THE SEARCH FOR A TREATMENT: RESEARCHING THE USE OF
advertisement

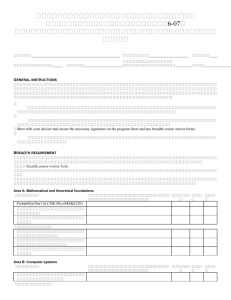
THE SEARCH FOR A TREATMENT: RESEARCHING THE USE OF MESENCHYMAL STEM CELLS THAT PRODUCE INSULIN-LIKE GROWTH FACTOR 1 AS A TREATMENT FOR AMYOTROPHIC LATERAL SCLEROSIS Michelle Renée Ohlson B.S., California State University, Sacramento, 2009 PROJECT Submitted in partial satisfaction of the requirements for the degree of MASTER OF ARTS in BIOLOGICAL SCIENCES (Stem Cell) at CALIFORNIA STATE UNIVERSITY, SACRAMENTO SPRING 2011 THE SEARCH FOR A TREATMENT: RESEARCHING THE USE OF MESENCHYMAL STEM CELLS THAT PRODUCE INSULIN-LIKE GROWTH FACTOR 1 AS A TREATMENT FOR AMYOTROPHIC LATERAL SCLEROSIS A Project by Michelle Renée Ohlson Approved by: __________________________________, Committee Chair Thomas Peavy, Ph.D. __________________________________, Second Reader Jan Nolta, Ph.D. __________________________________, Third Reader Thomas Landerholm, Ph.D. ____________________________ Date ii Student: Michelle Renée Ohlson I certify that this student has met the requirements for format contained in the University format manual, and that this project is suitable for shelving in the Library and credit is to be awarded for the Project. __________________________, Graduate Coordinator Susanne Lindgren, Ph.D. Department of Biological Sciences iii ________________ Date Abstract of THE SEARCH FOR A TREATMENT: RESEARCHING THE USE OF MESENCHYMAL STEM CELLS THAT PRODUCE INSULIN-LIKE GROWTH FACTOR 1 AS A TREATMENT FOR AMYOTROPHIC LATERAL SCLEROSIS by Michelle Renée Ohlson Amyotrophic lateral sclerosis (ALS) is a progressive, fatal neurodegenerative disease. Each year, about 5,000 people in the US are diagnosed with ALS. Treatment options for ALS patients are very limited with only one FDA approved drug that extends survival by a few months. Mesenchymal stem cells (MSCs) have created a lot of interest as a possible treatment option for many difficult to treat diseases. The purpose of this project is to characterize genetically altered MSCs that overproduce IGF-1 (MSC-IGF-1), as well as, GFP (MSC-GFP) as a control as a possible, future treatment for ALS. During this research, it was found that MSC-IGF-1 produced IGF-1 at 18µg/mL of supernatant, while MSC-GFP produced no detectable IGF-1. MSC-IGF-1 proliferated at a slower rate than MSC-GFP during a proliferation assay. MSC-IGF-1 was found to have decreased osteogenic differentiation potential as compared to MSC-GFP. MSC-IGF-1 migrated and proliferated slower than MSC-GFP during a motility assay. In conclusion, there is still a large amount of future experimentation to be completed before this treatment plan can become an option for ALS patients, but there is a lot of potential in this research bringing iv hope for an effective treatment for patients that fight a tragic and fatal disease with very limited options _______________________, Committee Chair Thomas Peavy, Ph.D. _______________________ Date v ACKNOWLEDGMENTS First, I would like to acknowledge and thank Dr. Thomas Peavy for his guidance and support during this program. Additionally, I would like to thank Dr. Thomas Landerholm for his guidance and support during the writing of this project. Second, I would like to acknowledge and thank Dr. Jan Nolta, Dr. Nanette Joyce, Fernando Fierro, Stefanos Kalomoiros, Dr. Scott Olson, Kari Pollock, and other members of the Nolta laboratory for their guidance and help during the research of this project. Finally, I would like to thank my husband, family, and friends for their unfaltering support throughout this program. Their love and support means the world to me. vi TABLE OF CONTENTS Page Acknowledgments....................................................................................................... vi List of Tables ............................................................................................................. viii List of Figures .............................................................................................................. ix INTRODUCTION .........................................................................................................1 MATERIALS AND METHODS ...................................................................................7 Transduction of Bone Marrow Derived MSCs and Vectors Used ................... 7 IGF-1 Enzyme-linked Immunosorbent Assay .................................................. 9 Proliferation Assay.......................................................................................... 10 Differentiation Assay ...................................................................................... 11 Motility Assay................................................................................................. 13 RESULTS ....................................................................................................................15 Transduction of Bone Marrow Derived MSCs ............................................... 15 IGF-1 Enzyme-linked Immunosorbent Assay ................................................ 17 Proliferation Assay.......................................................................................... 19 Differentiation Assay ...................................................................................... 21 Motility Assay................................................................................................. 25 DISCUSSION ..............................................................................................................27 Literature Cited ............................................................................................................32 vii LIST OF TABLES Page Table 1. Molecular components of experimental and control vectors ................................8 viii LIST OF FIGURES Page Figure 1. Transduction of bone marrow derived MSCs with doxycycline-inducible IGF-GFP (MSC-IGF-1) or GFP vector (MSC-GFP)........................................16 Figure 2. IGF-1 ELISA of supernatant collected after MSC-IGF-1 were in doxycycline media for 24 hours........................................................................18 Figure 3. Proliferation assay to compare proliferation rates of MSC-IGF-1 and MSC-GFP after cell culture in doxycycline media ...........................................20 Figure 4. Osteogenic differentiation assay after 21 days under doxycycline osteogenic cell culture conditions .....................................................................22 Figure 5. Adipogenic differentiation assay after 14 days under doxycycline adipogenic cell culture conditions ....................................................................24 Figure 6. Motility assay to determine the rate of cell motility and proliferation between MSC-IGF-1 and MSC-GFP after culture in doxycycline media ........26 ix 1 INTRODUCTION Mesenchymal stem cells (MSCs) have created a lot of interest in the scientific community as a possible treatment option for many diseases that are currently untreatable or difficult to treat including, but not limited to, Huntington’s disease, Parkinson’s disease, and muscular dystrophy. This interest in MSCs is due to the fact that MSCs are immune-privileged and have an intrinsic paramedic response when injected into the body (1). In previous studies, MSCs injected into the body have been shown to travel to the damaged parts of the body, particularly to hypoxic and inflamed tissues (1). Once the MSCs have reached damaged tissues in the body, they are known to produce many cytokines and growth factors like hepatocyte growth factor, fibroblast growth factor 2, vascular endothelial growth factor, and insulin-like growth factor 1 that aid in the healing of damaged tissues in the body (1). Additionally, MSCs have the ability to be genetically altered to produce specific proteins or growth factors that have the potential to heal or stop the further degeneration of the diseased tissues within the body (1). In the lab, MSCs are easily extracted and grown from bone marrow samples, as well as, from fat tissue samples from liposuctions. MSCs could be the tool needed by the scientific community to create effective treatment options, and possibly cures, for many diseases that are currently difficult to treat and/or incurable like those mentioned previously. More specifically, MSCs hold a lot of promise in the future treatment of neurological diseases that affect the central nervous system (CNS) like amyotrophic lateral sclerosis (ALS). 2 ALS, also known as Lou Gehrig’s disease, is a progressive, fatal neurodegenerative disease (2). ALS is a motor neuron disease, characterized by the degeneration and subsequent loss of motor neurons (2). In ALS, the upper and lower motor neurons found in the brain, brain stem, and spinal cord are affected specifically (2). Within the body, upper motor neurons in the brain carry signals to lower motor neurons in the spinal cord that continue the signals to the voluntary muscles (3). As the muscles receive fewer signals from the brain and/or spinal cord, the result is continued muscle weakness leading to muscle atrophy of voluntary muscles and the loss of voluntary movement for ALS patients (3). The clinical presentation of ALS patients can vary widely, but there are some common symptoms seen among patients (2). Some of these symptoms include, but are not limited to: muscle weakness, muscle twitching called fasciculations, muscle cramping, and muscle stiffness also known as spasticity (3). Symptom onset is asymmetric and often begins in the hands and feet, then progress to affect the muscles of the trunk of the body (3). Additionally, there is a bulbar form of ALS that affects the face, mouth and tongue of ALS patients (4). Symptoms of the bulbar form of ALS include motor speech impairments known as dysarthria with poor verbal articulation, as well as, difficulty swallowing (4). Progression of the disease inevitably leads to death by respiratory failure and often occurs within two to three years in bulbar ALS patients and three to five years in limb onset ALS patients (4). Diagnosis of ALS patients is difficult and based on clinical criteria (2). There is no definitive test or biomarker for ALS (2). Doctors must rule-out other causes of treatable motor neuron 3 disease, and the patient’s symptoms must progress both over time and over areas of the body before an ALS diagnosis is given (2). Each year, about 5,000 people in the US are diagnosed with ALS (2). Of those diagnosed with ALS, 90% of patients have developed ALS for unknown reasons and are labeled as sporadic ALS cases (4). The remaining 10% of those diagnosed each year in the US have a genetically transmitted familial form of ALS (fALS) (4). Of those patients with fALS, 20% will carry a mutation in the Copper Zinc Superoxide Dismutase 1 (SOD1) gene (4). To date, there are at least 120 identified mutations in the SOD1 gene that are known to cause ALS (5). It is hypothesized that these mutations create a toxic gain of function in SOD1, caused by the misfolding of the SOD1 protein likely leading to endoplasmic reticulum stress and motor neuron cell apoptosis (5). This endoplasmic reticulum stress induced by the accumulation of SOD1 misfolded proteins activates the unfolded protein response pathway, which is caused by an increase in the amount of misfolded proteins in the endoplasmic reticulum (6). The unfolded protein response pathway leads to the induction of chaperones, stress sensor kinases, and apoptotic mediators, as well as, the activation of the endoplasmic reticulum associated degradation system (6, 9). If there continues to be a buildup of misfolded proteins in the endoplasmic reticulum despite the activation of the unfolded protein response and endoplasmic reticulum associated degradation system, then apoptotic cell death occurs (9). This phenomenon has been seen in the cell and rodent models of fALS, as well as, in the spinal cord of human ALS patients (6). Although there is some information known on 4 the mechanisms in fALS, the ALS disease pathophysiology is still largely unknown, but appears to be multifactorial (13). Treatment options for ALS patients are very limited with only one FDA approved drug, Riluzole, which extends survival by only a few months (10). Riluzole must be taken daily with the possibility of many detrimental side effects with some examples being lowered ability to fight infection, muscle weakness and aches, fatigue, and loss of appetite (11). Unfortunately, patients that qualify for treatment with Riluzole must take it without the possibility of knowing whether it is prolonging their life because there is no way to gauge if it is working or not (13). During recent research of possible future ALS treatments, growth factors have been at the center of many experiments (10, 15). Growth factors are proteins that are necessary for the survival of neurons, as well as, neuron and support cell differentiation during development (6). The growth factor, insulin-like growth factor 1 (IGF-1) has been considered in the possible treatment of ALS by many researchers. In the body, IGF-1 binds to IGF-binding proteins and then binds the IGF-1 receptor (7). IGF-1 receptors have been shown to have high expression during tissue development and expression remains elevated in motor neurons after development (7). Previously, IGF-1 and other growth factors have been tested using experimental models of ALS (10, 16, 17, 18). The most common rodent experimental model is the SOD1G93A mouse model of ALS (8, 19). This model uses transgenic mice that have a mutated human copy of the SOD1 gene that develops a disease similar to fALS (8, 19). In rodent models of ALS that carry SOD1 mutations, the results have shown improvements in motor neuron survival and neuromuscular function in the animals being 5 tested (10, 16, 17, 18). However, human trials with ALS patients using classic protein delivery methods have shown a lack of improvement in neuromuscular function and patient survival (10, 12). These negative results could be due to inadequate dosing, issues with the protein crossing the blood-brain barrier, the short half-life of the protein, and/or the side effects of the protein in non-targeted areas of the body (10). For many neurological diseases, MSCs that are genetically altered to produce specific proteins or growth factors like IGF-1 are a promising alternative to classic protein delivery methods. This is because they have the potential to be injected directly into the CNS through a spinal tap or surgical means to promote healing and/or halt further degeneration of tissues through their innate paramedic properties and the continuous production and secretion of specific proteins like the growth hormone, IGF-1. There has previously been a Phase 1 clinical trial completed where ALS patients had MSCs surgically implanted into the CNS to determine the safety of this procedure (14). This study showed no deaths or serious adverse events related to the surgical transplantation of MSCs into the CNS further showing the promise of MSCs in the treatment of neurological diseases (14). The purpose of this project is to characterize genetically altered MSCs that overproduce IGF-1, as well as, GFP as a control. The ultimate goal of this project is to create a relevant therapy for ALS patients using MSCs that produce prolonged and targeted IGF-1 secretion thus changing the microenvironment of the motor neurons thereby slowing disease progression and improving quality of life. The broader significance of this experimental research is to increase future treatment options for ALS 6 patients while also evaluating the potential of mesenchymal stem cell drug delivery in the treatment of neurodegenerative diseases. 7 MATERIALS AND METHODS Transduction of Bone Marrow Derived MSCs and Vectors Used The purpose of MSC transduction was to create MSCs that stably express either the IGF-GFP vector (MSC-IGF-1) or GFP control vector (MSC-GFP). Both vectors are based on the third-generation lentiviral vector pCCLc backbone with tetracycline response elements (TRE). The IGF-GFP retroviral construct is: pCCLc-TREIGF1/p2A/EGFP-PGK-rtTA and is 8,948 bases in size. The GFP retroviral construct is pCCLc-TRE-EGFP-PGK-rtTA and is 8,417 bases in size. Both vectors are described in detail below in Table 1. Additionally, both vectors are under the control of a doxycycline-inducible promoter ensuring that the transduced cell only produces the vector product when there is doxycycline in the cell culture media. To transduce MSCs, first, cultured MSCs were grown in normal media (HyClone MEMα with 10% Atlanta Biologicals Premium Select FBS). After cultured MSCs reach 80% confluency, they were plated into six well plates at 50,000 cells per well. Two days after plating, cells were incubated with the desired vector in a viral mixture (normal media, 0.002% protamine sulfate, and virus). After transduced cells become 80% confluent, they were plated for future experiments or cryopreserved in liquid nitrogen. 8 Table 1. Molecular components of experimental and control vectors. Elements in vectors used1 Definition of the element pCCLc Lentiviral vector backbone with cytomegalovirus promoter driving high levels of expression TRE Tetracycline response element which must be bound by doxycycline-bound rtTA allowing for gene expression IGF-1 Insulin-like growth factor 1 gene segment p2A Linker segment EGFP Green fluorescent protein gene segment PGK Housekeeping phosphoglycerate kinase promoter rtTA Tet-on advanced transactivator which must be bound by doxycycline before binding TRE allowing for gene expression 1 Experimental IGF-1 vector (pCCLc-TRE-IGF1/p2A/EGFP-PGK-rtTA); Control GFP vector (pCCLc-TRE-EGFP-PGK-rtTA). 9 In order to know the amount of the desired virus needed to transduce 50,000 cells, a previous titer using GFP expression on the FC500 FACS machine was performed. To complete the titer, cells are plated at a known cell number into a 12 well cell culture dish and are transduced at various viral concentrations to determine what concentration of vius produces a high percentage of GFP positive cells. These transduced cells are then run through the FC500 flow cytometer to determine the amount of GFP positive cells. To complete this, cells were released from the plate with the protease, trypsin, before being centrifuged to create a cell pellet. The media surrounding the cell pellet was decanted and the cell pellet was re-suspended in PBS prior to being run through the FC500 flow cytometer to determine the amount of GFP positive cells. IGF-1 Enzyme-linked Immunosorbent Assay The purpose of the enzyme-linked immunosorbent assay (ELISA) for the IGF-1 protein was to determine the amount of IGF-1 expressed per cell after transduction with either the IGF-GFP vector or GFP control vector. This was done in order to figure out the number of cells needed for treatment dosages for future mice experimentation and, possibly, clinical trials. Additionally, three different doxycycline medias with three doxycycline concentrations were used to see how much IGF-1 was produced under different doxycycline concentrations. To achieve this, previously transduced MSCs were grown in normal media. After cells became 80% confluent, they were plated into 12 well cell culture plates at 4,000 cells per well in normal media. Two days after plating, media was changed to media with lowered FBS concentrations to prevent it from affecting the 10 results and doxycycline medias with three different doxycycline concentrations of 2X, 1X, and 0.5X (HyClone MEMα with 2% Atlanta Biologicals Premium Select FBS with doxycycline at 4µL/mL, HyClone MEMα with 2% Atlanta Biologicals Premium Select FBS with doxycycline at 2µL/mL, HyClone MEMα with 2% Atlanta Biologicals Premium Select FBS with doxycycline at 1µL/mL). Supernatant from each condition was collected after 24 hours incubation with the transduced cells. The IGF-1 ELISA was completed following the instructions from the R & D Systems Human IGF-1 ELISA Kit (DG100). According to these instructions, first, add assay diluent, then sample or provided standard to each well of one of the 96 well plate provided and incubate. After incubation, aspirate and wash each well with wash buffer before incubation with IGF-1 conjugate. Then, the wash step is repeated before addition and incubation with the substrate solution. Finally, the stop solution is added and the plate is read using a microplate reader set at the wavelength of 450 nm. Proliferation Assay The purpose of the proliferation assay was to determine and compare the proliferation rate of MSCs expressing either the IGF-GFP vector or GFP control vector. To achieve this, previously transduced MSCs were grown in normal media. After cells became 80% confluent, they were released from the plate with the protease, trypsin, and counted with a hemacytometer prior to being plated into 12 well cell culture plates at 4,000 cells per well in normal media. Two days after plating, media was changed to doxycycline media (HyClone MEMα with 10% Atlanta Biologicals Premium Select FBS 11 with doxycycline at 2µL/mL). The first time point of the assay is called Day 0 and is two days after media was changed from normal media to doxycycline media. The rest of the time points occurred every 48 hours and were called Day 2, 4, 6, 8, and 10. During each time point, two wells of the previously plated 12 well cell culture plates were trysinized and counted in duplicate using trypan blue in a standard hemocytometer. Additionally, at each time point, the sample was run through the FC500 flow cytometer to determine the amount of GFP positive cells. To complete this, cells were released from the plate with the protease, trypsin, before being centrifuged to create a cell pellet. The media surrounding the cell pellet was decanted and the cell pellet was re-suspended in PBS prior to being run through the FC500 flow cytometer to determine the amount of GFP positive cells. Differentiation Assay The purpose of the differentiation assay was to determine and compare the ability for MSCs expressing either the IGF-GFP vector or GFP control vector to differentiate into either adipocytes or osteocytes. To achieve this, previously transduced MSCs were grown in normal media. After cells became 80% confluent, they were released from the plate with the protease, trypsin, and counted with a hemacytometer prior to being plated into 6 well cell culture plates at 50,000 cells per well in normal media. Two days after plating, media was changed to doxycycline media (HyClone MEMα with 10% Atlanta Biologicals Premium Select FBS with doxycycline at 2µL/mL). Two days later, doxycycline media was changed to either osteogenic (HyClone MEMα with 10% Atlanta 12 Biologicals Premium Select FBS, 0.01% betaglycerol phosphate, 0.01% ascorbic acid, 0.0002% dexamethasone) or adipogenic differentiation media (HyClone MEMα with 10% Atlanta Biologicals Premium Select FBS, 0.001% 3-Isobutyl-1-methylxanthine (IBMX), 0.001% dexamethasone, 0.001% indomethacin). The osteogenic and adipogenic medias were made in the laboratory using the necessary components. For cells incubated in osteogenic media, media changes were completed every 3 days until day 21 in culture was reached. On day 21, RNA was collected and processed following the Qiagen RNeasy Kit instructions. The stored RNA was made into cDNA following the Quantitect Reverse Transcription Kit instructions. The stored cDNA was then used to complete qPCR for osteogenic markers bone sialoprotein (BSP) and osteocalcin (OCN). Additionally, on day 21 in osteogenic media, the alkaline phosphatase (ALP) concentration was determined. To achieve this, cells are trypsinized and centrifuged to create a cell pellet. After the cell pellet is made, the media is decanted and the cells are incubated in cell lysis solution (1.5M Tris-HCl solution with 1.0mM ZnCl2, 1.0mM MgCl2, 1% Triton X-100). After incubation, the cells are centrifuged to create a cell pellet prior to incubation with p-nitrophenylphosphate (p-NPP). After incubation, cells are read using a microplate reader set at the wavelength of 405 nm. Additionally, the protein concentration must be calculated by comparing to bovine serine albumin (BSA) standards. First, samples are diluted 1:5 with molecular grade water. Next, 10µL of sample or standard is added to 200µL Coomassie and cells are read using a microplate reader set at the wavelength 595 nm. Finally, ALP concentration is determined as “µg p-NPP/µg of protein”. 13 For cells incubated in adipogenic media, media changes were completed every 3 days until day 14 in culture was reached. On day 14, RNA was collected and processed following the Qiagen RNeasy Kit instructions. The stored RNA was made into cDNA following the Quantitect Reverse Transcription Kit instructions. The stored cDNA was then used to complete qPCR for adipogenic markers peroxisome proliferator-activated receptor gamma (pparg) and fatty acid binding protein 4 (FABP4). Additionally, on day 14 in adipogenic media, the lipid structures were stained with the nonfluorescent lipid stain nile red. To achieve this, cells are trypsinized and centrifuged to create a cell pellet. After the cell pellet is made, the media is decanted and a nile red solution (0.01% nile red in PBS) is incubated with the cells in darkness. After incubation, cells are centrifuged to create a cell pellet, then the media is decanted and cells are resuspended in PBS. Finally, the nile red stained cells are run in the FC500 flow cytometry and to determine the nile red positive percentage. Motility Assay The purpose of the motility assay was to determine and compare the rate of cell migration and proliferation of MSCs expressing either the IGF-GFP vector or GFP control vector. To achieve this, previously transduced MSCs were grown in doxycycline media. After cells became 80% confluent, they were released from the plate with the protease, trypsin, and counted with a hemacytometer prior to being plated into 24 well cell culture plates at 30,000 cells per well in doxycycline media. There is a defined area within the well of the cell culture plate that is absent of MSCs. Under a microscope, this 14 area is seen as a line across the middle of the well of the cell culture plate that is absent of MSCs. To create this define area absent of cell growth, a plastic divider is positioned in the well of the cell culture plate before MSCs were plated. MSCs are then plated in doxycycline media with 15,000 cells on each side of the divider for a total of 30,000 cells per well. Twenty four hours after plating, the dividers are carefully removed to prevent disturbing plated MSCs along the edge of this define area. The first time point of the assay is called Hour 0 and occurs when the dividers are removed. The rest of the time points are at hours 3, 6, 12, 24, and 30. At each time point, pictures are taken under the microscope at the area where the defined area without cell growth is within the well of the cell culture plate. The rate of closure of the defined area without cell growth was determined by TScratch computer software, available for download from the Computational Science and Laboratory of the ETH Zurich University website (www.cselab.ethz.ch). 15 RESULTS Transduction of Bone Marrow Derived MSCs Cultured MSCs were transduced with either the doxycycline-inducible IGF-GFP vector (MSC-IGF-1) or GFP control vector (MSC-GFP) to produce MSCs that stably express either vector product within the transduced cells. After transduction, MSCs were cultured in doxycycline media. After three days in doxycycline media, MSC-IGF-1 were shown to have 30% GFP positive cells while MSC-GFP were shown to have 80% GFP positive cells after transduction with 8µLof either lentivirus as seen in Figure 1. When discussing MSC-IGF-1, GFP positive cells represent IGF-1 secreting MSCs. Additionally, a picture of MSC-GFP can be seen in Figure 1B and MSC-IGF-1 can be seen in Figure 1C. 16 Figure 1. Transduction of bone marrow derived MSCs with doxycycline-inducible IGFGFP (MSC-IGF-1) or GFP vector (MSC-GFP). (A) Transduction of MSCs with IGFGFP or GFP control vector. (B) Representative field of GFP positive cells in MSC-GFP (100X magnification). (C) Representative field of GFP positive cells in MSC-IGF-1 (100X magnification). 17 IGF-1 Enzyme-linked Immunosorbent Assay To determine the amount of IGF-1 expressed per cell after transduction in MSCIGF-1 or MSC-GFP cells were grown in doxycycline media and supernatant was collected after 24 hours in culture. Additionally, three different doxycycline concentrations were used to compare the amount of IGF-1 produced when the doxycycline-inducible promoter is induced with cell culture media with varying doxycycline concentrations. The supernatant collected was used in the R and D Systems Human IGF-1 ELISA Kit. It was found that MSC-GFP produced no detectable IGF-1 with or without doxycycline media. Additionally, it was found that MSC-IGF-1 with normal (1X) doxycycline media produced IGF-1 at 18µg/mL of supernatant as seen in Figure 2. Additionally, there was minimal dose dependence seen in the supernatant on cells in cultures with 2X and 0.5X doxycycline concentrations as seen in Figure 2. 18 Figure 2. IGF-1 ELISA of supernatant collected after MSC-IGF-1 were in doxycycline media for 24 hours. This demonstrated the amount of IGF-1 protein produced by MSCIGF-1 in two donor cell lines with three different concentrations of Doxycycline media. 19 Proliferation Assay A proliferation assay was completed to compare the proliferation rate of MSCIGF-1 and MSC-GFP. It was found that MSC-IGF-1 proliferated at a slower rate than MSC-GFP as seen in Figure 3A. Additionally, MSC-IGF-1 showed a progressive decrease in GFP positive cells as proliferation increases and time passes as seen in Figure 3B. Additionally, MSC-GFP showed an equal amount of GFP positive cells as proliferation increases and time passes as seen in Figure 3B. 20 Figure 3. Proliferation assay to compare proliferation rates of MSC-IGF-1 and MSCGFP after cell culture in doxycycline media. (A) The average proliferation rate from two donor cell lines of MSC-IGF-1 and MSC-GFP. (B) The average GFP positive cells during proliferation of two donor cell lines of MSC-IGF-1 and MSC-GFP. 21 Differentiation Assay A differentiation assay was completed to compare the ability of MSC-IGF-1 and MSC-GFP to differentiate into osteocytes and adipocytes. After 21 days in osteogenic media, MSC-IGF-1 showed decreased ALP concentration as compared to MSC-GFP as seen in Figure 4A. 22 Figure 4. Osteogenic differentiation assay after 21 days under doxycycline osteogenic cell culture conditions. (A) The ALP concentration of MSC-IGF-1 and MSC-GFP after osteogenic differentiation. (B) The BSP mRNA levels in MSC-IGF-1 and MSC-GFP in two donor cell lines after osteogenic differentiation. (C) The OCN mRNA levels in MSCIGF-1 and MSC-GFP in two donor cell lines after osteogenic differentiation. 23 Additionally, BSP and OCN mRNA levels were decreased in MSC-IGF-1 as compared to MSC-GFP as seen in Figure 4B and Figure 4C. After 14 days in adipogenic media, PPARG and FABP4 mRNA levels were consistent between MSC-IGF-1 and MSC-GFP as seen in Figure 5A and Figure 5B. 24 Figure 5. Adipogenic differentiation assay after 14 days in doxycycline adipogenic cell culture conditions. (A) The PPARG mRNA levels in MSC-IGF-1 and MSC-GFP in two donor cell lines after adipogenic differentiation. (B) The FABP4 mRNA levels in MSCIGF-1 and MSC-GFP in two donor cell lines after adipogenic differentiation. 25 Motility Assay A motility assay was completed to compare the rate of cell migration and proliferation of MSC-IGF-1 and MSC-GFP. It was found that MSC-GFP showed a faster rate of migration and proliferation as compared to MSC-IGF-1 in both donor cell lines as seen in Figure 6A and Figure 6B. Additionally, pictures of MSC-GFP and MSC-IGF-1 at various time points can be seen in Figure 6C. 26 Figure 6. Motility assay to determine the rate of cell motility and proliferation between MSC-IGF-1 and MSC-GFP after culture in doxycycline media. (A) The time it takes to fill in a defined space in MSC-IGF-1 and MSC-GFP in 11.6 donor cell line. (B) The time it takes to fill in a defined space in MSC-IGF-1 and MSC-GFP in 11.6 donor cell line. (C) Images of MSC-IGF-1 and MSC-GFP at various time points during the motility assay (100X magnification). 27 DISCUSSION First, cultured MSCs were transduced with either the doxycycline-inducible IGFGFP vector (MSC-IGF-1) or GFP control vector (MSC-GFP) to create MSCs that stably express either vector product when there is doxycycline in the cell culture media. MSCIGF-1 had 30% GFP positive cells while MSC-GFP had 80% GFP positive cells after transduction with 8µLof either lentivirus. Even though MSC-IGF-1 had a much lower percentage of GFP positive cells than MSC-GFP, this was expected since the IGF-GFP vector is larger and more complex and, therefore, harder to transduce MSCs with than the GFP control vector. In the future, these transduction methods will continue to be used. Next, to determine the amount of IGF-1 expressed per cell after transduction in MSC-IGF-1 or MSC-GFP, supernatant was collected after 24 hours in cell culture conditions. It was found that MSC-GFP did not produce any detectable amounts of IGF1 in cell culture media with or without doxycycline in the cell culture media. It was found that MSC-IGF-1 produced IGF-1 at 18µg/mL of supernatant when there was 1X concentration of doxycycline in the media at 2µL/mL of media. Additionally, two other concentrations of doxycycline were used and it was found that there was minor dose dependence. In the 2X concentration of doxycycline in the media at 4µL/mL of media, there was a slightly elevated amount of IGF-1 produced as compared to the 1X concentration, but it was not statistically significant. In the 0.5X concentration of doxycycline in the media at 1µL/mL of media, there was a slight lower amount of IGF-1 produced as compared to the 1X concentration, but it was also not statistically significant. 28 In future experimentation, we would like to test additional concentrations of doxycycline that are lower than those tested previously in an attempt to find a difference in IGF-1 production as related to varying doxycycline concentrations that are statistically significant. Additionally, we would like to repeat this experiment with sorted MSC-IGF1 and MSC-GFP. This would allow us to test a homogenous population of cells instead of a mixed population of transduced and non-transduced cells. In order to sort cells, we would need to transduce cells with either the doxycycline-inducible IGF-GFP vector (MSC-IGF-1) or GFP control vector (MSC-GFP) to create MSCs that stably express either vector product when there is doxycycline in the cell culture media. These transduced cells can then be sorted for GFP positive cells in both heterogeneous cell populations. By doing this, we can create a homogeneous mixture of GFP positive cells only for both cell populations. A proliferation assay was completed to compare the proliferation rate of MSCIGF-1 of and MSC-GFP. It was found that MSC-IGF-1 proliferated at a slower rate than MSC-GFP. It was also found that MSC-IGF-1 showed a progressive decrease in GFP positive cells with MSC-GFP showed an equal amount of GFP positive cells as proliferation increases and time passes. We have hypothesized that the amount of GFP positive cells decrease as proliferation increases due to faster proliferation of nontransduced MSCs in the heterogenous mixture of cells as compared to transduced, GFP positive cells. In future experiments, we would like to repeat this experiment with sorted MSC-IGF-1 and MSC-GFP. This would allow us to test a homogenous population of cells instead of a mixed population of transduced and non-transduced cells. The methods 29 described above would be used to sort cells for GFP positive cells to create homogeneous cell populations. A differentiation assay was completed to compare the ability of MSC-IGF-1 and MSC-GFP to differentiate into osteocytes or adipocytes. For differentiation into osteocytes, it was found that MSC-IGF-1 showed decreased ALP concentration as compared to MSC-GFP. The mRNA levels for osteogenic markers, BSP and OCN, were decreased in MSC-IGF-1 as compared to MSC-GFP. For differentiation into adipocytes, it was found that mRNA levels were consistent between MSC-IGF-1 and MSC-GFP. In future experiments, we would like to repeat the differentiation into osteocytes and use additional osteogenic mRNA markers to see if there continues to be differences between MSC-IGF-1 and MSC-GFP. Since there were no significant differences in adipocyte differentiation between MSC-IGF-1 and MSC-GFP, there are no future experiments planned. Finally, a motility assay was completed to compare the rate of cell migration and proliferation of MSC-IGF-1 and MSC-GFP by looking at the time it takes to fill a define space vacant of cell growth for both cell types. It was found that MSC-GFP showed a faster rate of migration and proliferation as compared to MSC-IGF-1. It is thought that this occurred because MSC-GFP proliferates faster than MSC-IGF-1 as shown in the proliferation assay. For future experiments, we would like to repeat this experiment with additional bone marrow donors, as well as, with a homogeneous population of sorted MSC-IGF-1 and MSC-GFP to see if that affects the results. The methods described 30 above would be used to sort cells for GFP positive cells to create homogeneous cell populations. The purpose of this project was to characterize genetically altered MSCs that overproduce IGF-1, as well as, GFP as a control. The ultimate goal of this project was to create a relevant therapy for ALS patients using MSCs that produce prolonged and targeted IGF-1 secretion thus changing the microenvironment of the motor neurons and thereby slowing disease progression and improving quality of life. Previous research has shown that using classical protein delivery methods of IGF-1 in humans, like subcutaneous injections, did not show increased patient survival or neuromuscular function (10, 12). This is thought to have occurred due to inadequate dosing, problems with IGF-1 passing the blood-brain barrier, the short half-life of IGF-1, and/or side effects of IGF-1 in non-targeted areas of the body (10). Additionally, IGF-1 has shown some positive effects in the rodent models of ALS that carry mutations in the SOD1 gene when injected into the muscles of these animals (10). Clearly, these positive effects seen in the rodent models of ALS have not easily translated into humans when experimentation has previously been done. There is a potential problem with translating a relatively small number of muscle injections in the ALS mouse to the possibly high number of injections needed in a patient with ALS if this experimental method became a treatment option in the future. Additionally, there is the question of whether injections into easily accessible muscles of the human body will positively affect the diaphragm, which is ultimately the muscle that leads to respiratory failure and death in ALS patients once it becomes affected by the disease and can’t function properly (13). 31 The ultimate goal of the research presented here is to create a treatment option for ALS patients where MSCs that stably express IGF-1 are transplanted into the CNS and allowed the positively affect the microenvironment of the disease affected motor neurons to increase muscle function, quality of life, and patient survival. This potential treatment plan could bypass many of the problems previously discussed that are associated with other experimental treatment plans. In conclusion, there is still a large amount of experimentation to be completed before this treatment plan can become an option for ALS patients, but there is a lot of potential in this research bringing hope for an effective treatment for patients that fight a tragic and fatal disease with very limited options. 32 LITERATURE CITED 1. Joyce, N., Annett, G., Wirthlin, L., Olson, S., Bauer, G., Nolta, J. “Mesenchymal stem cells for the treatment of neurodegenerative disease”. (2010) Regen Med. 5(6): 933-946. 2. ALS Organization. 1 Nov. 2009 http://www.alsa.org 3. National Institute of Neurological Disorders and Stroke. 1 April 2010 http://www.ninds.nih.gov/disorders/amyotrophiclateralsclerosis 4. Wijesekera, L., Leigh, P. “Amyotrophic Lateral Sclerosis”. (2009) Orphanet Journal of Rare Diseases. 4(3): 350-372. 5. Culotta, V., Yang M., O’Halloran, T. “Activation of Superoxide Dismutases: Putting the medal to the pedal”. (2006) Biochim Biophys Acta. 1763(7): 747758. 6. Mori, A., Yamashita, S., Uchino, K., Suga, T., Ikeda, T., Takamatsu, K., Ishikazi, M., Koide, T., Kimora, E., Mita, S., Maeda, Y., Uchino, M. “Derlin-1 overexpression ameliorates mutant SOD1-induced endoplasmic reticulum stress by reducing mutant SOD1 accumulation”. (2011) Neurochemistry International 58(3): 344-353. 7. Corbo, M., Lunetta, C., Magni, P., Dozio, E., Ruscica, M., Adobbati, L., Silani, V. “Free insulin-like growth factor (IGF)-1 and IGF-binding proteins -2 and -3 in serum and cerebrospinal fluid of amyotrophic lateral sclerosis patients”. (2010) European Journal of Neurology 17: 398-404. 33 8. Leichsenring, A., Linnartz, B., Zhu, X., Lubbert, H., Stichel, C. “Ascending neuropathology in the CNS of a mutant SOD1 mouse model of amyotrophic lateral sclerosis”. (2006) Brain Research 1096: 180-195. 9. Lai, E., Teodoro, T., Volchuk, A. “Endoplasmic Reticulum Stress: Signaling the Unfolded Protein Response”. (2007) Physiology 22(3): 193-201. 10. Suzuki, M., Svendson, C. “Combining growth factor and stem cell therapy for Amyotrophic lateral sclerosis”. (2008) Trends in Neurosciences 31(4): 192-198. 11. Riluzole PubMed Health. 9 April 2011 http://www.ncbi.nlm.nih.gov/pubmedhealth/PMH0000978 12. Sorenson, E., et al. “Subcutaneous IGF-1 is not beneficial in 2-year ALS trial”. (2008) Neurology 71: 1770-1775. 13. Joyce, Nanette. Personal Communications. 14. Mazzini, L., et al. “Mesenchymal stem cell transplantation in amyotrophic lateral sclerosis: A Phase 1 clinical trial”. (2010) Experimental Neurology 223: 229-237. 15. Funakoshi, H., et al. “ALS and neurotrophic factors – HGF as a novel neurotrophic and neuroregenerative factor”. (2007) Brain Nerve 59: 1195-1202. 16. Suzuki, M., et al. “Direct muscle delivery of GDNF with human mesenchymal stem cells improves motor neuron survival and function in a rat model of familial ALS”. (2008) Mol. Ther. 16: 2002-2010. 17. Kadoyama, K., et al. “Hepatocyte growth factor (HGF) attenuates gliosis and motoneuronal degeneration in the brainstem motor nuclei of a transgenic mouse model of ALS”. (2007) Neurosci. Res. 59: 446-456. 34 18. Nagano, I., et al. “Therapeutic benefit of intrathecal injection of insulin-like growth factor-1 in a mouse model of amyotrophic lateral sclerosis”. (2005) J. Neurol. Sci. 235: 61-68. 19. Julien, JP., et al. “Transgenic mouse models of amyotrophic lateral sclerosis”. (2006) Biophys. Acta. 1762: 1013-1024.