Document 16071290
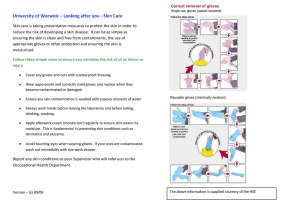
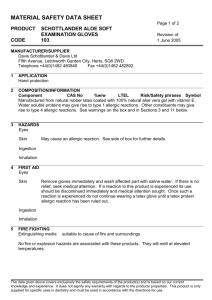
advertisement

1 Office of the Institutional Animal Care and Use Committee (909) 469-5241; FAX (909) 469-5577 OCCUPATIONAL HEALTH AND SAFETY PROGRAM (OHSP) FOR PERSONNEL WORKING WITH OR AROUND LABORATORY ANIMALS U.S. Department of Agriculture regulations, Public Health Service Policy and the National Institutes of Health Guide for the Care and Use of Laboratory Animals require that all institutions receiving public funds establish an OHSP for persons who may come into contact with laboratory animals, their tissues or their allergens. Persons who work with or around laboratory animals are at some risk and the IACUC has the responsibility to verify that such persons are enrolled in the OHSP program before they are permitted to work with or around animals. The purpose of this policy is not only to prevent or minimize the risk of illness but to provide for early diagnosis and treatment when such illnesses occur. Who should participate? Because the OHSP is a regulatory requirement, enrollment is mandatory for all persons who have contact with laboratory animals or wildlife, their tissues, body fluids or wastes or who are exposed to animal allergens on a regular basis. This includes not only the veterinary staff, animal care workers, investigators, laboratory technicians and students but may also include facilities and maintenance personnel and custodial staff. You will be successfully enrolled in the OHSP once you have completed 1) the on-line Animal Care and Use Exposure and Risk Assessment form and that it has been determined that a) no medical evaluation is necessary, or b) that a medical evaluation is necessary and that you have received the evaluation and any required interventions such as immunizations, and 2) all prescribed training. All information will be held confidential. This brochure alone does not provide all of the information you may need to completely assess the occupational risks associated with animal care and use. Instead, it briefly summarizes some of the hazards you may encounter and some important health and safety tips. Many activities require general safety training such as Laboratory Safety, Radiation Safety and Bloodborne Pathogens training. On-line training in these areas is found in the Faculty and Staff Training Center on Blackboard. Once there, you will need a user name and password to enter the site. After you are in, click on Faculty and Staff Training Center from the list of courses on the right side 8/15/14 2 of the screen. From there, click on the appropriate link on the left side of the screen. For assistance, contact Tech Support at (909) 469-5432 from an outside line or dial x-5432 from an inside line. RISKS ASSOCIATED WITH ANIMAL EXPOSURE Allergies, infectious disease and physical injuries are the primary health risks to persons working with or around laboratory animals. Allergic reactions are exaggerated reactions by the body’s immune system, most often to proteins, and are among the most common conditions that adversely affect the health of workers exposed to laboratory animals. Proteins most commonly associated with allergic reactions are found in the animal’s urine, dander and saliva, especially those from rodents. Nasal symptoms, itchy eyes and skin rashes are the most frequent manifestations of an allergic reaction but, in serious cases, asthma or anaphylaxis can occur. Symptoms that suggest the development of asthma include coughing, wheezing and shortness of breath. Severe and occasionally disabling breathing problems can occur. Rarely, an employee with allergic symptoms will develop a potentially life-threatening reaction following an animal bite or contaminated needle stick. If an allergic reaction to laboratory animals is to occur, it usually does so within one or two years of working with the animals although, on rare occasions, it may take years to develop an allergic reaction. In either case, once the worker has been sensitized, symptoms may occur within minutes of re-exposure to the animals. Disorder Allergic Reactions to Laboratory Animal Allergens__________________ Symptoms Signs _____ Contact urticaria Redness, itchiness of skin, welts, hives Raised, circumscribed erythematous lesions Allergic conjunctivitis and/or rhinitis Sneezing, itchiness, clear nasal drainage, nasal congestion Conjunctival vascular engorgement, clear discharge usually bilateral) Asthma Cough, wheezing, chest tightness shortness of breath Decreased breath sounds, wheezing, reversible airflow obstruction, airway hyperresponsiveness Anaphylaxis Generalized itching, hives, throat tightness, eye or lip swelling, difficulty swallowing, hoarseness, shortness of breath, dizziness, fainting, nausea, vomiting, abdominal cramps, diarrhea Flushing, urticaria, angioedema, stridor, wheezing, hypotension Allergies to latex gloves can occur with repeated exposure to products that contain natural rubber latex. The allergy is a reaction to certain proteins in latex rubber. The reaction may occur within minutes to hours after contact and produce a variety of symptoms. Mild symptoms include skin rash, hives or itching. More severe reactions include, runny nose, sneezing, scratchy throat, asthma and severe shock that can be life threatening. Persons with preexisting allergies or food allergies to avocados, bananas, potatoes, tomatoes, apples, carrots, celery, 8/15/14 3 melons or papaya are at increased risk of developing a latex allergy. If you are allergic to latex or suspect you may be developing a latex allergy, use nitrile gloves instead. Who is at increased risk of having an allergic reaction to laboratory animals? A history of allergy to other animals, particularly dogs and cats, is the best predictor for who will develop an allergy to laboratory animals. Activities such as handling animals and cleaning their cages increase the risk of exposure to animal proteins that cause allergic reactions and thus place the worker at greater risk of developing an allergy. Although workers with a personal history of asthma, seasonal allergies or dermatitis are at increased risk, persons with no prior history of allergies and only brief exposures can also become allergic to laboratory animals. How can you reduce the risk? Controlling exposure to allergens is the most effective strategy for reducing or preventing allergic reactions so Protect Yourself! Work in a clean, well-ventilated environment. Use a well-designed waste management system. Limit the number of exposures. Wear appropriate PPE such as a lab coat and disposable gloves Never rub your face or eyes until you have removed your gloves and washed your hands thoroughly. Wear appropriate respiratory protection. Zoonotic diseases are diseases that can be transmitted from animals or animal tissues to humans. Although many animal pathogens can cause disease in humans, zoonotic diseases are not common in modern animal facilities due to successful efforts at disease prevention and detection. Nevertheless, some animal diseases may produce serious disease in humans even when the animals themselves show few signs of illness. Therefore, you must be aware of possible consequences when working with each species of animal and take precautions to minimize the risk of infection. Personal hygiene is a critical barrier to the transmission of zoonoses. Should you become ill with a fever or other sign of infection, let your healthcare provider know that you work with animals. If you are concerned that you may have symptoms suggesting an allergy or illness, notify your supervisor immediately. Your supervisor may refer you to U.S. Health Works to determine the best plan of action. PREVENTION Some common sense steps that can be taken to lessen the risk of contracting a zoonotic disease include: Do not eat, drink or apply cosmetics, lip balm, or contact lenses around animals. 8/15/14 4 When performing bedding changes, blood or urine collections or necropsies, work in biological safety cabinets or use specialized PPE. Wear gloves when handling animals or their tissues. Do not recap used needles! Instead, discard them promptly in a biohazard “sharps” container. To reduce the risk of needle stick injuries, sedate or anesthetize animals if manual restraint is problematic Consult your supervisor or Environmental Health and Safety at x-5528 if you need additional training at any time. WHAT YOU SHOULD KNOW Physical hazards include animal bites and scratches, sharps injuries, injuries associated with compressed gas cylinders and moving cages or equipment. The key to preventing these injuries is proper training and meticulous attention to proper work practices. Use appropriate techniques for animal handling and restraint. Do not recap used needles or scalpel blades. Dispose of sharps in approved containers. Use proper lifting techniques with heavy loads or when doing repetitive tasks. Wear personal protective equipment (PPE) such as a lab coat, gloves and face mask. About bites, scratches and other injuries: Contact your supervisor immediately if you are bitten or scratched, if you injure yourself on animal caging or equipment or if you experience unusual disease symptoms. If you are pregnant: Working with hazardous agents in general and toxic chemicals in particular is discouraged during pregnancy. Consult your healthcare provider for advice about working safely during pregnancy. Toxoplasma is an infectious parasite that can be shed in cat feces. It can infect the fetus in women who are exposed during pregnancy and do not have immunity to the organism. To help assess the level of immunity against this organism, serum samples can be tested. Cat feces should be avoided and gloves should be worn when working in areas that are potentially contaminated. Wash your hands thoroughly after handling any potential source of infection. Nonhuman primates: Several primate viruses can cause disease in humans of which Herpesvirus simiae (B-virus) is of greatest concern. This virus occurs naturally in macaques such as rhesus and cynomolgus monkeys. Infected monkeys usually do not show clinical signs but the virus may cause fatal encephalitis in humans. Transmission to humans occurs by exposure to contaminated saliva, secretions or tissues. This typically occurs as a result of a bite or scratch. Transmission can also occur via splashes that come into contact with mucous membranes or from injuries caused by contaminated equipment. Proper work practices constitute the best protection against infection. 8/15/14 5 Wear PPE that includes protective outer garments, gloves, face mask and eye protection. Sedate monkeys whenever possible before handling. In the event of possible exposure, obtain medical attention immediately. Instructions for treating wounds and obtaining medical attention will be posted in each primate area. Mycobacterium tuberculosis (TB) may be transmitted from humans to animals AND from animals to humans. Nonhuman primates and persons in contact with them must be TB tested regularly. To prevent transmission, appropriate PPE should be worn when working with or around this organism. Shigella, Campylobacter, Salmonella, and Entamoeba histolytica cause diarrhea in primate species and can cause similar problems in humans exposed to primate feces. Infection is best prevented by the use of gloves and careful hand washing. Simian immunodeficiency virus (SIV) is closely related to HIV, the virus that can cause AIDS in humans, and, on rare occasions, can affect macaques. Some evidence suggests it may infect humans as well so measures should be taken to prevent contact with monkey blood or blood products. If you work with dogs or cats, the main risks are bites and scratches that can lead to infection. Cat scratch disease is caused by a rickettsial organism and is characterized by flu-like symptoms and swollen lymph nodes. Cat bites can result in severe bacterial infections. The likelihood of contracting rabies as a result of a bite is low because dogs and cats are usually vaccinated for rabies or bred exclusively for research. Nevertheless, it is recommended that persons in contact with dogs or cats be vaccinated against rabies. If you work with farm animals, Q fever, a potentially serious disease caused by Coxiella burnetii, is of concern. Q fever is carried by ruminants and is shed from the placental membranes of sheep. This route of exposure may cause Q fever pneumonia and other associated symptoms in laboratory workers. Sheep used in research should be assumed to be infected and measures should be taken to prevent transmission. All persons working with pregnant sheep should wear gloves, respiratory protection and protective outerwear that is fluid resistant. If you work with rodents or rabbits: Allergies are common among personnel who work with rodents (mice, rats, guinea pigs, hamsters) and rabbits. If you have pre-existing allergies or if you experience a runny nose, itchy eyes or skin rashes when working around these species you should report this immediately to your supervisor. Measures can be taken to limit your exposure to allergens thus reducing the severity of symptoms and decreasing the likelihood that symptoms will worsen. Rodents and rabbits obtained from commercial sources do not constitute a significant source of zoonotic diseases. However, animals caught in the wild can harbor a variety of bacterial, viral fungal and parasitic infections that constitute a significant hazard to personnel. 8/15/14 6 Sharps are common in animal care facilities and laboratories and include needles, broken glass and scalpels. Do not recap used needles. Instead, all used sharp devices must be discarded in a properly labeled biohazard sharps container. Locate sharps disposal containers as near to the point of use as possible as traveling across a room to dispose of a scalpel or needle increases the risk of injury and/or exposure. At no time is it permissible to dispose of any sharp device in a regular waste container. Incorrect disposal of sharps puts custodial staff at high risk of injury from cuts, puncture wounds, infectious agents or hazardous chemicals. Electrical hazards are found throughout animal and laboratory facilities. Electrical outlets should be covered and/or ground-fault protected. Be particularly cautious when using electrical equipment in wet areas such as cage-wash areas and rooms housing aquatic species. Do not use equipment with frayed or damaged cords or cords with splices or repairs made with electrical tape as such tape does not provide insulation. Use power strips that have power surge protectors instead of extension cords. Compressed gas cylinders may be found in animal facilities and laboratories. They are heavy and are under high pressure and thus contain an enormous amount of energy. Uncontrolled release of this energy from a typical compressed gas cylinder can easily propel the cylinder through a concrete block wall. To minimize this risk, all compressed gas cylinders, including empty cylinders, must be doubly secured by wall chains or brackets. Replace the protective valve stem cap when the cylinder is not in use. Wet floors in animal rooms and cage wash areas increase the risk of slips and falls. The risk of back injuries can be reduced by using proper lifting technique and not lifting excessively heavy or bulk loads. Some jobs may require two people, so get help when needed. Hand, finger and arm injuries can easily occur from moving large equipment and racks through narrow doorways and hallways. Placing hands on the front of the rack rather than the sides where they are unprotected can help avoid injuries to hands. Noise is generally not a problem in rodent facilities but dogs and pigs are known for their persistent and loud vocalizations that can become intense in the confined area of a holding facility. Cage washers, high-pressure air cleaning equipment and wet vacuum systems are other sources of excessive noise. In areas with excessive noise, hearing protection is recommended. If you work with hazardous agents: The proper use of hazardous biological (biohazardous), chemical and physical agents is dependent on careful planning, proper training and careful attention to prescribed safe work practices. Signs should be posted indicating the nature of the hazard, necessary precautions and emergency contact information. The PPE needed depends on the agent used but, in all cases, gloves should be worn and hands should be washed with soap and water after handling potentially contaminated materials. A biological safety cabinet should be used when handling infectious materials, especially if there is a potential for generation of 8/15/14 7 aerosols, and a fume hood should be used when handling toxic chemicals or radioactive materials. Biohazardous material is defined as infectious agents, toxins or other biological materials that present a risk or potential risk to the health of humans, animals or the environment. The risk can be direct through infection or indirect through damage to the environment. Biohazardous materials include certain types of recombinant DNA, organisms and viruses infectious to humans, animals or plants (e.g., parasites, viruses, bacteria, fungi, prions, rickettsia) and biologically active agents (e.g., toxins, allergens, venoms) that may cause disease in other living organisms or cause significant impact to the environment. All human blood products, tissue and many body fluids must be handled as if infected and, therefore, must be treated as biohazardous material. This includes human blood or bloodbased products, human clinical samples other than saliva, human cells and human cell lines, unfixed human tissues and water containing human waste. Persons who handle or are at risk of exposure to these potentially infectious materials must be vaccinated against Hepatitis B virus or sign the Hepatitis B Vaccination Declination Form. Laboratory personnel are at the greatest risk because of their potential for direct contact with concentrated stocks of infectious agents. Animal care personnel are at much lower risk but may still be exposed through direct contact with infected animals, from animal bites or scratches or through contact with contaminated bedding and cages. Animals exposed to biohazardous material must be housed in a containment room or facility clearly identified with the universal emblem for biohazardous material. Check with the Institutional Biosafety Committee before using biohazardous or potentially biohazardous material in animals. Fresh animal tissues, blood and body fluids should be treated as potential sources of zoonotic disease. If you need additional information, contact the Attending Veterinarian or the Biosafety Officer. Inhalational anesthetics are often used in animal experiments and may pose a health risk to persons working with or near them, particularly if pregnant. Depending on the agent, they may be carcinogenic or otherwise toxic to major organ systems, e.g., the liver or kidneys. Proper ventilation must be maintained by use of a scavenging device, a fume hood or other local exhaust ventilation. Ethylene oxide is a carcinogen that is used in some animal facilities to sterilize equipment that cannot be autoclaved. The safest way to use ethylene oxide is with a sealed bag system inside a properly functioning fume hood. Radiation can present a hazard through inhalation, ingestion, skin contact or proximity. Ionizing radiation is of particular concern because it can remove electrons from other atoms and, 8/15/14 8 in mammalian cells, this may directly damage DNA or it may lead to the formation of free radicals which are highly reactive with various cell components and can result in abnormal cell function or cell death. Non-ionizing ultraviolet (UV) radiation can occur with the use of UV germicidal lamps and transilluminators. UV light is very damaging to the skin and eyes and can cause hyperpigmentation, burns, cataracts, photokeratitis and skin cancer. Protect skin and eyes when using equipment that generates UV radiation. Cover hands with gloves and protect arms with long sleeves. An appropriate face shield will protect the eyes and face. There may be occasions when radioactive material must be administered directly to live animals (in vivo). If a radioisotope is administered in vivo, the animal itself is now radioactive, as is the cage in which it is housed and the bedding material lining the floor of the cage due to the presence of contaminated urine and feces. Animal care personnel are largely protected from exposure to such radioactive material by their required use of PPE within the vivarium. Nevertheless, the door to any room within a vivarium that is used either for the administration of radioisotopes to live animals or to store radioactive material of any kind must be posted with the sign on the left. Any study conducted within a vivarium that requires the in vivo use of radioactive material must be conducted using disposable cages to house the animals. At the end of each study, the cages and all bedding material must be double bagged and properly disposed of in waste containers designated and approved for disposal of radioactive waste. Contaminated animal carcasses must be kept in a properly labeled designated freezer for storage until picked up by a vendor licensed to dispose of such material or stored until the isotope has decayed to acceptable background levels. EATING OR DRINKING IN ANY LABORATORY, VIVARIUM OR OTHER AREA DESIGNATED FOR THE USE OF RADIOACTIVE MATERIAL IS STRICTLY PROHIBITED! No food or beverages may be kept or consumed in areas posted for radioactive material use or storage. In addition, all other activities involving handto-mouth motion such as application of cosmetics, lip balm, gum chewing, etc. must be avoided. Do not place notebooks, pens, tools, etc. in posted radioactive material areas as they can easily become contaminated. Additional radiation safety training may be obtained by contacting the Radiation Safety Officer at (909) 469-5592 from an outside line or at x-5592 from an inside line. WesternU adheres to the policy of ALARA, keeping radiation doses As Low As Reasonably Achievable. ----------------------------------------------------------------Persons who have sustained a work-related injury or illness should report to their immediate supervisor to initiate the proper paperwork and then immediately seek medical attention. Work- 8/15/14 9 related injuries are covered under worker’s compensation and must be reported on the Workers Compensation Claim Form. For California, it is DWC 1 and, for Oregon, it is Report of Job Injury or Illness, form 801. It is the responsibility of the person’s immediate supervisor to complete the appropriate paperwork and submit it to the workers’ compensation coordinator in Human Resources. For additional information about Worker’s Compensation, contact Human Resources at (909) 469-5372 from an outside line or at x-5372 from an inside line. To confirm that you have read and understand the information contained herein, you must pass the on-line quiz located in the faculty and staff training center on Blackboard. Once in Blackboard, you will need a user name and password to enter the site. After you are in, click on Faculty and Staff Training Center from the list of courses on the right hand side of the screen. After accessing the Training Center, click on IACUC on the left side of the screen. Then scroll down to the Occupational Health and Safety Program – Quiz and begin. Contact Tech Support at 469-5432 for assistance. 8/15/14