparative effectiveness of 5 smoking cessation pharmacotherapies in primary care clinics. Arch Intern Med, 2009. 169(22): p. 2148-55. Polosa, R., et al., Effect of an electronic nicotine delivery device (e-Cigarette) on smoking reduction and cessation: a prospective 6-month pilot study. BMC Public Health, 2011. 11: p. 786. Siegel, M.B., K.L. Tanwar, and K.S. Wood, Electronic cigarettes as a smoking-cessation: tool results from an online survey. Am J Prev Med, 2011. 40(4): p. 472-5. Etter, J.F., Electronic cigarettes: a survey of users. BMC Public Health, 2010. 10: p. 231. Goniewicz, M.L., E.O. Lingas, and P. Hajek, Patterns of electronic cigarette use and user beliefs about their safety and benefits: an Internet survey. Drug Alcohol Rev, 2013. 32(2): p. 133-40. McQueen, A., S. Tower, and W. Sumner, Interviews with "vapers": implications for future research with electronic cigarettes. Nicotine Tob Res, 2011. 13(9): p. 860-7. Foulds, J., S. Veldheer, and A. Berg, Electronic cigarettes (e-cigs): views of aficionados and clinical/public health perspectives. Int J Clin Pract, 2011. 65(10): p. 1037-42. 24 45. 46. 47. 48. 49. 50. 51. 52. 53. 54. 55. 56. 57. 58. 59. 60. 61. 62. USDHHS, The health benefits of smoking cessation: A report of the Surgeon General, U.S.D.o.H.a.H. Services, Editor. 1990, U.S. Department of Health and Human Services, Public Health Service, Centers for Disease Control and Prevention: Atlanta, GA. Vansickel, A.R., et al., A clinical laboratory model for evaluating the acute effects of electronic "cigarettes": nicotine delivery profile and cardiovascular and subjective effects. Cancer Epidemiol Biomarkers Prev, 2010. 19(8): p. 1945-53. Eissenberg, T., Electronic nicotine delivery devices: ineffective nicotine delivery and craving suppression after acute administration. Tob Control, 2010. 19(1): p. 87-8. Vansickel, A.R. and T. Eissenberg, Electronic cigarettes: effective nicotine delivery after acute administration. Nicotine Tob Res, 2013. 15(1): p. 267-70. Dawkins, L., et al., The electronic-cigarette: effects on desire to smoke, withdrawal symptoms and cognition. Addict Behav, 2012. 37(8): p. 970-3. Karyn Heavner, J.D., Paul Bergen, Catherine Nissen, Carl Phillips, Electronic Cigarettes (ecigarettes) as potential tobacco harm reduction products: Results of an online survey of ecigarette users. 2009. Pokhrel, P., et al., Smokers who try e-cigarettes to quit smoking: findings from a multiethnic study in hawaii. Am J Public Health, 2013. 103(9): p. e57-62. Etter, J.F. and C. Bullen, Electronic cigarette: users profile, utilization, satisfaction and perceived efficacy. Addiction, 2011. 106(11): p. 2017-28. Caponnetto, P., et al., Impact of an electronic cigarette on smoking reduction and cessation in schizophrenic smokers: a prospective 12-month pilot study. Int J Environ Res Public Health, 2013. 10(2): p. 446-61. Caponnetto, P., et al., Successful smoking cessation with electronic cigarettes in smokers with a documented history of recurring relapses: a case series. J Med Case Rep, 2011. 5(1): p. 585. Caponnetto P., et al., Smoking Cessation with E-Cigarettes in Smokers with a Documented History of Depression and Recurring Relapses. International Journal of Clinical Medicine, 2011. 2(3): p. 281-284. Shiffman, S., et al., Tobacco harm reduction: conceptual structure and nomenclature for analysis and research. Nicotine Tob Res, 2002. 4 Suppl 2: p. S113-29. Zeller, M., D. Hatsukami, and G. Strategic Dialogue on Tobacco Harm Reduction, The Strategic Dialogue on Tobacco Harm Reduction: a vision and blueprint for action in the US. Tob Control, 2009. 18(4): p. 324-32. Klesges, L.M., et al., USe of nicotine replacement therapy in adolescent smokers and nonsmokers. Archives of Pediatrics & Adolescent Medicine, 2003. 157(6): p. 517-522. CDC, E-cigarette use more than doubles among U.S. middle and high school students from 20112012. 2013. FDA, Electronic Cigarettes (e-Cigarettes). 2013. Hajek, P., et al., Should e-cigarettes be regulated as a medicinal device? The Lancet Respiratory Medicine, 2013. 1(6): p. 429-431. News, C., E-cigarettes to get FDA regulations like tobacco. 2011. 25