Objectives: To understand 1 Basic physics of magnetic moments, macroscopic
advertisement

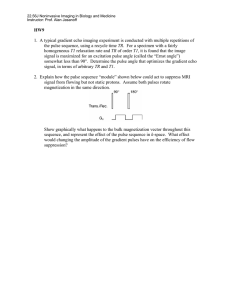
Objectives: To understand
1
Basic physics of magnetic moments, macroscopic
magnetization, precession,rotating reference frame
2
Relaxation and the Bloch equations
3
Free induction decay
4
The spin echo pulse sequence
5
Basic MRI apparatus, quadrature detection
6
Slice selection
7
Gradient Compensation
8
Spatial encoding
9
Spin warp imaging
10
Stimulated echos
11
Inversion recovery
12
Fast Imaging
13
Flow and Angiography--Phase contrast and time-of-flight
14
Maximum intensity projection
15
Qualitiative difference between angiographic methods
Nuclear magnetic resonance was discovered by Bloch and coworkers
and by Purcell and coworkers in 1946 and has been an important tool
for spectroscopic analysis of molecular structure ever since. Bloch and
Purcell received Nobel Prizes for their work.
The use of magnetic resonance for imaging purposes began in the
early seventies with perhaps the most important contributions made
by Lauterbur who suggested the use of gradient fields to encode
spatial position of the nuclear spins.
Commercial introduction of MR imagers began in the early 1980's
and since then MRI has become the greatest innovation in medical
imaging since computed tomography, which it has come to
outperform in several areas.
As we will see, in addition to directly competing in areas where CT
is used, MRI has far broader potential, for example in generating
quantitative flow information and for spectroscopic identification of
specific molecules taking part in physiological processes.
The force exerted on a particle with charge Q by an electric field E is
given by Fe= QE. If there were magnetic monopoles Maxwells
equations would be symmetric with respect to interchange of electric
and magnetic fields and we would have a force relationship like
Fm = mB. Fortunately, for patients sitting inside MRI magnets,
magnetic poles always come in pairs so that there is no net magnetic
force on static objects.
Figure 1 illustrates that for the case of a magnetic dipole, which does
exist, a torque T can be exerted on the dipole.
B
mB
+m
d
-m
- mB
The torque is given by
T = mdB = B
where is the magnetic dipole moment = md
(1)
A similar torque is exerted on a current carrying loop situated in a
magnetic field as indicated in Figures 2A and 2B
Figure 2A
Figure 2B
B
B
F = idl x B
•
A
x
i
µ = iA
Torque out of page = µ x B
The magnetic moment of this current loop can be shown to be =iA
The origin of the magnetic resonance signal is the nuclear magnetic
moment produced by the nuclear spin. The relationship between
angular momentum and the magnetic moment can be understood
qualitatively by considering the magnetic moment of a current loop
of area A, carrying current i, such as that shown in Figure 3.
Assuming that the current is due to a charge q of mass m traveling in a
circle at radius r as shown in Figure 3
we can write
= iA = (q) / (2 r/v ) (r 2 ) = (q/2) vr = (q/2m) mvr
= ( q / 2 m) J
(2)
where J = mvr is the angular momentum of the particle.
For a nucleus, we can consider that there is a distribution of rotating
charge analogous to that in the example. The differences between the
nucleus and the current loop are reflected in the factor multiplying the
angular momentum. In the case of the nuclear magnetic moment the
relationship is written as
J
(3)
where is called the gyromagnetic ratio and the magnitude of J is
related to the nuclear spin quantum number I by
J = (I ( I+1 )) 1/2 h / 2
where h is Plank's constant.
Although MRI in general deals with any nucleus having non zero
spin, protons are by far the easiest to image because they are most
abundant. For the purposes of this course we will limit our attention
to proton imaging. However, keep in mind that specialized
applications including sodium, phosphorus and other nuclei are
possible, although usually more difficult.
In the absence of an external magnetic field the proton spins in the
body would be randomly oriented giving rise to no measurable
magnetic moment in a volume the size of a typical imaging volume
element (voxel). However when placed in a magnetic field the proton
energy is quantized into two quantum levels which depend on whether
their spin is up or down relative to the magnetic field.
The higher energy level is associated with the spin down state since the
natural tendency is for spins to align with the field and work is required
to twist the spin around to the spin-down position.
The energy of the magnetic moment in the magnetic field is given by
E = -
For protons = ((1/2(1/2 +1))1/2 h/2and the two possible energy
states shown in Figure 4 are
E+ = + (1/2) (h/2 and E- = - (1/2) (h/2
B0
Spin up
E + Spin down N+
Spin down
E - Spin up
N-
Transitions from the low energy state to the high energy state may be
induced by radiation of frequency where
h= E
and
E = (E+ - E-) = (h/2) B0
(7)
(8)
This yields
=( / 2)B0
(9)
or an angular frequency of
= 2 B0
~ 64 MHz at 1.5 Tesla.
(10)
Photons with energy equal to the difference in energy between two
states are said to be in resonance with these states.
This is the origin of the "resonance " part of nuclear magnetic
resonance.
In the original applications of NMR, samples were irradiated with
radiofrequency radiation and the absorption of the radiation by the
sample was measured as the frequency was swept.
This produced a spectrum of absorption lines at various frequencies.
Because the protons in various molecules see slightly different
magnetic fields because of contributions from neighboring charges, it is
possible to identify the absorption lines associated with various
molecules by the so called "chemical shift " in their resonant
absorption.
When protons are placed in an external field B0 at temperature T there
will be an excess population of protons N- aligned with the field and
a somewhat smaller number N+ antiparallel to the field, where the +
and - refer to relative energy. The ratio of the number of protons in
the two energy states is given by the Boltzmann relation
N- / N+ = e E/kT
where k is Boltzmann's constant.
(11)
To calculate the ratio in the exponential we need
/ 2 = 42.58 * 106 Hz/Tesla
h / 2 Joules/Hz
and
k = 1.38 * 10-23 Joules / degree Kelvin
Assuming B=1.5T and a temperature of 300K, we obtainE =4.2*
10 - 26 Joules and kT = 4.14 * 10 - 21 joules. This gives E / kT = 10 - 5.
Therefore we can expand the exponential obtaining
or
(N-) - (N+) = N+
N/N =E / 2kT = 5 10 -6
(12)
Where we have used the fact that N = N + N and N ~ N .
+
+
So N+ ~ N/2
Therefore, there is an excess of only about 5 protons in 10 6 which
are aligned with the applied magnetic field. These excess protons
combine to produce a net magnetic moment per unit volume M.
Since there is no other defined direction except that of B0, the
expectation values of the components of the individual proton
magnetic moments along the x and y directions are zero.
Therefore the net magnetic moment ( or magnetization ) produced by
the excess protons points directly along the applied magnetic field.
Suppose that by some means the magnetization is tipped
away from its equilibrium direction along B0 as shown in
Figure 5.
B0
T
M
Figure 5
A torque given by
T = M x B0
(13)
will be exerted on the magnetization causing a precession around B0
with angular frequency prec .
The equation of motion of the magnetization is written by recalling
the angular form of Newton's second law, namely that torque equals
change in angular momentum. Therefore, since the angular
momentum per unit volume Jv is given by
Jv = M /
Newton’s second law bcomes
dJv / dt = d( M / ) / dt = M x B0
(15)
It can also be shown that for a vector M precessing at angular velocity
wprec
dM / dt = wprec x M
(16)
comparing equations 15 and 16 we see that
wprec = - B0
(17)
which corresponds to a clockwise rotation with an angular velocity
equal in magnitude to the angular frequency of the photons required to
induce transitions between the proton energy levels.
The precessing transverse component of the magnetization produces
a time varying magnetic field which can induce a voltage signal in a
receiver coil according to Faraday's law of magnetic induction,
which states that the induced EMF is equal to the time rate of change
of the magnetic flux through the receiver loop.
Recall that the flux is the integral of the normal component of the
magnetic field over the surface of the coil as shown in Figure 6.
B0
M
Receiver coil
Mxy
Induced
voltage
Optional reading
Ch. 14 and 15 Bushberg et al The Essential Physics
of Medical Imaging
Ch 28 Christensen
It is convenient to look at the behavior of the magnetization in a
reference frame rotating at an angular frequency equal to the resonant
frequency. It can be shown that in a reference frame rotating at angular
velocity f there is an effective magnetic field given by
Beff = B0 -f /
This can be seen by arguing that in the rotating frame the effective
rotational frequency is eff =B0 - fBeff which can be solved for
Beff .
For f = 0 = B0 the effective field of the NMR magnet goes to
zero in the rotating frame. As the frequency is increased from
below resonance to above resonance the z component of Beff
decreases from B0, goes through zero and then becomes negative.
In order for there to be precession, which is required before an
observable signal can be induced in the detector coil, we must tip the
magnetization into the transverse plane. This is done by applying a
radiofrequency field, usually called B1. The total effective field in the
rotating frame is given by
B' = B0 - + B1
(19)
In the rotating frame precession takes place around the effective field
B'. If a linearly polarized B1 field of frequency = 0 is applied it
can be shown that this can be decomposed into two circularly
polarized fields, one which rotates with the precessing magnetization
in the laboratory frame, and one which rotates at resonant frequency
but in the opposite (counterclockwise) direction from the
magnetization as shown in Figure 7.
Figure 7
B0
M
Laboratory frame
B1 cw
B1
B1 ccw
Any torques exerted on the magnetization by the counterclockwise
field cancel over time and produce no effect. In the rotating frame
neither the clockwise rf field nor the magnetization precess and the
clockwise component ,which we will call B1 from now on, can cause
the magnetization to precess toward the transverse plane as shown in
Figure 8.
z
M
M x B1
Rotating frame
y
x
B1
By analogy with our previous discussion of the torque exerted on M
by B0 , we can immediately write that the angular precession
frequencytip is given by
tip = B1
(20)
=wtip t
(21)
and the tip angle is given by
where t is the duration of the radiofrequency pulse.
As an example, let us calculate the size of the rf field needed to
produce a tip angle of 90 degrees in a time of 1 millisecond.
B1 =/ ( t ) = (( / 2 ) / ( 2 * 42 MHz/T * 10- 3 secs)
= 6 * 10- 6 T * (1 gauss /10-
4
T ) = .06 gauss
We should mention that if a linear excitation field is used, only one
half of the rf power is effective in tipping the magnetization. The
other half can still contribute to heating the patient. Therefore it is
more efficient to produce circularly polarized rf fields so that all of
the rf power is used for imaging purposes. This can be done using
so-called quadrature excitation using rf fields of sinusoidally
varying amplitude.
Suppose we apply a 180 degree rf pulse to a sample. The longitudinal
magnetization will be inverted and will point in a direction opposite
B0. The longitudinal magnetization will then undergo an exponential
return to equilibrium with a time constant T1 introduced by Bloch and
called the spin-lattice or longitudinal relaxation constant. Following
excitation, the longitudinal magnetization Mz will be given by
Mz = M0 - 2M0e - t / T1
as shown in Figure 9.
(22)
Longitudinal Magnetization Following Inversion
T1=1000 ms
Time Seconds
Notice that after four or five T1 intervals the system has nearly
returned to equilibrium. T1 is a phenomenological descriptor of the
rate at which various interactions between the proton and its
environment induce energy transitions which slowly result in the
reestablishment of the spin up and spin down level populations
predicted by the Boltzmann equation.
The importance of the T1 constant for medical imaging is that different
types of tissues have different T1 values. Depending on the sequence
of rf excitation and signal readout used to form the MR image, these
T1 differences produce differences in tissue contrast which may
readily be seen as pixel intensity differences on the image.
Bloch also introduced another time constant T2 which he ascribed to
the exponential attenuation of the transverse magnetization following
an excitation pulse. This time constant includes those interactions
which contribute to T1 but also those which involve only phase
changes as opposed to energy transitions. The effect of T2 decay
following a 90 degree pulse is shown in Figure 10. A homogeneous
B0 field is assumed for the present discussion.
Relaxation Following 90 Degree Pulse
Bloch introduced some phenomenological equations to describe the
sort of time dependent behavior of the magnetization described above.
The Bloch Equation is an extension of the basic Newton's second law
equation with the addition of terms describing the relaxation effects
and is given in vector form as
dM / dt = M x B - ( Mx i + My j ) / T2 - ( Mz - M0 ) k /T1
where i, j, and k are unit vectors along x, y, and z.
(23)
In the rotating frame, the first term, which produces precession, is
absent and the solutions reduce to
Mz = Mz0 e- t / T1 + M0 ( 1- e- t
= M0 - (M0-Mz0)e- t/T1
Mxy = Mxy0 e -t / T2
/ T1
)
(24)
(25)
where Mz0 is the initial longitudinal magnetization, M0 is the
equilibrium magnetization, and Mxy0 is the initial transverse
magnetization following the excitation pulse.
Remember that for any nuclear state the Heisenberg uncertainty
principle says that
E = h / t
(26)
recalling that E= hf, and w = 2f, we get
w=2/t
(27)
where t is the lifetime of the state.
This band of frequencies causes interference(dephasing) which causes
the signal decay as shown in Figure 12.
The frequencies which are present can be obtained from the Fourier
transform of the detected signal which is shown in Figure 13.
Narrow resonances are characterized by large T2 values. Wide
resonances are associated with short T2 values.
( FID ) In a Real Magnet
When an excitation pulse is given in a real imaging magnet, it is found
that the signal decays more rapidly than predicted by the transverse
decay constant T2 as shown in Figure 14.
Figure 14
The detected signal decays faster than expected, with a decay constant
called T2* associated with the combined effects of T2 and magnetic
field inhomogeneities which produce a spectrum of detected
frequencies. The oscillations inside the envelope imposed by T2*
decay occur near the resonant frequency. The interference between
several nearby frequencies associated with the variations in the
magnetic field lead to a rate of dephasing which is faster than that
predicted by T2 decay alone.
The Fourier transform of the detected signal gives the distribution of
proton precession frequencies present in the detected signal. The faster
the falloff in the transverse magnetization, the broader will be the
width of the observed proton line. This rapid falloff in signal is a
problem in imaging but is a disaster for spectroscopic applications
where one hopes to separate the peaks from protons in biological
molecules. Because of the line broadening produced by field
inhomogeneity, careful shimming of the magnet is done by tweaking
small currents in correction coils or by placing metal shims in the
magnet to perturb the field so as to achieve greater uniformity.
Some typical values for T1 and T2 are given in Table 1 in
milliseconds.
Table 1
B0 = .15 T
TISSUE
Grey matter
White matter
Fat
Cerebrospinal fluid (csf)
T1
520
380
170
2000
T2
95
85
100
1000
Table 1 continued
B0 = 1.5 T
T1
T2
Grey matter
950
100
White matter
780
92
Muscle
869
47
Blood
1200
100
Some general remarks can be made regarding T1 and T2. T1
increases at higher field strength, whereas T2 is fairly independent of
field strength. From the table above note that fat has a very short T1,
while csf has a very long T1. Solids have long T1 but very short T2.
See page 52 of Smith and Ranallo.
There are a variety of rf pulse sequences which can be used to
generate solutions of the Bloch equations which emphasize either
proton density, T1, T2, or combinations of these parameters. A
frequently sequence for MR imaging is the spin echo sequence. This
sequence has the property that the effects of magnet inhomogeneities
which lead to rapid decay of the MR signal are greatly reduced.
Consider the sequence of Rf pulses shown in Figure 15.
TR
TE/2
TE/2
90x
RF
a
b
90x
180y
c
d
signal
FID
ECHO
(data acquisition)
At time a, a 90 degree pulse is applied along the x axis in order to tip
the magnetization into the transverse plane. Because of field
inhomogeneities and T2 effects the spins will precess at different
angular velocities. In the rotating frame those spins precessing faster
than the resonant frequency will go clockwise, while those going
slower will precess in a counterclockwise fashion as shown at time b.
b
a
slower
y
x
dephasing
faster
At time c, a 180 degree pulse is applied along the y axis in order to
place the fast spins at the phase angle formerly occupied by the slow
spins and vice versa. Since the fast spins are still faster because their
local environment has not changed, they will catch up with the slow
spins which are now precessing toward them.
c
d
faster
rephasing
slower
Rotating frame
Note that the rephased amplitude is not as large as the amplitude of the
original FID since the effects of T2 decay may not be rephased. If a
series of 180 degree pulses are applied at equal intervals the signal
may be repeatedly rephased. The envelope of all the rephased signals
represents the T2 decay for the sample. In this way the spin echo
sequence permits improved measurement of T2 in the presence of field
inhomogeneities. From an imaging point of view it also removes so
called susceptibility artifacts which can arise at interfaces of dissimilar
materials.
The time between excitations is called TR and plays an important role
in the determination of T1 contrast since it determines the extent to
which the longitudinal magnetization recovers. For very long TR the
longitudinal magnetization of all tissues will have recovered producing
no contrast. High T1 contrast between two tissues is obtained by
choosing TR approximately equal to the average T1 of the two tissues.
Now that we have some idea how spins may be manipulated to
produce signal we will move on to MR imaging (MRI). We will need
to learn more about how pulse sequences can be manipulated to
produce various contrasts as different combinations of spin density,
T1, and T2 contrast are generated. But first we need to review the
basic imaging apparatus.
Figures 16 and 17 ( From General Electric Signa product literature )
illustrate the basis components.
Figure 16
CONTROL
COMPUTER
SCANNING
Shim
Supply
Image
Disc
Tape
Data
Disc
Magnet
Gradient Coils
Array
Processor
MAIN
COMPUTER
Gradient
Amplifiers
Pulse
Control
Module
Image
Processor
Operator’s
Console
Image
Processor
Image
Transceiver
Patient
Transport
RF
Amplifier
Remote
Console
A simplified schematic of the Signa System’s components and their interrelationships
Figure 17
Magnet and cryogens
Shim coils
Gradient Coils
RF Coils
The Z Gradient Coil
Z axis
RF Coils
Gradient Coils
Shim coils
Magnet and cryogens
A coil
flux lines
A cross sectional representation of the Signa Magnet
B coil
flux lines
The Z gradient coil varies the magnetic
field along the longitudinal plane
Nitrogen
X
Helium
Vacuum
X gradient coil
Cryogens surrounded by vacuum are used to to
maintain low temperatures
Y
Status Display
Panel
Button Controls
Trolley
Bridge
The Face of the Signa Magnet
Y gradient coil
Z
Relative orientation of X and Y gradient
coils
The main magnet can be permanent, resistive or superconducting.
The latter is commonly used for high field applications typically
above 1 T. Because uniformity is essential for decreasing T2*
signal decay and to prevent spectral broadening from the same
mechanism in spectroscopic applications shim coils are used to
tweak the magnetic field.
Superconducting magnets are operated at liquid helium temperatures,
about 4 degrees K. Both liquid helium and liquid nitrogen are
employed to ensure that the coils remain in the superconducting
range. Maintenance of cryogens is a major expense for MR scanning
with a superconducting magnet.The coils consist of superconducting
niobium-titanium wire embedded in a protective copper matrix. The
main magnet provides the B0 field which determines the resonant
frequency of the precessing protons.
The gradient coils provide linear variations of the local magnetic
field for the purpose of spatially encoding the positions of the
protons by creating spatial variations in their precession frequencies.
The x,y, and z gradient coils are all concentric with the z axis of the
magnet (patient cranio-caudal axis). The coils are formed by
wrapping conducting wire around a fiberglass cylinder. The z coils
are wrapped at the two ends of the magnet opening and produce
linear variations from B0 as distance increases from the magnet
isocenter. The x and y coils are saddle shaped and are identical to
each other except that the are oriented at 90 degrees to each other.
.
For the x and y coils it is important to realize that the effect is to
increase or decrease the magnitude of the z component of the field
in the x or y directions, not to introduce x or y field components
The main or so-called body rf coil is also enclosed within the magnet
cover and is usually of a birdcage resonator design. Additional
specialized coils which can be situated closer to the patient to
increase the detected signal are also used. Head, extremity, neck and
various surface coils are used in an attempt to improve signal to
noise ratio.
For some applications where the uniformity of deposition of rf
energy is better with the body coil, than with the specialized coils,
the body coil may be used to deliver a uniform tip angle while the
specialized coils are used for receiving only. Because the received
signal is thousands of times smaller than the rf excitation pulse, it is
important to detune the receiver coil during rf pulse transmission.
The received signal is sent to a quadrature phase detector. The
purpose of this circuit is to strip off the resonant frequency so that
audio frequency signals can be used for signal processing. This
amounts to analyzing the data in the rotating frame. Quadrature
detection is also necessary in order to distinguish between signals
which are equally displaced in frequency from the resonant frequency
in the positive and negative directions( since cos w= cos (-w) )
The processing is shown in Figure 18 and relies on the fact that
cos( + )t cos t = [ cos(t) + cos(2 + ) t ] / 2
(29)
and
cos( + )t (- sint) = [ sin t - sin(2 + ) t] / 2
(30)
cos ( + )t
Multiply by
cos t
Multiply by
- sin t
sin (t) +
- Sin (2 + )t
Cos (t) +
cos (2 + )t
Low pass filter
Low pass filter
sin (t)
Cos (t)
M real
imaginary
M imaginary
t
real
Because the imaginary signal is available ( the signal that has been
set up so that it is known to lag the real signal by 90 degrees ) it is
possible to distinguish between + and - values of w. This scheme is
referred to as quadrature detection.
This is illustrated in Figure 19 which shows how the availability of the
imaginary component can distinguish between the signals associated
with points at +x and -x. These signals have equal real parts but
opposite imaginary parts due to the fact that they are rotating in
opposite directions in the rotating reference frame.
imaginary
-x
•
-x
•
0
•
+x
+ t
- t
+x
real
Since the resonant frequency has been stripped from the detected
signal, further amplification and A/D conversion of the signal can take
place at audio frequencies ( kHz instead of mHz ). The real and
imaginary parts of the signal are separately digitized and are separately
stored in the computer so that phase images as well as magnitude
images can be formed.
In most MRI applications it is desirable to excite spins in specific
planes within the patient so that tomographic images analogous to
CT slices can be obtained. This is done by temporally modulating
the rf excitation pulse so that it contains a predetermined band of
frequencies. This rf pulse is delivered while a slice select gradient is
applied in the desired direction. This gradient creates a linear
variation in resonant frequency. Only those spins having resonant
frequencies within the bandwidth of the rf pulse are excited.
For example, suppose a gradient is applied along the z direction as
shown in Figure 20.
frequency
∆ rf bandwidth
Excited
Slice
∆Z
0
Z=0
Variation in resonant frequency
vs Z due to Z gradient
Z
Since the resonant frequency is given by f B/2 in the presence of
the Z gradient, which has a value Gz T/cm, the resonant frequency as
a function of Z becomes
f (Z) = (Z) / 2=(B0 + Gz Z) / 2
and the slice thicknessZ is related to the rf bandwidth by
f = Gz Z / 2
For a 1.5 T system with = 42 mHz/T and Gz = .5 G/cm, with
1G = 10- 4 T, a 2 cm slice requires
f = 4200 Hz
If we desire to place this slice around the position Z = +10 cm then
the center frequency shift f0 for the rf excitation should be
f0 = ( Gz Z ) / 2kHz
The rf excitation pulse is arranged to be circularly polarized with the
form
Bxy = e it
The desired rf bandwidth is obtained by temporally modulating the rf
with a waveform S(t) as shown in Figure 21.
xy
The overall waveform then becomes
Bxy(t) = e i wt S(t)
(33)
The Fourier transform of this is given by the convolution theorem as
xy(w') ('-)
where is the FT of S.
In order to form a well defined slice profile a sinc function
sin (t / t ) / (tt) as shown in Figure 22 is used.
This produces a rectangular profile in frequency (and in the slice
select direction) as shown in Figure 23.
∆ f = 1/ ∆t
Thus, for 1 millisecond t we obtain a bandwidth of 1000 Hz. For
Gz = 0.5 G/cm this produces a selected slice of
Z =f / (GZ/2 = 1000Hz / [ (42*106 Hz/T)*0.5*10- 4T ]
= 0.5 cm
During the slice selection process the rf pulse is applied while the
slice select gradient is turned on. The presence of the gradient will
act to dephase the transverse component of the magnetization. This
would reduce the amount of signal available at readout since, even if
a spin echo sequence is used, the effects of the dephasing due to
different amounts of precession at various spatial positions along the
gradient would not be refocused. Therefore it is necessary to apply a
negative lobe of the slice select gradient which is equal and opposite
to that which is present while the rf is applied.
This is shown in Figure 24.
RF
Slice select
Compensation
lobe
Although it is not obvious that the compensation lobe duration
should be half that of the slice select gradient, it can be shown that
this is a good approximation to the solutions of the Bloch equations.
( Bailes and Bryant ,Contemp. Physics,1984,vol.25. N0. 5, 441-475)
We should mention that since it takes several T1 periods for the
longitudinal magnetization to recover before the slice may be reexcited, it is possible to jump to other slices while the first slice is
recovering. In this way multi-slice techniques considerably decrease
the scan time which would be required for sequential single slice
techniques. This is a less important issue when very short TR
sequences are used.
Thursday- Thanksgiving no class
Tues Nov 3 RSNA no class
Thursday Nov 5
more MR
Tuesday Nov 10
MR applications
Thursday Nov 12
Review session
Tuesday Nov 17 Final exam CSC G5/113 10am-noon
Now that we have a slice selected in the z direction, we need to
determine the x and y coordinates within the slice. Spatial encoding
is done using gradients in the x and y directions, applied separately.
We will consider a one dimensional problem first.
Suppose in the slab shown in Figure 25 that there are two objects
at x1 and x2.
X
Y
•
•
x2
Z
∆Z
x1
Bz
x
B0
If we apply a gradient in the x direction, the objects will resonate at
frequencies relative to isocenter ( the point where the gradient
amplitude is zero ) of
1= Gx x1
and 2 =Gx x2.
(35)
By Faraday’s law, the detected signal in the receiver coil will be
proportional to the time derivative of the magnetic field and
therefore proportional to the rate of change of the transverse
magnetization. Assuming a 90 degree tip has been done we get
s2(t) = D1 1 e i1t + D2 2 e i2t
(36)
where e.g. D1 represents the density of protons at x1 multiplied by a
geometrical factor describing the coil sensitivity at x1.
Since the changes in w caused by the gradient are much smaller than
w0, we can replace the multiplicative (x) terms by 0 and write
s1(t)=s2(t) / 0 = ( D(x) e iw(x) t dx)
(37)
In the present example D(x) would just be the sum of two functions.
Note that it is important to keep the (x) terms in the phase factor.
The signal with0 stripped off can be expressed in terms of the
's as
s(t)= ( D(x) e i(x) t dx)
(38)
This describes a superposition of signals at different frequencies
which vary with x position and which are weighted by the signal
strength at each position. This would be equivalent to listening to all
of the radio stations on the dial at the same time.
This can also be written as
s(t) = D(x) eiGxxt dx
(39)
We can describe the spatial distribution of spins in the x direction
as a Fourier integral over spatial frequency kx as
D(x) = (1/2 D (kx) e ikx x dkx
(40)
where D (kx) represents the k space weightings of the spatial
frequencies needed to reproduce D(x).
Taking the FT of equation 40 we get
D(kx) = (1/2 D(x) e - ikx x dx
(41)
Now if we make the substitution in equation 39
s(t) = D(x) eiGxxt dx
(39)
that
Kx =-Gxt
we obtain
s(t) = ( D(x) e -iKxx dx)
(42)
(43)
Comparing equations 41 and 43
D(kx) = (1/2 D(x) e - ikx x dx
(41)
s(t) = ( D(x) e -iKxx dx)
(43)
we see that the two expressions are equivalent if
and
kx = Kx = -Gx t
(44)
This means that the MR signal at each t provides the k space
expansion coefficients for kx = Gx t .
To summarize, when we write the equation for the temporal signal
s(t), which contains several temporal frequencies, the fact that these
frequencies are linearly related to the x position enables us to write
an expression for s(t) which is identical to that for the Fourier
expansion coefficients D(kx) which describe the weightings of the
various spatial frequencies needed to describe D(x).
Let's use these equations to examine the imaging situation involving
the two point objects at x1 and x2 shown in Figure 25.
Since there is a direct relationship between the x axis and frequency,
there will be two frequencies superimposed in the detected signal as
shown in Figure 26 giving, according to equation 38,
s(t)= D(x1) e i (x1) t +D(x2) e i (x2) t
(45)
As a function of temporal frequency w(x) this waveform obviously
contains two temporal frequencies as shown in Figure 27.
X
Y
•
•
x2
x1
∆x
Signal
strength
2
1
However we can obtain the same result using the previous equations
which, in a more complicated situation, would be the best method.
Using equation 40, 44,and 45,
D(x) = (1/2 D (kx) e ikx x dkx
(40)
(44)
s(t)= D(x1) e i (x1) t +D(x2) e i (x2) t
(45)
we get
D(x) =
( (D(x1) e i (x1) t +D(x2) e i (x2) t) e ikxx dkx) /2
which , when we substitute kxx = -(x) t becomes
D(x) = ( (D(x1) e - i kxx1 +D(x2) e -i kxx2 ) e -i kxxdkx)/2
or,
D(x) = D(x1) ( e ikx(x-x1) dkx)/2 + D(x2) ( e ikx(x-x2) dkx)/2
or, recognizing the integral form of the delta function,
we get
e ikx(x-xi)dkx = 2(x-xi)
D(x) = D(x1) (x-x1) + D(x2) (x-x2)
which represents two delta functions at x1 and x2 in the x
domain as shown in Figure 28.
Figure 28
At this point we should emphasize that and x are linearly related by
Gxx and that time and spatial frequency are linearly related by
kx = -Gxt. Time and temporal frequency form one set of conjugate
Fourier variables, and x and spatial frequency in the x direction form
another as shown in Figure 29. Generally, everything is done by
converting all values to the x,kx pair.
x
FT
kx
FT
x
t
The MR signal is typically sampled 256-512 times during the echo
or FID. The relationship between the bandwidth w , desired field
of view in the x direction, FOVx, and the required x gradient is
given by
(kHZ) = Gx FOVx
(46)
The temporal bandwidth filter is used to prevent higher frequency
information outside the field of view from aliasing into the image.
This would occur because of undersampling of the temporal
information.
Aliasing can still occur in the directions perpendicular to the xreadout since, as we will, see there is no temporal bandwidth filter
available in those directions.
We will defer our discussion of spatial encoding in the y direction,
which is done somewhat differently. Eventually we will map out 128
(typically) lines in k space obtaining a continuous set of D (kx)
values as in Figure 26 for 128 fixed values of Ky. This method is
called SPIN WARP imaging. But first let's see how we could make a
2D projection imaging just with the x space ( Figure 28 ) encoding
that we have done.
If we apply a linear combination of x and y gradients simultaneously
we can repeat the above analysis along several different x' axes. The
D(x) values we obtain can then be back projected using the same
methods we have discussed for x-ray CT as shown in Figure 30.
Basically the D(x) values will reinforce where they overlap. As in the
x-ray case avoidance of the star artifact would require filtering before
back projection.
Figure 30
Recall that in our discussions of x-ray imaging we said that we could
represent any one dimensional image as a superposition of images
formed by sticking an appropriate series of sinusoidally transmitting
grids in the beam as shown in Figure 31.
The mathematical description of this is
Image(x) = ai sin kix + bi cos kix
where the ai and bi are real numbers.
(47)
If we have a set of grids of continuously varying spatial frequency we
can write this as
Image(x) = 1/(2) D(kx) eikx x dkx
(48)
where D(kx) is the weighting of the transmission contribution per unit
frequency interval from the grids. D(kx) is a complex number which
introduces whatever necessary phase is needed to ensure that the
proper admixture of sine grids and cosine grids are used.
To make a 2 dimensional x - ray image we would need some grids
oriented in the y direction. The transmission through these grids
would multiply the transmissions produced by the x grids. The grid
equation in pictorial form would be as shown in Figure 32.
Figure 32
Image (x,y)=
where it is assumed that each of the grids is multiplied by an
appropriate complex weighting factor which determines its
transmission and its lateral shift. In general the weightings of the x
grids may change depending on which y grid is in.
This gives us a 2 dimensional matrix or space of weighting coefficients
for the various spatial frequency grids present as shown in Figure 33.
ky
kx
This space is called (spatial) frequency or k space. The above example
illustrates the construction of an image in k space using a series of
grids with weightings which vary at each point shown in this space.
Knowing that it is possible to construct a 2 dimensional image by a
series of sinusoidal waves as we did above, the next question is to
ask how we can determine the weightings of the sinusoidal
construction functions at each point in frequency space. The
procedure is very similar to what we would do in a one dimensional
case.
For example, suppose we want to expand the square wave
x=0
- a/2
shown above into a cosine series as
+ a/2
square(x) = a0 +an cos kn x.
where kn = (2n-1)/a and n goes from 1 to infinity ( in practical
systems the highest frequency is always limited by apparatus or image
processing constraints).
The way we determine the weighting of the various cosine functions is
to multiply the function of interest by each cosine function one by one.
On the right side the products of all unlike cosine terms integrate to
zero (orthogonality). The cosine2 integrates to a constant giving
an = constant *
square(x) cosknx dx
(49)
As we will see, in spin warp magnetic resonance imaging, the
determination of the k space weighting coefficients along lines in
the kx direction is also carried out by multiplying the proton
distribution by one sinusoidal function of spatial frequency ky at a
time in the y direction and then multiplying by a series of sinusoidal
functions of frequency kx in the x direction.
Let us now consider the MRI case. A two dimensional distribution of
protons can be represented by a superposition of waves in two
dimensions as
D(x,y) = 1/2 D(kx,ky) e ikx x e iky y dkx dky )
(50)
Suppose that following excitation and before readout with the x
gradient as discussed earlier, we apply a y gradient for a short period of
time . While the y gradient is on, the precession frequency will
depend on y according to
y = Gy y
(51)
and the MR signal following application of the y gradient will have
acquired a phase factor equal to
y = Gy y
During the x readout the signal will be modified from our previous
signal equation as
s(t,)= ( D(x,y) e i(x) t ei Gy y dxdy )
(53)
Notice that this equation is analogous to equation 49
an = constant *
square(x) cosknx dx
(49)
for the solution of the Fourier expansion coefficient for the square
wave. In this case the image, in addition to being multiplied by the xwaves, is also multiplied by a sinusoidal wave of fixed frequency in the
y direction.
Setting ky = - Gy and recalling that (x)t= -kxx , equation 53
becomes
s(t,)/2= 1/2 ( D(x,y) e -i kxx e- i ky y dxdy )
(54)
Taking the 2D Fourier Transform we obtain
D(x,y) =1/4
( s(t,) e i kxx ei ky y dkx dky )
(55)
Comparing equations 50
D(x,y) = 1/2 D(kx,ky) e ikx x e iky y dkx dky )
(50)
and 55 we see that
s(t,) = 2D(kx,ky)
(56)
So, equation 54 which reminded us of the solution for the coefficient
of the square wave expansion functions is also a solution for the 2D
k space weighting coefficients in the MR case.
In the MR case the multiplication of the image (proton signal
distribution) is accomplished by applying a y gradient for a short
timeand producing a continuously changing sinusoidal
multiplication factor in the x direction by means of the x
gradientsSince kx = -Gxt and ky = -Gy depend linearly on t and
respectively, the signal obtained during x readout following the
imposed y gradient gives us a line of k space weighting coefficients
along a line of constant ky.
The variable is usually held constant while the y gradient is
incremented evenly, usually for 128 separate lines in k space.The
effect is the same as if the y gradient were held constant and were
allowed to increase linearly. This process is called phase encoding
but is better understood as solving for D(kx,ky) at fixed ky.
The temporal progression of the MR signal as the phase encoding is
increased is said to occur in pseudotime, a time variable which
increases a little bit at a time. The y direction is called the phase
encoding direction and the x direction is called the frequency
encoding direction.
Each line in k space, shown in Figure 35 is called a "view".
View 128
Ky
View 1
kx
The phase encoding gradient is usually represented on the pulse timing
diagram as shown in Figure 36.
Gy
The figure is meant to indicate that the y gradient is stepped so as to
cover all the necessary y spatial frequencies in k space. Notice that
negative as well as positive frequencies are obtained.
Remember the existence of "negative frequencies" really just means
that in order to have a complete Fourier representation of an object,
for example in the x direction, terms of the form e- ikx as well as terms
of the form eikx are required.
The extension of the 2D case discussed to 3D is straightforward. As
you might guess, an additional phase encoding operation is performed
by stepping the z gradient. In this way the Fourier coefficients
D(kx,ky,kz) are obtained, once again by fixing ky and kz and then
reading out the time varying signal during the x gradient.
The advantages of 3D imaging include the possibility of voxels of
equal size in all three dimensions and certain SNR gains derived from
processing the signal from the entire volume at all times during the
data acquisition.
The relationship between the field of view in the y direction, FOVy,
the spatial resolution in the y direction y and the k space resolution
ky are determined by the requirements of the Nyquist sampling
theorem which states that there must be two samples per cycle. This
means that since k = 2f,
kymax= 2/2y
(57)
The k space resolution ky is then given by, since the region from
-kymax to + kymax is spanned
ky = 2kymax/Ny = 2 / Nyy
(58)
where Ny is the number of phase encoding steps. It can be shown that
the number of pixels is equal to the number of phase encoding steps.
Therefore
FOVy = Nyy=2/ky
(59)
Therefore the field of view in the y direction is inversely proportional
to the k space resolution. For a given field of view the size of the pixel
in the y dimension is inversely proportional to the number of phase
encodes.
The size of the phase encoding gradient is determined by equations
(42) and (57). At the highest spatial frequency (and therefore the
highest Gy) there should be one cycle, or a 360 degree phase change
every 2 pixels as shown in Figure 37.
The progressive wrapping of the spins in the y direction in this
diagram is the origin of the term " Spin Warp ".
The Nyquist criterion leads to a phase shift per pixel of
r
max = Gymax y =
Gymax= FOVy / Ny)= Ny / FOVy
(61)
Therefore, if the desired FOVy and the number of phase encode steps
are known a can be chosen and Gymax is determined.
Just as we multiplied the square box function by the particular cosine
function to determine its weighting coefficient, in the case of MR
imaging we also multiply through by a factor which causes sinusoidal
variation in the y direction. The sinusoidal variation in detected
intensity from protons situated along the y direction is due to the
progressive twist in the spins in that direction. This twist is due to the
linearly increasing resonant frequency created by the y gradient.
Recall that since kyy=-t , the twist created by the linear gradient
causes the same sort of sinusoidal signal variation as the sinusoidal xray grid we discussed at the beginning of this section.
In the 2D MR case, multiplication by this sinusoidal variation in the y
direction not only gives us a single solution, but a series of weighting
coefficients at fixed ky and continuously variable kx (= -Gxt ) as the
signal is read out in time as shown by the solution machine in Figure
38.
In this machine we put in coins, first a ky coin and then a series of kx
coins to get out a series of D(kx, ky) solutions for the k-space
coefficients along one k-space view. Then we put in another ky coin
and start the kx coins over again. The ky coin corresponds to a phase
wrap in the y direction. As time goes on, the linearly increasing
frequency along the x direction multiplies the proton signal
distribution by sinusoidal functions of increasing frequency in the x
direction.
The proton phases are wrapped in the y and the x directions.The y
wrap is applied and held constant for each progression of x wraps.
At each point in time the detected signal is the solution for the
weighting function D(kx, ky) which multiplies the two dimensional
spatial frequency function which modulates the signal distribution
at that time. In general there is a different set of x weighting
coefficients for each value of the applied sinusoidal y function ( i.e.
for each phase encoding).
MR Scanner Acting As An Analog Computer
s(t,)/ 2 = D(kx,ky)= 1/2 ( D(x,y) e -i kxx e- i ky y dxdy ) (54)
B0
Receiver coil
M
D(kx,ky)
Mxy
y phase
encoding
twist ky
multiplies
proton signal
by fixed eiky
Gx
early
later
performs integral
to produce k-space
data D(kx,ky)
kx=-Gt
x
multiplies
proton signal
by eikx
There are a number of variations in the way that the spins may be
excited and read out. These various pulse sequences are designed to
create different contrast dependencies on T1, T2, spin density, spin
velocity, etc. Clinically it has been found that certain sequences are
best for certain applications. The radiologist must become familiar
with all of the available sequences in order to intelligently order the
sequence of scans which will lead to the most diagnostic image for
each case.
We will now review some of the most commonly used sequences
including the spin echo sequence described briefly earlier.
The pulse sequence for the spin echo sequence is shown in Figure 39.
TR
TE/2
RF
a
b
TE/2
c
180y
d
90x
90x
signal
ECHO
FID
(data acquisition)
Gz
Slice select
readout
Gx
Rephase in x
Dephase in x
Phase encode
Notice that the dephasing lobe of the x readout gradient which has
been placed before the 180 degree pulse has the same sign as that of
the rephasing portion. This is because the 180 degree pulse reverses
the relative positions of the phase shifts caused by the dephasing
gradient. Therefore the x dependent phase shifts are all refocused at
the peak of the echo.
The signal amplitude for the spin echo sequence may be derived by
considering the solutions of the Bloch equations and is given by
(62)
s =D(H) [1- e-TR/T1] e-TE/T2
where D(H) is the density of protons (with a coil sensitivity factor
lumped in) and T1 and T2 are the local relaxation values. By varying
TE and TR images emphasizing differences in each of these parameters
may be generated.
For large TR the term in brackets is close to one and T1 contrast will
be suppressed. This is because all substances regardless of their T1
values will have time to return to equilibrium value of longitudinal
magnetization. If, at the same time, TE is made short, the last term
will also generate little dependence on T2.
Therefore the combination of long TR and short TE produces an
image with signal proportional to the local density of protons. These
images usually have fairly low contrast.
Short TE combined with short TR produces T1 weighted images
since the first exponential term will be highly T1 dependent. The
combination of long TR and long TE will generate primarily T2
contrast. Which combination is chosen depends on the clinical
situation.
From the equation for the spin echo signal amplitude
s =D(H) [1- e-TR/T1] e-TE/T2
it can be seen that a tissue with longer T1 will appear darker than
one of shorter T1, since the term in brackets decreases for large T1.
On the other hand, longer T2 increases the image brightness as can
be seen from the last exponential term. Therefore T1 and T2
contrast are of opposite sign.
Since tissues with longer T1 usually have a longer T2, this effect
can produce a cancellation of contrast making it more difficult to
distinguish two different types of tissue. That is why it is important
to use images with different amounts of T1 and T2 weightings.
Sometimes in a spin echo sequence two different 180 degree pulses
are used after the rf excitation so that the first generates a short TE
and the second generates a long TE. In this way from a single rf
excitation two echoes can be recorded, the first containing little T2
contrast and the second containing significant T2 contrast.
Figure 40 illustrates the use of multiple 180 degree pulses to repeatedly refocus
the spins while they are in the transverse plane. This permits the acquisition of
images with different T2 weighting within the same 90 degree excitation
sequence. Notice that the refocused echoes have an amplitude falling on the T2
decay curve. The individual echoes decay at the T2* decay rate.
90
180
180
90
Excitation
))
TI
TE
Detected Signal
TE
T2
decay
T2* decay
TR
Figure 41 (From Wehrli et al. Parameters Determining the
Appearance of NMR Images-General Electric) illustrates the wide
variation in image contrast that may be obtained with a spin-echo
sequence depending on the parameters chosen. Figure 41 shows two
sets of four echo acquisitions. Set A was obtained at TR = 0.5
seconds. Set B was obtained with TR =2.0 seconds. Within each set
the amount of T2 decay which occurs increases from left to right.
Figure 41
Note that in A1 the cerebrospinal fluid (arrows), which has a long
T1 and a long T2 is suppressed by the short TR which has
prevented full recovery before the application of the 90 degree
pulse. In B4 which corresponds to long T2 decay, the
cerebrospinal fluid has a greater relative image brightness than the
rest of the brain because of its long T2. The images have been
individually rescaled to show relative brightness.
It is possible to show that any two rf pulses will result in a spin echo
signal. In Figure 1 of Hahn "Spin Echoes",Physical Review, Vol. 80,
no.4 page 583, it is demonstrated how two ninety degree pulses lead
to the formation of a spin echo at a time equal to twice the
separation of the two pulses. Basically after being rotated to the
transverse plane, the spins fan out uniformly into a circular figure.
This figure is then rotated into the vertical plane by the second
ninety degree pulse. Then the spins, because of their different
precession rates refocus into a figure eight on the surface of a sphere
and form the peak echo signal. (You have to look at the figure).
Since any two rf pulses will have components in the transverse
plane, these 90 degree components will also form a spin echo
regardless of the rf tip angle.
In Hahn's paper he shows that three 90 pulses will also form an echo
which is called a stimulated echo and involves a rather complicated
set of illustrations. Foo (UW-1990) used the stimulated echo pulse
sequence related to the sequence shown in Figure 42 to image
blood flow.
TE
90
TE
TE
90
90
spin echo
Simulated echo
A spatially selective 90 pulse is applied in the upstream region of
the vessels of interest. These are allowed to fan out. Then a nonselective 90 is applied. This places all of the spins into the
longitudinal plane where no T2 decay is experienced. After a
suitable travel time, another spatially selective 90 is applied in the
downstream region of the vessels producing a stimulated echo for
those spins which saw all three 90 pulses.
Since the two selective 90 pulses do not overlap spatially, the static
tissue does not see all three 90 pulses and does not experience the
stimulated echo. Therefore this method represents a potential,
although not often used, non-subtractive approach to MR
angiography, which we will discuss in more detail later.
Notice in the diagram that a spin echo is formed due to the first two
90 pulses. Another spin echo would be formed from the second and
third 90 pulses. It is important to choose the time parameters so that
this echo does not overlap the stimulated echo. There are also FID
signals following application of the first and third 90 pulses. The last
one must also be over before the stimulated echo occurs or signal
from static tissue will be seen in the image.
The stimulated echo is also used in a spectroscopic technique called
STEAM in which three selective 90 pulses are used to excite a small
cubical region over which excellent field uniformity leads to
narrower spectral lines. This technique provides the opportunity to
examine a small selected region of the body where questions related
to tissue viability may be studied based on the presence of spectral
lines associated with various metabolites such as ATP.
spectroscopic voxel
excite three
orthogonal planes
A pulse sequence called inversion recovery is used to provide
maximal T1 contrast. In this sequence the longitudinal
magnetization is inverted using a 180 pulse and is then read out with
a 90 pulse after a time TI called the inversion time. The
magnetization recovers according to the equation
Mz = Mz0 ( 1 - 2 e-t
/ T1
)
(63)
where Mz0 is the equilibrium magnetization at the time of the 180
pulse. This value depends on the repetition rate TR.
The recovery curves for two tissues with T1 values of 1000 and 2000
are shown in Figure 43.
By choosing the inversion time so that one of the tissues is passing
through zero, this tissue will provide zero signal upon readout with
the 90 pulse. The maximum signal difference is obtained by choosing
TI to be approximately equal to the average of the two T1 values.
Following application of the 90 degree readout pulse, magnetization
which had passed through zero and was pointing upwards will be 180
degrees out phase in the transverse plane with magnetization which
was still negative at the time of the 90 degree pulse. This fact can be
used to distinguish between magnetization of equal magnitude but
opposite sign. Such phase corrected inversion recovery displays
preserve all of the contrast provided by the recovery of the
longitudinal magnetization.
The inversion recovery sequence may be combined with a spin echo
sequence as shown in Figure 44.
TR
TE/2
T1
180
90
FID
TE/2
180
180
SPIN ECHO
In this case the 180 degree pulses refocuses the dephasing caused by
T2* effects as in normal spin echo imaging. Additionally data can be
collected in negative as well as positive areas of frequency (k) space.
A special case of the inversion recovery spin echo sequence is the so
called Short TI Inversion Recovery (STIR) sequence. We mentioned
above that T1 and T2 effects produce opposing contrast leading to
possible cancellation of contrast. In the STIR sequence the inversion
time is kept short enough so that all of the longitudinal
magnetization is still negative. In this case tissues with smaller T1
will produce less signal following the 90 pulse. Once in the
transverse plane, the magnetization associated with tissues having
short T2 will decay faster leading to diminished signal.
Therefore the effects of T1 and T2, which are correlated within a
given tissue ( since T1 interactions also contribute to T2) will be
additive, removing the possibility of contrast cancellation.
Following a few years of heavy reliance on spin echo imaging,
interest was focused on techniques for faster imaging. These
techniques utilize gradient echo imaging with small tip angles.
The advantages of using small tip angles is illustrated in the Figure
45.
z
Mz0
.86 Mz0
30o
.5 Mz0
Mz0
M
For a 30 degree tip angle, half of the transverse magnetization is
realized while the longitudinal magnetization is only decreased by 13
percent. This permits rapid restoration of the longitudinal
magnetization so that short TR values may be used, thus reducing scan
time.
A gradient echo pulse sequence is shown in Figure 46 .
RF
a
a
signal
Readout gradient
Phase encode
spoiler
The dephasing lobe of the readout gradient dephases the FID. The
size of the gradient echo signal is the same as the FID would have
been at the same time if it had not been disturbed. Because there is no
180 pulse, the decay of the signals proceeds according to T2* and
field nonuniformity effects are not refocused.
In very short TR sequences it is possible for a so-called steady state
transverse magnetization to be set up. The alpha pulses (analogous to
the 90 degree pulses in a spin echo sequence) can cause spin echoes
which build up to produce a steady state signal separate from the
gradient echo which is formed from the FID . The contrast produced
by the steady state signal has a different dependence on T1 and T2*
than the gradient echo. In some cases it is desirable to suppress the
steady state signal.
In the sequence shown, the "spoiler gradient" on the phase encode
axis has been used to dephase the transverse magnetization. The
steady state can also be destroyed by randomly changing the phase of
the alpha pulses so that no steady state coherence is built up. This is
called "RF spoiling".
Gradient echo sequences are especially useful in MR angiography
where short TR sequences are used to suppress static tissues.
In conventional MR imaging, which typically uses spin echo
sequences, flow manifests itself as a signal void( dark region ) in the
slice images. This happens simply because in order for a spin echo to
be formed, the spins must see both the selective 90 and the selective
180 pulses. Thus, the cross sections of blood vessels are routinely
seen in axial spin echo images. The use of pulse sequences designed
to generate signal from flowing spins is called MR Angiography
(MRA). In the discussion below we will look at some of the basic
concepts of MRA.
There are three major types of MRA methods,
Phase Contrast
Time-of-Flight.,
and Contrast Enhanced.
Phase contrast angiography relies on the fact that spins moving in a
gradient with velocity v, for example in the x direction, will
experience a phase shift given by
=
(t)dt =
Gx vt dt
(64)
Consider the effect of placing a bipolar gradient in the x direction prior
to the x readout pulse as shown in Figure 47 .
RF
readout
x
It can be shown that the phase shift acquired by the moving spin as a
result of the bipolar gradient is
+ - = - G v t2
(65)
where t is the width of one of the bipolar lobes and G is the size of the
bipolar gradient.
= B(t) dt = G xdt = G vt dt
0
t
2t
= Gv/2 {t2
=-Gvt2
t
0
-t2 2t t =Gv/2 {t2-0 –4t2-t2}
For static spins the effects of the two lobes cancel and the net phases
shift is zero. This is shown in Figure 48.
Static Spins
Moving Spins
net
phase
Basically the static spins see equal and opposite magnetic fields
during the two lobes. Therefore, the phase shift caused by the
positive lobe is cancelled by that produced by the negative lobe.
However, for the moving spin, a greater magnetic field is seen
during the negative lobe, since it has moved along the gradient into
regions of higher field. Because of this the phase shift during the
negative lobe is larger than that during the positive lobe leading to
the net result calculated.
Now suppose that a bipolar gradient of opposite sign is used. This will
produce a phase shift of
- + = + G v t2
(66)
The complex difference between the signal readout following each of
these bipolar gradients will be proportional to
(67)
Therefore, for G v t2 less than or equal to about 1 radian, the
angiographic difference signal is approximately linearly related to
velocity.
The vector diagram associated with the formation of the complex
difference image is shown in Figure 49.
Complex
Difference
Signal
sinGvt2
The phase contrast data acquisition usually must be done using
separate bipolar sensitization gradients in all three directions. The
results from these three scans are added vectorially by taking the
square root of the sum of the magnitude images from the three scans.
It is important to set the size of the bipolar gradient carefully so that
velocities which are too high do not go over the top of the sine
function and provide incorrect or even zero signal. This is a problem
in areas of high vessel pulsatility in which the velocity varies greatly
within the cardiac cycle. Even in the absence of pulsatility there is a
distribution of velocities within vessels. For parabolic flow in a
circular vessel the peak flow velocity in the center of the vessel is
twice the average velocity and the velocity at the edges of the vessel
is near zero.
VENC
sinGvt2
velocity aliasing
v
The phase contrast method can be implemented in a phase difference
display mode in which phase difference images are used instead of
magnitude images. In this mode images display flow direction rather
than just speed. In this mode only one direction of flow sensitization
can be used at a time. This mode is most useful in vessels with flow in
one dominant direction. The phase difference image is calculated as
arctan
I
R
arctan
I
(68)
R
where, for example, R+ and I + are the real and imaginary components
of the signal obtained with the bipolar gradient of positive (up-down)
polarity.
Velocity-Resolved PC
1
2
11:12
P
3
2563
4
Sum of S/I Velocity Images
5
6
Sum of flows
Vel FOV =
+/- 60cm/s
Vres =17cm/s
A
4 x 2 enc steps
7
8
Sc =22
Speed Image
It is important to obtain a phase difference in order to eliminate any
non-zero phase which might be associated with the static background
tissues, which, even though they are not moving, typically have nonzero phase.
The size of the velocity sensitization gradient is usually chosen so
that the fastest velocities present will provide a phase difference of
. The velocity corresponding to this maximum phase difference is
called VENC. Velocities greater than VENC will be aliased to lower
velocities. This can be a problem in clinical imaging where the
velocity spectrum present is unpredictable and changes throughout
the cardiac cycle.
It should be noted that although the static tissue cancels in the
complex difference image, its presence leads to an underestimation of
phase and therefore of velocity. This is a so-called partial volume
effect. When phase difference images are used to calculate flow, the
product of velocity and area, the presence of the static tissues in the
pixel also leads to an overestimation of vessel area which tends to
lead to an overestimation of flow. Although the two effects tend to
compensate, the net effect is usually an overestimation of flow, at
least in small vessels.
Typical phase contrast angiograms are shown in Figure 50.
These are sagittal views (lateral view looking through the ears) taken
at two different VENC values. The image on the right was taken at a
lower VENC to emphasize the slow flow in the arterio-venous
malformation seen in the upper right hand side of each image.
We have already discussed the fact that flowing blood gives a signal
void in spin echo sequences because the spins do not see both RF
pulses. We also mentioned the method of Foo in which the stimulated
echo sequence involving three 90 pulses was used to selectively image
flowing spins. The latter method is called a "tagging" method and is
one example of a time of flight technique.
Most current clinically used time of flight angiography relies on
another effect called "flow related enhancement". This effect relies
on the fact that if static spins see a series of RF pulses with short TR
interval they will not have time for their longitudinal magnetization
to recover. Soon the longitudinal magnetization becomes "saturated"
and tends toward a small equilibrium value. Conversely, spins
which are flowing into the field of view have full longitudinal
magnetization and will produce far greater signal and pass out of the
imaging slice before seeing too many rf pulses.
RF Saturation
1.0
RF Pulses
Longitudinal
Magnetization
(along B0) 0.5
Regrowth
Equilibrium
magnetization
TR
0
Time
Flow Related Enhancement
Imaging
Slice
Flow
0
1
2
Mz
Static
Tissue
Time
Flow Related Enhancement
Vessels
Static Tissue
Image from Anderson,
Edelman and Turski
Clinical MRA
Many of the angiographic techniques provide 3D data sets, including
the sequential 2D TOF technique described above. In order to produce
projection angiograms which look like their x-ray counterpart, it is
necessary to trace rays through the 3D volume at some angle of
interest. Several algorithms exist for dealing with the information
encountered along the various paths through the data set.
The most frequently used technique is called the "Maximum Intensity
Pixel (MIP) " method. In this technique only the value of the most
intense pixel is projected onto the image plane. This method is robust
and provides attractive vessel images. Its primary disadvantages are
that it underestimates vessel diameters and that vessel overlap is not
adequately represented.
Maximum Intensity Projection
1
Images from Anderson,
Edelman and Turski
Clinical MRA
5 2 10 6
2
7
3
10
Underestimation of vessel diameter is due to the fact that the small
vessel signal at the edge of the vessel does not compete favorably
with the more numerous maximum pixel signal candidates residing
in the static spin background pixels. Because these may be chosen
more often than the vessel signal, the edge of the vessel merges
with the background resulting in decreased apparent
width. Nevertheless, this technique often produces satisfactory
images and is the most widely used algorithm for generating
projection images from 3D MR angiographic data sets.
MIP Images from
3D Volume Data
axial
coronal
sagittal left
carotid
sagittal right
carotid
source image
F. Korosec
PhD Thesis
U. of Wisconsin
1991
Examples of Signal Saturation
2D TOF
3D TOF
3D
Slab
Keller and Saloner, TOF Flow Imaging, in
MRA Concepts and Applications, Potchen et al. eds.
The dependence of the signal on the number of RF pulses is shown in
Figure 51 for 10, 30, and 50 degree tip angles.
Notice that the larger the tip angle, the more rapidly the static tissue is suppressed.
The size of the tip angle must be chosen in accordance with the expected blood
velocity and slice thickness so that adequate saturation of static spins is achieved
but flowing blood signal does not become saturated.
The geometry for a 2D sequential slice time of flight technique is
shown in Figure 53.
The data is acquired one slice at a time. Therefore, in order to
acquire 128 phase encodings, 128 RF pulses are applied to the same
slice. This is more than adequate to saturate the static spins. The
number of RF pulses seen by the flowing spins depends on slice
thickness and velocity.
The signal produced by spins of various velocities are shown in Figure
54 for various tip angles in the case of a 5 mm slice. Note that for
spins traveling at 1 cm/sec, a small tip angle is optimal in order to
reduce saturation. As the velocity increases, the optimal tip angle
increases.
In the 2D TOF geometry it is possible to apply a 90 pulse and a
spoiler gradient above the slice in order to dephase flow coming
from the direction opposite from that of the vessels of interest. This
"SAT" technique is useful for separation of arterial from venous
flow signals.
Time of flight (and phase contrast) techniques are presently
implemented in 2D and 3D acquisition geometries. In the 3D
techniques, because larger volumes are used, rf saturation becomes a
more important consideration than in 2D geometries.
The spatial resolution of an MR angiogram is determined by the voxel
size. The voxel sizes for several geometries are shown in Figure 57.
As can be seen from the diagrams, the 3D data acquisition
sequences provide the smallest voxels. The direct projection
techniques have voxels which extend all the way through the region
of interest. In these applications it is customary to apply a mild
dephasing gradient in the projection direction in order to partially
dephase large objects while leaving small objects like vessels
relatively unaffected.
This results in a smaller overall detected signal, which means that
the signal representing the vessels can occupy a larger fraction of
the dynamic range of the A/D converter.
Increased spatial resolution is not the only advantage of smaller
voxels. As we mentioned before, there can be a distribution of
velocities within a vessel. The accumulated phase of the flowing
spins within a vessel can destructively interfere, leading to signal
loss. This is generally referred to as "intravoxel dephasing" and is
another reason why it is important to keep voxels as small as
possible.
There are three things which may be done to minimize intravoxel
dephasing. Aside from keeping the distribution of velocities small by
using small voxels, it is important to use the smallest possible TE
time so that dephasing has less time to occur.
Another method is called "gradient moment nulling". It is possible to
design gradient waveforms which refocus moving as well as static
spins.
The phase acquired by a by a moving spin is given by
=Gr r(t) dt
(69)
The position variable r(t) can be expanded into a series of terms
representing velocity, acceleration, jerk, and higher order terms as
r(t) = r0 + vt + 1/2 at2 + ...
(70)
It can be shown that if only velocity is present, the phase shift
produced by a gradient of amplitude 1,-2,1 as shown in Figure 58,
will refocus all spins moving with constant velocity in the direction
of the gradient, independent of the magnitude of this velocity.
Flow compensated gradient
G
t
It is also possible to design gradients which refocus acceleration as
well as velocity induced phase shifts. However these gradient require
longer TE times and lead to possible problems with higher order
motion terms which depend on the third and higher powers of t.
Generally velocity compensated gradients are worthwhile, but the
use of acceleration compensation is not worth the additional increase
in the required TE.
Contrast Enhanced MRA
Effect of Gadolinium on MRA Signal
1
Through
Plane
0.8
0
Gado 60
T1 = 50
0.6
Signal
0.4
In-Plane
15
0.2
0
0
T1 = 1000
60
0
0
5
10
A
15
Number of RF Pulses
20
Comparison of 2D TOF with
3D Contrast-Enhanced MRA
Prince, Grist and Debatin, 3D Contrast MR Angiography, 1997
Some Current MRI Contrast Agents
Knopp et al, J Magnetic Resonance Imaging, 1999
Artifacts due to Uneven
Weighting of Acquired Data
Injected
contrast
signal
Time
Overlap of Arteries and Veins
Fast Imaging
Data acquisition in k-space
(the spatial frequency domain)
ky
kx
The Mona Lisa in k-space
ky
kx
Low frequency Mona
k - space
ky
kx
High frequency Mona
k - space
Image
k-space
space
k-space Image
space
k-Space Flight Plans
Cartesian
Undersampled Projections
PR HyperTRICKS
VIPR
PR TRICKS
HyperVIPR
Keyhole Imaging*
Spock in k-space
Dynamic
Static
* Van Vaals et al. J. Magn. Reson. Imaging,
3,671-675 (1993)
Keyhole Acquisition
c(t)
Artery
Vein
Time
AAAAAAAAAAAAAAA
B
B
A
K-Space
A
B
Keyhole k-space
Keyhole Imaging
Low Resolution
Time
frames
Keyhole
Time
frames
3D TRICKS*
* Time Resolved Imaging
of
Contrast KineticS
Korosec F, Frayne R, Grist T, Mistretta C.
Time-resolved contrast-enhanced 3D MR angiography.
Magn Reson Med 1996; 36:345-351.
C
B
A
K-Space Segments
for
3D TRICKS
B
C
ky
Vein
Artery
•••
A
•••
Temporal Aperture
Keyhole
Frame
Time
B
A
C
A
C
A
B
C
A
B
TRICKS
7.5-10 s
B
C
3D TRICKS
Selected MIP images from a 27 frame series.
Frame time
Contrast dose
5.6 seconds
35 ml Gadodiamide.
3D TRICKS
512 x 128 x16
Frame Time
5.6 s
“We are using 3D TRICKS”
3D Muppet Show
Disney’s California Adventure Theme Park
High Resolution
Time Resolved MRA
Objectives
• Dynamic time series
• High spatial resolution
HyperTRICKS Acquisition
Artery
Vein
c(t)
Time
Dynamic Phase
Steady-State
A B A C AB A CA
...
D
kx
ky
kz
A BC D
VTRAC - Vessel Segmentation
Vessel Segmentation using
Time-Resolved ACquistion
Mazaheri, Du, Carroll, et al., Proc. 7th ISMRM, p. 2181
(1999).
ROI Selection
time
2D Cross Correlation Coefficients Formed from
Arterial and Venous Reference Curves
ccA
cc(x,y,z) =
ccV
S (x, y,z) S (x, y, z)R
i
i
i
i
R
S (x, y,z) S (x, y,z) R R
2 1/2
2
i
i
i
original
6
segmented
HyperTRICKS* with Low Frequency Vein Suppression
* 2 minute dynamic followed by 10 minute steady state*
4
4.6 s time frame
12 min MF
Vein suppressed MF
3
3
2.05
mm
0.19
mm
* using Gadomer 17- long lasting intravascular contrast agent
How Would We Do MRA If We Could
Start all Over?
Cartesian
MRA
Limitations of Cartesian
Acquisitions
For Cartesian acquisition the number
of pixels in y or z is directly proportional
to imaging time.
This is a serious limitation in the
presence of motion or dynamic
contrast variations as in contrastenhanced MRA
UW CME Imaging Course
Wollaston Lake Saskatchewan
August 1996
Dr. Reichelderfer “How
could we do virtual real
time endoscopy with MR”?
Cartesian vs. PR trajectories
ky
ky
kx
kx
FT (Spin-warp)
PR
Caution
Undersampled
Projection Holes!
Fully Sampled
k-space
Image
space
Undersampled
k-space
Image
space
Comparison of Conventional and PR Methods
Imaging Time
1
Cartesian
512 x
128
D. Peters PhD Thesis UW 1999
1
PR
512 x
128
4
Cartesian
512 x
512
PR TRICKS
72 projections
8x undersampling
2.6 s frames
384 x 256 x 18
3 times more resolution / time
than previous 3D TRICKS movie
K Vigen et al
PR HyperTRICKS
D
C
B
C
B
A
A
B
C
B
C
D
ABACABAC
Contrast Arrival
D
Steady State
PR HyperTRICKS
PR TRICKS
Sagittal
Coronal
J. Du et al
PR HyperTRICKS
1mm slices
Calfs from 2 station exam
0.94 mm pixels
4.1 sec frames
2.5 min exam
J. Du et al
PR-hyperTRICKS: Run-off Study
45 sec
59 sec
81 sec
Asymmetric enhancement: A-V transit time
T. Carroll, J. Du et al
Vastly Undersampled Isotropic PRojection
Imaging ( VIPR )
A full 3D projection sampling trajectory
Barger, Block et al.
Relative VIPR Noise vs Speedup Factor
22
11
5.5
2.7
256 x 256 x 256
Relative noise g
49
6
Speedup factors R
relative to Cartesian
49
5
4
22
3
11
5.5
2
2.7
1
5000
10000
15000
20000
25000
Number of projections angles
Preliminary Results
2
3
4
4 sec time
frames 256 x 256
x256 1.6 x 1.6
x 1.6 mm
6
7
8
Speedup relative to Cartesian = 33 Undersampled by 100x
W. Block et al
Arterial Time Frame
W. Block et al
Time Resolved VIPR
2 sec time frame intervals
40 x 24 x 40 elliptical FOV
256 x 256 x 256 1.6 x 0.94 x 1.6 mm
40 ml Gado at 3ml/s
24 s BH
Speedup relative to Cartesian = 33
Undersampled by 100x
E. Brodsky and W. Block
Time Resolved VIPR
2 sec time
frame intervals
256 x 256 x256
1.6 x 1.6 x 1.6 mm
24s BH
Speedup relative to
Cartesian = 33
Undersampled by 100x
E. Brodsky and W. Block
Jiang Du
VIPR + Bolus-Chase
initial results
Abdomen & calf:
Bolus-chasing + timeresolved
Thigh: separate injection
400 X 400 X 400 FOV
256 X 256 X 256 matrix
1.56 X 1.56 X 1.56 mm
All the stations are
time-resolved
15 s acq.
22 ml dose
2.0 ml/sec
56 s acq.
16 ml dose
2.0 ml/sec
56 s acq.
M.S.
VIPR+Bolus-Chase 4D imaging
MIP
3D
Jiang Du
Time
series
M.S.
Phase Contrast VIPR
Provides signal proportional
to velocity
TL GU et al
Basic VIPR PC vs 3D TOF
voxelsize = 0.24 mm3
4:48
voxelsize = 1 mm3
VIPR
10 minutes post contrast
384 x 384 x 384
10x speed gain relative to 3D TOF
3D TOF
5:40
No contrast
TL Gu et al
Basic VIPR PC vs Conventional PC
10X Advantage
4:35
Voxel
Size
0.83mm3
2.5mm3
7:11
TL Gu et al
Pulsatile Flow Phantom
Cartesian PC
PC VIPR
30cm/sec
VENC =50
Flow pump waveform
72 bpm
Images Courtesy of Sean Fain
PC VIPR
10-15 m post contrast
12
24
1.0 *24*24*12*5:48
= 12
S=
0.24*22*16* 8*4:48
.63
24
.63 .24 mm3
.63
Need to repeat at higher BW
and with eddy current correction
4:48
3843
3D TOF
8
22
.86
16
5:40
256 x 224 2 slabs 1.6 mm slices
1.0 mm3
.74
1.6
Questions Regarding 3D TOF vs PC VIPR
Image Quality
• Will longer PC VIPR TE’s, typically 5-6 ms
cause dephasing or will 0.25mm3 voxels reduce
velocity dispersion enough?
• Can we use contrast to go to higher BW for VIPR PC.
Velocity and Speed Resolved PC VIPR
Motivation:
It is the goal of PC VIPR to image all vessels in the
FOV with good SNR
When a single Venc is used, some vessels may alias
while others may be imaged with low SNR.
Fourier velocity encoding permits the use of the large gradients
required for good low velocity SNR without aliasing.
All applied gradient encodings contribute to the SNR in each velocity
bin.
Velocity-Resolved VIPR PC
1
2
11:12
P
3
2563
4
Sum of S/I Velocity Images
5
6
Sum of flows
Vel FOV =
+/- 60cm/s
Vres =17cm/s
A
4 x 2 enc steps
7
8
Sc =22
Speed Image
Formation of Anatomical Image from Speed Images
S1
S2
S3
S4
Sx
X
Y
Sy
Z
Sz
SMIP, Sum
or Matched Filter
Sum
of
Squares
Tian-Liang Gu M.S.
Cine’ VIPR PC: Introduction
Motivation: One isotropic 3D scan
to retrospectively measure all the
blood vessel waveforms in the
image volume.
VIPR trajectories are acquired for
each cardiac phase using
retrospective ECG gating.*
*Wieben O, PhD thesis UW-Madison, 2002
1
2
3
4
5
6
7
8
9
Cine’ PC VIPR
9 cardiac phases
2563
10 min scan Venc = 30
time series
Sum of all projections
Sum of All Projections Acquired During Time Series
Time
Series
Motion Correction Using VIPR
Projections as Navigators
O. Wieben et al.
Motion
Motion
with correction
No motion
Undersampled Projection Reconstruction
Spatial Resolution
SNR
X
Imaging Time
D. Peters - Thesis
Undersampled Projection
MRA
Imaging of Coronary Artery Plaque
Fayad, ZA et al.
500 µm in-plane resolution
Circ. 2000 (in press)
16 heart-beats imaging
X-ray angiogram
mild LAD disease
Concentric Thickened Wall
LAD Wall
LAD
RVOT
LV
RV
Fayad, ZA et al.
Circ. 2000 (In press)
~ 670X500 µm resolution
4 mm slice
~ 4 mm max wall thickness
Sign-Up Here
for
Wine/Grape Juice Study
•High fat diet
•Unlimited wine/juice
•Active sex life
•Free housing
•Free medical care
J.
Folts
Sorry-No further applications for
participation in this program are
being accepted.
That’s All Folks