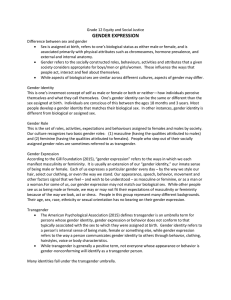
BREAKING THE BINARY: ADDRESSING HEALTHCARE DISPARITIES WITHIN SACRAMENTO’S TRANSGENDER COMMUNITY A Project
advertisement

BREAKING THE BINARY: ADDRESSING HEALTHCARE DISPARITIES WITHIN SACRAMENTO’S TRANSGENDER COMMUNITY A Project Presented to the faculty of the Division of Social Work California State University, Sacramento Submitted in partial satisfaction of the requirements for the degree of MASTER OF SOCIAL WORK by Annie Louise Temple SPRING 2013 BREAKING THE BINARY: ADDRESSING HEALTHCARE DISPARITIES WITHIN SACRAMENTO’S TRANSGENDER COMMUNITY A Project by Annie Louise Temple Approved by: __________________________________, Committee Chair Serge Lee, Ph.D., M.S.W. Date ii Student: Annie Louise Temple I certify that this student has met the requirements for format contained in the University format manual, and that this project is suitable for shelving in the Library and credit is to be awarded for the project. , Graduate Coordinator Dale Russell, Ed.D., L.C.S.W. Date Division of Social Work iii Abstract of BREAKING THE BINARY: ADDRESSING HEALTHCARE DISPARITIES WITHIN SACRAMENTO’S TRANSGENDER COMMUNITY by Annie Louise Temple Previous research has illuminated the fact that the transgender community faces many barriers to healthcare (Lombardi, 2001). The purpose of the present study was to determine the current barriers that the greater Sacramento area transgender community experiences surrounding the ability to access quality healthcare services. The researcher conducted interviews with transsexual individuals, health professionals, community advocates and Social Work professors. The present study, like previous research in other parts of the country, revealed that medical professionals are not adequately trained in transgender cultural competency and that more education and training needs to be given to both mental and physical health providers. The present study also found that Gender Identity Disorder, a mental disorder that transgender-identified individuals are often diagnosed with, assists transgender individuals in insurance coverage but also stigmatizes them. Implications for social work practice in addition to future research recommendations are also discussed. , Committee Chair Serge Lee, Ph.D., M.S.W. Date iv ACKNOWLEDGMENTS My parents have offered invaluable encouragement throughout the writing of this project. My parents, Nancy and Blake Temple gave me an abundance of emotional support, helped motivate me to “get to the coffee shop and write!” and answered many frantic phone calls. My mother, Nancy Temple helped me edit my project and was open to learning about a topic that she previously knew very little about. Thank you both for your unwavering support throughout my work on this project and through all of life’s ups and downs. My friends and colleagues in this program, Leah Barros, Christine Arneson, and Heather Valdez have also been amazing throughout this process. Even though they had projects of their own to work on, each of these women made themselves available to support me when I needed encouragement. Whether it was reassuring me that I “WILL FINISH” via text messages, commiserating over drinks and dinner, taking mini trips to Napa to get a break from the perils of writing or intimate conversations over coffee (specifically the ones that had NOTHING to do with this project), I CAN’T thank you ladies enough. Your friendship means the world to me. I also need to thank my cats, Fall, Stanley and Spring Temple. Spring, thank you for being so cuddly and cute and keeping me company during the naps that I took to procrastinate. Thank you also for demanding food with your piercingly loud meows in the morning so that I got out of bed and got to work. Fall, thank you for being the king of the neighborhood and keeping me company (on my lap) while I typed away on my v laptop. Stanley, thank you for being so youthful and cute, your energy (although sometimes irritating) reminded me to stay light hearted throughout the stressful times. Thank you also to Emily Newton for advising me on this project, inspiring me to thank my cats and for being an amazing and supportive friend. I also want to thank my advisor, Dr. Serge Lee for his advising and reassurance. Additionally, thank you to Dr. Andrew Bein and Dr. Chrys Barranti for their mentorship. Thank you to Dr. David Nylund, the professor who first educated me about the oppression that the transgender community experiences and inspired the focus of this project. Thank you for your support throughout the writing process and your dedicated commitment to the Gender Health Center (GHC). Lastly, I want to thank the Gender Health Center and Rachael and Ben Hudson for supporting my research and helping me recruit participants. The amazing work that is done on a daily basis at the GHC inspires me to be the best social worker that I can be. vi TABLE OF CONTENTS Page Acknowledgments................................................................................................................v Chapter 1. INTRODUCTION .........................................................................................................1 Background of the Research Problem......................................................................2 Study Purpose ..........................................................................................................3 Theoretical Framework ............................................................................................4 Definition of Terms..................................................................................................7 Social Work Research Justification .........................................................................9 Study Limitations ...................................................................................................10 2. REVIEW OF THE LITERATURE .............................................................................12 Transgender Identity ..............................................................................................13 Access to Healthcare ..............................................................................................22 3. METHODS ..................................................................................................................37 Study Objectives ....................................................................................................37 Study Design ..........................................................................................................37 Sampling Procedures .............................................................................................38 Instruments .............................................................................................................40 Data Analysis .........................................................................................................40 Protection of Human Subjects ...............................................................................40 vii 4. STUDY FINDINGS AND DISCUSSIONS ................................................................42 Overall Findings.....................................................................................................42 Specific Findings ...................................................................................................43 Interpretations of the Findings ...............................................................................52 Summary ................................................................................................................54 5. CONCLUSION, SUMMARY, AND RECOMMENDATIONS .................................55 Summary of Study .................................................................................................55 Discussion ..............................................................................................................55 Social Work Implications ......................................................................................60 Future Research .....................................................................................................61 Appendix A. Consent Forms..............................................................................................64 Appendix B. Questionnaires ..............................................................................................68 References ..........................................................................................................................72 viii 1 Chapter 1 INTRODUCTION Approximately 3%-10% of the population considers themselves transgender (van Kesteren, Gooren, & Megens, 1996). The transgender community has long been marginalized when it comes to receiving acceptable healthcare services. There are many reasons for the subpar healthcare access that transgender individuals are subject to. Fear of stigma, violence, judgment, prejudice and also a general lack of services specific to this population are several of the reasons behind the lack of access to quality care (Alegria, 2011; Lombardi, 2001). The fears that many transgender individuals live with surrounding seeking healthcare are not unfounded due to pervasive societal stigma. In one study, 60% of transgendered individuals interviewed reported being the victim of harassment and/or violence (Lombardi). In another study in Philadelphia, 26% of respondents from a 182-person sample of transgender individuals, reported to having been denied healthcare access due to their gender identity (Kenagy, 2005). In addition to pervasive stigma, many transgender individuals lack insurance coverage or do not have insurance that covers transition related services. Lack of coverage for necessary healthcare services, fear of culturally incompetent providers and lack of insurance access all influence the problem of finding and obtaining quality healthcare (Johnson, Mimiaga, & Bradford, 2008; Lombardi, 2001). Faced with many barriers to receiving adequate healthcare services, many transgender individuals go without healthcare (Sanchez, Nelson, Sanchez, & Danoff, 2009). It is unacceptable for any human being to go without 2 the fundamental right of healthcare and thus, more studies must be done to find out details about specific barriers that leave transgender individuals without satisfactory access to superior, culturally competent mental and physical healthcare services. The current Master’s Project hopes to identify information about the access transgender individuals currently have to quality mental and physical healthcare services in the greater Sacramento region. Additionally, the study aims at identifying what the barriers are for transgender individuals when seeking both psychological and physical health care services. Lastly, the current study will assess what possible solutions there are to the barriers discovered and what is already being done to alleviate the identified barriers to ensure adequate healthcare for the greater Sacramento region’s transgender community. Background of the Research Problem The research problem for the current study is to examine the quality of healthcare available to the greater Sacramento region’s transgender community. Currently, there are not enough culturally competent mental and physical healthcare services for the transgender community in the United States. Furthermore, transgender individuals that have access to health insurance and healthcare often come across culturally incompetent doctors and mental health professionals. Although there are guidelines available through the World Professional Organization of Transgender Health (WPATH), many doctors and psychotherapists are not educated on culturally appropriate ways to treat transgender patients. More research needs to be done to reveal the current barriers to obtaining 3 proper healthcare for transgender individuals, brainstorm solutions to these barriers and assess the cultural competence of health providers in order to get a full picture of what is going on for the transgender community in the greater Sacramento area when it comes to receiving quality mental and physical health care. Study Purpose The transgender community has been gaining more attention as a legitimate community who has been marginalized not only within society as a whole but also within the LGBTQ community. Because the transgender community has been pathologized and ignored by much of society, few studies have been done to assess the unique needs of the transgender community when it comes to receiving both physical and mental healthcare (Alegria, 2011). Since the transgender community has been invisible in many scholarly studies surrounding LGBTQ access to healthcare, it is important that social workers study how much access the community currently has to mental, physical and transition related healthcare. The purposes for this study are to discover the extent that healthcare services are available to the transgender community in the greater Sacramento area currently, what kinds of reformations to healthcare need to happen in order to adequately meet the transgender community’s needs, to discover the reasons behind why adequate healthcare services may not be available and identify potential solutions. In addition to these reasons, this study will also seek to find out what local professionals and transgender individuals think about the Gender Identity Disorder/proposed Gender Dysphoria diagnosis and how helpful these are in accessing healthcare. Because the transgender 4 community has only recently begun to be recognized as a population that deserves a voice, it is imperative that these questions be researched so that more information can be gathered to ensure that transgender individuals in the greater Sacramento area and all over the world have access to sufficient healthcare. The author of this Master’s Project expects to find that healthcare services for the transgender community in the Sacramento area are going to be limited and grossly inadequate when it comes to cultural competency. It is also expected that most of the transsexual participants that are interviewed will carry a Gender Identity Disorder (GID) diagnosis. Because transgender individuals are still pathologized as having a mental disorder, the assumption is that without this diagnosis, required surgeries and other medical treatments may be seen as cosmetic and thus, not covered by insurance. This researcher expects to find that most professionals and transgender participants alike find the GID diagnosis to be helpful in obtaining healthcare services yet stigmatizing by nature of it being a mental disorder. Finally this researcher expects to find that mental health professionals, medical doctors and nurses are going to possess little knowledge about the unique needs of the transgender community. It is expected that many healthcare settings will neither have programs nor plans in place to serve the transgender community and meet the unique needs of this population. Theoretical Framework Three main social work theoretical frameworks will be utilized when conducting this study. The first theoretical framework utilized in this research is the Conflict 5 Perspective (Johnson & Rhodes, 2010). This theory describes how minority populations are marginalized due to their lower economic and cultural status. The conflict perspective explains the reasons behind why transgender individuals have not been able to receive adequate healthcare. According to the Conflict Perspective, the healthcare system in our society holds the power and because transgender individuals are not a highly valued and powerful community, they are not valued in our healthcare system (Johnson & Rhodes, 2010). Through this perspective, research into the discrepancies in access to and quality of healthcare is extremely important because it is only in actively fighting the system and demanding rights, that the transgender community is going to obtain access to quality healthcare services. This study will utilize Conflict theory in the hope that the present study’s research findings can be a part of the fight for social justice for the world’s transgender community. The second theoretical framework used to inform the present study is Queer Theory (Butler, 1988). Queer Theory suggests the ridding of sexual based binaries, whether they are related to sexual orientation, sexual practices or gender identity. Because the transgender community does not fit into the gender binary categories of “male” or “female” that are seen as essential and fixed identities in much of our society, transgender individuals are marginalized and pathologized as having a mental disorder (Sennott, 2011). Following this logic, because the transgender identity is outside of the socially constructed binary and therefore marginalized by it, the pathologization of the identity that this creates influences the fact that the transgender community has 6 inadequate healthcare access. Thus, if society were to rid itself of gender binaries and adopt a more fluid idea of gender and sexuality, the transgender population would no longer be marginalized and would have more opportunities for equality in society and better healthcare access and services. The present study will utilize Queer Theory in that it will study a population that does not fit into the current gender binary. In recognizing the transgender community as one that deserves equal access to healthcare, Queer Theory allows research into categories outside of commonly accepted societal gender binaries and hopefully will enable society to move towards a system that is more inclusive of different gender identities and sexual orientations (Butler, 1988). The third theoretical framework that guides this research project is Transgender theory. In many ways, Transgender theory is a bridge between essentialist theories of sexuality, Feminist theory and Queer theory. Transgender theory views essentialist theories of sexuality as being too rigid, as they suggest that a person’s gender and sexual orientation are fixed traits within an individual. Similarly, Transgender theory views social constructivist theories such as Queer theory and Feminist theory as discounting a transgender person’s unique experience and claim of an identity that can assist in combatting stigma and marginalization. In finding a balance between essentialist theories, Feminist theory and Queer theory, transgender theory incorporates socially constructed ideas of gender with transgender individuals’ unique experiences, so as not to discount identities that can be helpful to a person or the entire transgender community (Nagoshi & Brzuzy, 2010). The present study will bring awareness to the socially 7 constructed nature of gender and at the same time honor the Transgender identity and the ways that the gender binary can be helpful to transgender individuals. Definition of Terms The following are definitions of terms used in this research project. Without an understanding of these terms, the review of the literature and present study’s findings cannot be properly understood. Cisgender An individual who is cisgender identifies as the same gender as his/her biological sex (Hulstein, 2012). Gender Binary The Gender Binary reflects common perspectives in contemporary society surrounding gender norms. People are often referred to as being female or male. These categorizations stem from a person’s biological sex and other performative actions such as whether one chooses to wear skirts or pants. Certain behaviors are socially constructed as being normal and others are pathologized. The Gender Binary refers to the rigidity surrounding gender categorization in that it only has two options: male or female. Transgender individuals often fall outside of this binary (Butler, 1998). Genderqueer Transgender individuals and cisgender (individuals whose gender reflects their biological sex) individuals alike sometimes identify as genderqueer. This 8 category of gender identity can encompass any and all expressions of gender that do not fit neatly into the gender binary (e.g., a man who prefers to wear women’s clothes or a female born individual who prefers to express a masculine identity) (Alegria, 2011). Intersex Intersex individuals are born with genitalia and/or chromosomal make up that can neither be classified as male or female. There is a range of different possibilities of intersex characteristics. For example, intersex individuals may have male genitalia and XY chromosomes or ambiguous genitalia (Sax, 2002). LGBTQ LGBTQ is an acronym that stands for Lesbian, Gay, Bisexual, Transgender, Queer. This acronym is often used when talking about entire Queer community (Sherrif, Hamilston, Wigmore, & Giambrone, 2011). Gender Gender is a socially constructed category that in contemporary society is often looked at as a binary system with only two options: male or female. Because the term “gender” differs from sex in that it is not referring to biological features, in reality, there are many more than two expressions of gender (Butler, 1998; Nagoshi & Brzuzy, 2010). 9 Transgender The term transgender is an umbrella term that has a range of expressed gender identities. Transgender identities can include individuals who identify as the opposite gender from their birth sex, transvestites, cross-dressers and individuals that express other gender-bending practices (Reis, 2004). While some transgender individuals readily embrace the gender binary, others may reject it entirely (Alegria, 2011). Transsexual The term transsexual refers to a transgender person who feels that they are a different gender from their biological sex. Most transsexual persons are in the process of transitioning to a gender other than their birth sex (Roen, 2001). Transphobia Transphobia refers to discomfort and negative feelings towards those who do not comply with societal gender norms and live out differing expressions of gender (Lombardi, 2009). Social Work Research Justification The transgender population has historically been a marginalized and oppressed community. As stated in the National Association of Social Workers’ (NASW) Code of Ethics, it is important for social workers to take action against discrimination towards any group of people. Because the transgender population is the victim of discrimination in many realms, it is important that social workers take action (NASW, 2008). In order for 10 social workers to begin action steps at alleviating stigma, fighting discrimination and advocating for better healthcare services for transgender individuals, more research needs to be done to find out the specific factors contributing to the transgender population’s marginalized status. This research examines healthcare disparities among the transgender community and therefore sheds light on an important topic for social workers to act on. Social workers are pursuers of social change and advocates of social justice and this research project reflects both goals. In examining barriers to healthcare for the transgender community, social workers can begin to advocate with the transgender community for more comprehensive healthcare services. Without research into the healthcare services available, accessibility of care, specific barriers and possible solutions, social workers do not have enough knowledge to fight for social justice for the transgender community. It is the hope of this researcher that this study will be part of a broader effort to bring the transgender community out of invisibility and help highlight this population’s healthcare needs. Study Limitations This research project is limited in nature by its small sample size. Because the researcher cannot afford to provide incentives for participating in the research, all subjects participated on a volunteer basis. Because the sample size is so small, it is difficult to generalize findings to the greater Sacramento region’s entire transgender population or the United States population at large. Additionally, the researcher composed her own questionnaires and therefore the interviews were unstandardized and 11 may lack validity. An additional limitation is that two of the medical professionals are connected to the Gender Health Center, a non-profit counseling center specializing in the transgender community’s needs. Had the researcher interviewed medical professionals unassociated with the Gender Health Center, different results may have been found. With that said, the research conducted in this study contains results from interviews done with experts in the field of transgender healthcare and transsexual participants personal experiences. Because of this, these results are extremely valuable when looking at the struggles that this population faces in obtaining respectable healthcare services. 12 Chapter 2 REVIEW OF THE LITERATURE The transgender community is broad in definition and has only recently begun to get the recognition it deserves as a population with specific needs. Additionally, only recently have efforts begun to research the available healthcare services for the community (Alegria, 2011). For the last several years, many transgender individuals have been given a psychiatric diagnosis of Gender Identity Disorder (GID) that has been both helpful and damaging to transgender individuals as it pertains to their access to healthcare services. The diagnosis can be helpful to transgender individuals getting certain healthcare services paid for by insurance, but harmful in other scenarios regarding prejudice and stigma from health care professionals (Sennott, 2011). The current Diagnostical Statistical Manual on Mental Disorders (DSM-IV) continues to classify the transgender identity as Gender Identity Disorder although the following edition will change the diagnosis to Gender Dysphoria (Ford, 2012). Previous research suggests that health care professionals need further training in transgender physical and mental health care as well as in the appropriate language to use with transgender individuals to ensure that professionals respect a transgender person’s preferred gender identity (Lombardi, 2001). Additionally, education and training for healthcare professionals needs to address the fear of stigma that currently exists within the transgender community in order to prevent transgender individuals from avoiding seeking healthcare due to their fears of 13 judgment, violence, and prejudice (Alegria, 2011). The following literature review explores the research that has been previously conducted pertaining to the transgender community’s access and barriers to healthcare. It begins by describing the transgender identity, and then explores the Gender Identity Disorder (GID) diagnosis and its pertinence to the transgender community when accessing healthcare. The literature review goes on to discuss the previously identified barriers to both physical and mental healthcare for transgender individuals and the role that The World Professional Association for Transgender Health (WPATH) plays in this process. Transgender Identity Gender Gender is considered a socially constructed category that in modern western society is often split into the binary male or female. Because the term gender differs from sex in that it is not referring to biological features, in reality, there are many more than two expressions of gender than the binary system suggests. Queer theorists such as Judith Butler (1988), view this binary classification of gender as harmful and question the need for such categorizations as well as the reasons for the categories. Queer theorists see gender as performative and dramatic and thus, see individuals as acting out a gender that is historically situated and culturally determined. Queer and Feminist theorists see these categories of male and female as being harmful to individuals that deviate from said categories. According to Queer theorists, the gender binary is used to contain and police individuals who do not fit into one of these categories, and thus, Queer theorists reject 14 these socially constructed systems (Butler, 1988). Opposed to viewing gender as an essential trait within an individual, Queer theorists see gender as being both socially constructed and fluid. Although Feminist theory argues that gender is one attribute that helps humans develop categories to identify and make meaning of relationships with other people, the gender binary can be extremely harmful to transgender individuals. When gender is viewed as a fixed essential trait within a person, it can be used as a justification for prejudice, discrimination, and other forms of oppression similar to other traits such as race and class when they were viewed as being natural. Because society expects a culturally specific gender expression that reflects one’s biological sex, the transgender expression of gender identity is outside of what is considered normal and is often deemed deviant or abnormal (Grossman & D'Augelli, 2006). However, viewing gender as entirely socially constructed with no merit whatsoever can also be problematic for transgender individuals. Without being able to at least partially identify with constructed ideas of gender, a transgender individual may feel like s/he is without an identity. If transgender individuals denied all labels of gender expression, the transgender community could not come together as an oppressed group to fight marginalization because following this logic, not even the transgender identity could exist. Because oppression and discrimination towards the transgender population is pervasive, socially constructed ideas of gender prove somewhat useful to transgender individuals in claiming an identity (Nagoshi & Brzuzy, 2010). 15 Although some physicians believe that a person whose gender identity differs from their biological sex is mentally ill and needs to be treated with behavioral therapies and medication, there is a great deal of research suggesting that gender identity is a relatively fixed trait. Several studies have been conducted with findings about intersex patients who are raised as a certain gender and turn out to identify as the opposite gender. Moreover, chromosomal make up does not predict gender identity. For example, an intersex person with an XY genotype may not identify as male, even if they are raised as a boy (Feldman & Safer, 2009). Transgender Approximately 3%-10% of the United States population is considered transgender (Grossman, & D'Augelli, 2006). As stated by Alegria (2011), the term “transgender” “refers to appearance, behavior, or identity that does not conform to socially constructed norms for women or men” (p. 176). Transgender as a construct is an umbrella term that has a range of expressed identities that do not fit within traditional male or female categories. Although the cause of transgenderism is unknown, one explanation comes from brain autopsies of transgender individuals. In one study with male-to-female (MTF) transsexuals, the Bed Nucleus of the Stria Terminalis (BST) in the hypothalamus contained less staining, a finding that is consistent with genetically female individuals. Additionally, sexual orientation had no effect on the amount of BST staining shown. This particular study illustrates an association between the transgender identity and BST staining in the brain. Although studies like these are small and there isn’t enough 16 research to draw any conclusions, preliminary results portray the fixed nature of gender identity and the transgender diagnosis. Despite some medical and mental health professionals’ claims, there is no literature to support the idea that gender identity can be changed or manipulated by behavioral therapies or other treatments (Feldman & Safer, 2009). The Transgender identity has a large range of expressions. Transgender individuals may identify as the opposite gender or as “genderqueer”, connoting that the gender expression is outside the norms of any categorized gender. Transgender individuals may dress in what is considered the opposite gender’s clothing; however, dressing in the opposite gender’s clothing does not necessarily make a person transgender. Moreover, not all transgender individuals desire to change their physical body with hormones or surgeries in order to live as their desired gender (Alegria, 2011). Many transgender individuals view themselves as expressing a fluid portrayal of gender identity, identify with masculine and feminine aspects of gender and therefore do not fit in the traditional categorical male/female binary. Recently, more transgender individuals have embraced a transgender identity instead of trying to fit within the dichotomy of masculine or feminine or male or female (Bockting, 2009). Transgender individuals may also be transsexual, defined as a condition that is biological in nature, therefore requiring surgeries and/or hormones to address the assumingly inherent condition. Typically, individuals that are transsexual have received medical interventions such as hormones and/or Sex Reassignment Surgery (SRS) (Nagoshi & Brzuzy, 2010). Moreover, some 17 transsexual or other gender nonconforming individuals don’t identify with the transgender identity at all and alternatively, even embrace the gender binary. Gender nonconforming individuals who do not claim a transgender identity will often solely identify with the opposite gender from their biological sex (Hines, 2007). In addition to the wide range of different experiences and gender expressions of transgender individuals, a person’s gender identity, including the transgender identity, does not indicate their sexual orientation. A person’s sexual orientation is entirely different than his/her gender identity (Alegria, 2011). A male-to-female (MTF) transgender individual may identify as a lesbian, bisexual, straight or queer woman, just as a female-to-male (FTM) transgender individual may identify as a gay, straight, bisexual or queer man. Gender identity does not dictate what gender or physical characteristics one is sexually attracted to (Alegria). The transgender community is a marginalized one, much like other racial, ethnic and Lesbian, Gay, Bisexual, and Queer (LGBQ) identities. However, in some ways, the transgender population is a different type of minority group. Unlike women or African Americans who may grow up in a community of people that look like them, it is very unlikely that a transgender individual will grow up in a society where they know of other transgender identified individuals. Therefore, their lack of social status is in part due to their isolation from each other (Johnson & Rhodes, 2010). Additionally, many other minority groups do not have a mental disorder attached to their identity. Currently, many 18 transgender individuals are diagnosed as having a mental disorder categorized in the DSM-IV as Gender Identity Disorder (GID) (Sennott, 2011). Gender Identity Disorder Many transgender individuals are diagnosed with what is known in the Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association [APA], 2000) as Gender Identity Disorder (GID). The American Psychological Association (APA) first presented GID as a diagnosis in 1980 and it continues to exist as a diagnosable mental disorder today (Byne et al., 2010). According to the DSM-IV, to be diagnosed with GID as an adolescent or an adult, a person must exhibit these characteristics: Frequent passing as the other sex, desire to live or be treated as the other sex, or the conviction that he or she has the typical feelings and reactions of the other sex, Persistent discomfort with his or her sex or sense of inappropriateness in the gender role of that sex, preoccupation with getting rid of primary and secondary sex characteristics (e.g., request for hormones, surgery, or other procedures to physically alter sexual characteristics to simulate the other sex) or belief that he or she was born the wrong sex. (Alegria, 2011, p. 178) In addition to these qualities, an individual with GID cannot have a “physical intersex condition” and the “disturbance causes clinically significant distress or impairment in social, occupational, or other important areas of functioning” (APA, 2000, p. 581). 19 Although the DSM-IV categorizes GID as a mental disorder, there are no standardized mental health treatment guidelines for treating GID. Currently, most of the guidelines for mental health professionals who are treating transgender individuals come from patients who report on the care that they are getting. However, there is a small body of research regarding mental health treatment for transgender individuals. Evidence suggests that patients with other psychiatric and or alcohol/drug abuse issues are more likely to be unsatisfied with their treatment. Additionally, retrospective data describes that adults with GID who undergo sexreassignment surgery (SRS) are more likely to experience satisfaction and well-being. Even though these outcomes are empirically validated, the APA has not instituted ethical guidelines for treatment of GID (Byne et al., 2010). Holding a diagnosis of Gender Identity Disorder (GID) can be both useful and harmful to transgender individuals. The fact that Gender Identity Disorder labels transgender individuals as having a mental disorder is pathologizing of the identity. Critics of the mental disorder diagnosis compare the diagnosis of GID to homosexuality that was also considered a mental disorder in the DSM-II as late as 1970 (Sennott, 2011). In addition to this criticism of the diagnosis, because gender nonconforming individuals have been seen throughout different time periods and various cultures, many people question whether it is appropriate to categorize transgender individuals as being deviant at all (Sennott). Gender Identity Disorder is considered a mental disorder with criteria that includes distress experienced by an individual when living in accordance to his/her 20 biological sex. However, many people feel that this distress is due to social stigma, not an inherent distress that is located within an individual who is gender nonconforming. A work group for the World Professional Association for Transgender Health (WPATH, 2011) has recognized that distress among those with GID is alleviated upon living in accordance to what a transgender person feels is his/her real gender identity. Therefore, the distress component of the diagnosis is wavering and largely impacted by societal discrimination and stigma (Bouman, Bauer, Richards, & Coleman, 2010). Along similar lines, critics of the diagnosis indicate that when something becomes a disorder in our society, it immediately becomes stigmatized. Many transgender theorists see the Gender Identity Disorder diagnosis as being a direct link to prejudice and discrimination against the community (Nagoshi & Brzuzy, 2010). Due to many of these concerns, the World Professional Association for Transgender Health (WPATH) has proposed a change for the DSM-V that would change the Gender Identity Disorder diagnosis to a Gender Dysphoria diagnosis. WPATH believes that because not all transgender individuals experience distress associated with their identity, the DSM-V’s Gender Dysphoria diagnosis would only address individuals that experience significant distress instead of blanketing the entire community under this diagnosis (WPATH, 2010). Opponents of the GID diagnosis, including WPATH, speculate that the transphobia that permeates modern American society stems largely from Gender Identity Disorder’s mentally disordered status (Sennott). 21 However, there are some benefits to having Gender Identity Disorder as a diagnosis in the Diagnostic and Statistical Manual on Mental Disorders (DSM-IV) (APA, 2000). Supporters of the diagnosis see the fact that GID is a mental disorder as a justification for insurance companies to cover health care services related to the physical transition process between genders (Sennott, 2011). Backers of the diagnosis question whether insurance companies would cover the costs for the medical aspects of the gender transition process if GID were not labeled as a mental disorder. Many healthcare providers offering sex reassignment surgery (SRS) require a GID diagnosis before surgery can be completed (Nagoshi & Brzuzy, 2010). Those in opposition of the GID diagnosis suggest one possibility that might keep the financial benefits and eliminate stigma for transgender individuals. As an alternative to a mental disorder, one suggestion is to transfer the GID diagnosis from a mental disorder into a medical or physical disorder, therefore eliminating some of the shame and stigma that currently accompanies having a mental illness (Sennott). In some ways, this would make sense due to the fact that many transgender individuals require medical treatment, hormones and/or surgery in order to transition. However, others acknowledge that although there are similarities between Gender Identity Disorder and homosexuality in that both were considered mental disorders at one point, homosexuality requires no medical attention. Some see this distinction as merit for GID continuing to exist in the DSM-V (Rochman, 2007). Others have suggested that a less stigmatizing DSM diagnosis would suffice. Ideas for a new diagnosis that is not as pathologizing include 22 the terms “Gender Dysphoria,” “Gender Dissonance,” and “Gender Incongruence.” Advocates of this type of change have insisted that a new name for the diagnosis would eliminate the shame that currently exists, while still allowing for the legal and medical procedures that the diagnosis affirms (Rochman, 2007, pp. 32-35). In May of 2013, the fifth edition of the Diagnostical Statistical Manual on Mental Disorders (DSM-V) will be released. In this new edition, Gender Identity Disorder will be removed as a diagnosis and replaced with Gender Dysphoria. The anticipated change aims at emphasizing the dysphoric feelings that transgender individuals often carry due to the incongruence between their biological sex and their preferred gender. Many involved in the transgender community feel that this new diagnosis will allow access to transition related healthcare without the stigma that has previously been attached to the Gender Identity Disorder diagnosis (Ford, 2012). Access to Healthcare WPATH For many transgender individuals seeking medical treatment to aid in their transition process, The World Professional Association for Transgender Health (WPATH) is the organization that guides this process (Alegria, 2011). WPATH is designed to promote “the highest standards of care” for transgender individuals and provide medical professionals with guidance on how best to help transgender individuals in their journey (WPATH, 2011, p. 1). WPATH provides many kinds of information to different types of clinicians including information related to a transgender person’s 23 medical transition in addition to medical issues that are not directly related to transitioning protocols. Guidelines are released for medical professionals who are treating the entire Lesbian, Gay, Bisexual, Transgender, Queer (LGBTQ) population that include creating a welcoming environment, utilizing appropriate language and pronouns, maintaining written confidentiality, and instituting mandated training and educational programs for staff. Unfortunately, even though these guidelines are available to the public, several studies show that in many cases, these guidelines are not being followed (Johnson et al., 2008). Although WPATH was designed for medical professionals, many transgender individuals and their family members will consult WPATH’s guidelines when making decisions regarding their own health needs (WPATH). WPATH provides specific standards for transgender-identified individuals to abide by when seeking to medically transition to the opposite gender. These standards also inform medical professionals about how to begin assisting their patients in their process towards transitioning. WPATH proposes a transition that happens in stages so that individuals have a chance to change their mind. Therefore, surgeries and more permanent parts of the transition process are recommended to come in the later stages (Byne et al., 2012). Although many transgender individuals never pursue surgery, if the transgender individual does decide to seek surgery, WPATH recommends that there be a collaborative team approach where the surgeon, primary care physician and mental health professional work together in order to best prepare the patient for surgery. Because of this collaborative approach, 24 surgeons who diagnosis/Gender Dysphoria Diagnosis as well as other medical problems the patient may be facing. Additionally, WPATH recommends that surgeons who are operating on transgender individuals should agree with the Gender Identity Disorder/ Gender Dysphoria diagnosis for their patient before proceeding with surgery, even if another medical professional has already made a diagnosis, due to the fact that surgeons are responsible for all diagnoses justifying the surgical procedures they perform. Because surgical intervention requires many medical professionals to be on the same page with treatment goals, in some geographic areas, there are treatment teams of different medical professionals already set up for transgender individuals seeking surgery. Unfortunately, treatment teams offering this approach are not available to many transgender individuals who seek surgery and in these cases; WPATH recommends that a surgeon communicate directly with all psychiatrists, psychologists and primary care doctors involved (Schechter, 2009). Although WPATH can be extremely helpful to medical professionals and transgender individuals, some critique WPATH in that it gives a medical professional, who may not be educated on transgender issues, too much power in deciding a transgender person’s fate (Lev, 2009). Many transgender individuals feel like they should be the ones to decide whether they are ready for sex-reassignment surgery instead of a medical professional that may not even be an expert in the area of transgender health care. Additionally, WPATH puts a lot of the responsibility on medical doctors and mental health professionals in determining a transgender person’s track. Through 25 charging mental health and medical professionals with diagnosing GID and often times determining if surgical treatment is appropriate, there is an expectation that these professionals are competent in transgender related care. This responsibility of medical professionals causes many transgender individuals to feel even more pathologized due to the fact that they often need a mental health diagnosis in order to obtain surgery (Bockting, Robinson, Benner, & Scheltema, 2004). Barriers to Healthcare Several empirical studies suggest that enormous disparities exist when it comes to the transgender community’s access to health care. In the United States, simply falling outside the norm in one’s sexual orientation or gender identity puts one at greater risk for developing health problems and for not receiving adequate healthcare (Brockett, McNair, & Suniewick, 2007). For transgender individuals who fall outside of the male-female binary paradigm, barriers to healthcare include inadequate care and a lack of services for both mental and physical health care needs. In one survey of transgender-identified individuals, only 30%-40% reported regularly seeking healthcare services (Sanchez et al., 2009). In a similar study (n=154) done with transgender subjects living in Philadelphia, 26% of the sample reported that they had been denied health care access in at least one instance due to their transgender identity (Kenagy, 2005). Additionally, research looking into access to health care in the United States among the Lesbian, Gay, Bisexual and Transgender, Intersex (LGBTI) communities found that the transgender community was 26 the most uninsured group. Within the transgender community, transgender people of color were the least likely to have insurance (Johnson et al., 2008). Absence of insurance coverage presents transgender individuals with even more problems. Lack of access to hormone therapy has created a black market industry for transgender individuals desiring secondary sex characteristics associated with the opposite sex. Many transgender youth and adults are getting their hormones outside of a medical setting, often times on the street, from friends or the internet. Because of this, the transgender community is at further risk for contracting HIV and other diseases from contaminated needles (Grossman & D'Augelli, 2006; Sanchez et al., 2009). HIV and AIDS are major concerns for the transgender community. In one study of 515 transgender individuals living in San Francisco, 25% were HIV positive. Despite this alarming statistic, literature suggests that transgender individuals are sometimes denied healthcare services related to the treatment of HIV and AIDS (Kenagy, 2005). Without health care access and competent health care services, this epidemic can only get worse. In addition to lack of insurance coverage, there are many other barriers evident that prevent the transgender community from obtaining adequate healthcare services. One of the most common barriers to transgender individuals receiving decent medical care is the ignorance of medical professionals. Many doctors are unfamiliar with transgender medical needs and are prejudiced towards the community (Lombardi, 2001). Due to this prejudice, many transgender individuals fear seeking treatment due to the pervasive stigma that exists in doctors’ offices in addition to previous negative 27 experiences with healthcare professionals (Shipherd, Green, Abramovitz, 2010). The stigma that the transgender population faces can manifest in physical violence or verbal attacks and the fear of these real threats prevents many transgender individuals from seeking healthcare due to fear of emotional violation from providers (Alegria, 2011). Furthermore, Alegria (2011) explains, “these forms of negative bias have been linked to greater rates of unemployment and risk of suicide among transgender persons” (p. 177). One cross-sectional study of 97 Male to Female (MTF) transgender adults found statistically significant results that a greater proportion of transgender adults had experienced a traumatic life event than had the rest of the biologically male population. This study found that transgender females had experienced about the same amount of trauma as women that were female-born. Additionally, 55% of transgender women reported being objects of unwanted sexual advances, 54% of transgender women reported sexual assault, 51% had experienced physical abuse and 33% claimed to have been harassed due to their gender identity. Moreover, transgender individuals who dressed as their preferred gender experienced much more exposure to traumatic events than those who did not (Shipherd, Magnun, Skidmore, & Abromovitz, 2011). For transgender individuals, the medical realm is not necessarily somewhere to escape this kind of abuse. In a video made for the California HIV/AIDS hotline about transgender health care needs, one transwoman describes the humiliation she experienced at an appointment with her primary care doctor. Having gone in for a bronchial infection, this transwoman described how she ended up on a table with many doctors curiously 28 examining her vagina, even though this had nothing to do with her reason for seeking care. Due to this experience, this patient now feels uncomfortable going to doctors that do not specialize in transgender health care (Transforming health care). Because transgender individuals experience a high rate of discrimination, stigma and violence in their lives, the fear of facing more of this treatment from medical professionals often prevents transgender individuals from seeking healthcare (Shipherd et al., 2010). The impact of stigma and violence on the transgender community is pervasive and many healthcare services are not culturally competent enough to make transgender individuals feel comfortable and safe. Added to the transgender community’s valid fears surrounding stigma and negative bias among medical professionals, another barrier identified that impedes the transgender community from seeking medical treatment is fear that medical professionals will tell a transgender individual’s family about his/her transgender identity. Because many transgender individuals are not public with their identity, the threat of being outed by a medical professional often prevents people from seeking treatment (Alegria, 2011). Lack of insurance coverage coupled with inadequately trained medical professionals creates enormous roadblocks for transgender individuals in need of healthcare services. On a Macro level, the mental and physical healthcare needs of the transgender community remains largely unknown to policy makers. Unlike other marginalized communities, the transgender community does not have specific access to publicly funded mental health care programs. Because of this lack of care, transgender 29 individuals often frequent community-based organizations and self-help or other support groups. In one study, where interviews were conducted with 30 transgender individuals, such support groups proved to be incredibly helpful at filling in the gap of what is greatly lacking in medical care (Hines, 2007). Healthcare Needs The transgender community would greatly benefit from medical professionals becoming trained and further educated on transgender medical care, in addition to training about appropriate language to use with transgender identified individuals (Alegria, 2011). When meeting with a transgender identified individual, professionals need to address the person in a “gender appropriate manner,” referring to the person by the pronoun with which he/she self identifies. However, many doctors are not aware of or do not follow this practice (Alegria, 2011, p. 179). Additionally, many of the intake forms contain only two gender options: male and female. This fact further marginalizes the transgender community in that there isn’t even a space for the transgender community to choose their preferred gender when coming to see a medical professional. Similarly, Dafna Wu, a nurse at a clinic specializing in causes many transgender individuals discomfort. Wu asserts that having unisex bathrooms is imperative to equalization of healthcare services for the transgender community (Brockett et al., 2007). Prior research has shown that nurses need more comprehensive training regarding Lesbian, Gay, Bisexual, Transgender, Queer (LGBTQ) cultural competence. Specific to the transgender population, it is essential that nurses receive more training about allowing 30 transgender persons to self-identify when it comes to picking a gender on an intake form (Cavender, 2011). In one study, only 10% of nurses had adequate knowledge about the LGBTQ community (Lombardi, 2001). In another similar study, when given a questionnaire regarding LGBTQ issues, only 13% of the nursing students interviewed got 90% of the questions correct (Chapman, Watkins, Zappia, Nicol, & Shields, 2011). Transgender individuals are aware of the fact that medical professionals do not understand their needs. In a study where researchers interviewed 30 transgender individuals about their access to healthcare, participants identified lack of understanding among general practitioners of medicine as one of the top reasons for the existing disparities (Hines, 2007). The results from these studies illustrate that the medical community in general lacks knowledge pertaining to the transgender population’s healthcare needs. Additionally, physical examinations for transgender individuals should be tailored to individual needs and based on the person’s physical anatomy, hormone regimen, possible medications, and potential surgeries instead of doctors and nurses solely relying on a person’s sex assigned at birth or their current gender presentation. Physical and laboratory examination of the MTF who has had sex reassignment surgery should include pelvic examination with Papanicolau (Pap) smear, prostate exam, prostate specific antigen (PSA), and mammograms. Examination of the FTM with a vagina should include pelvic examination with Pap smear, clinical breast exam, and if breast tissue is present, mammogram. (Alegria, 2011, p. 180) 31 Currently, transgender individuals are often denied healthcare examinations based on their birth sex after they have transitioned despite continuing to need these procedures. In one study of 122 female-to-male (FTM) men, nearly 50% of them did not receive annual pelvic examinations and only 7% had a diagnosis of polycystic ovarian syndrome, 18% less than what the general population reports (Johnson et al., 2008). Without proper exams, many of the individuals in this study may have had PCOS and were simply not aware of it. Lori Kohler, a family practitioner specializing in transgender healthcare described the fact that many doctors are uneducated about transgender individuals who take hormones. Many doctors, Kohler describes, wrongly assume that the health problems that transgender individuals are experiencing are related to the hormones that the person is taking (Brockton et al., 2007). Unfortunately, doctors are not the only ones who are largely uneducated about transgender health care needs. Because transgender individuals have healthcare needs that differ from some healthcare needs of biological males and females, many insurance companies will not cover certain sex-specific exams that transgender individuals may need. Medical professionals and insurance companies alike are not well versed in medical services that are unique to this community and the lack of education greatly impacts the quality of care for the transgender community (Alegria). Additionally, many transgender adults first seek mental health treatment for a secondary condition such as substance abuse, depression or another mental health problem that is really related to their gender dysphoria (Byne et al., 2010). The pervasive 32 social stigma towards the transgender community causes a myriad of mental health problems for transgender individuals. Many transgender individuals experience shame, self-hatred, anxiety and depression and may suffer from substance abuse and other harmful coping mechanisms as a result of the stigma and discrimination that is pervasive in contemporary society (Johnson et al., 2008). Because of the psychological impact that stigma and discrimination have on the transgender community, clinicians need to be aware of other mental health issues that often manifest in transgender individuals. Transition Related Healthcare Even though GID is considered a mental disorder and evidence shows that SexReassignment Surgery and hormones are effective ways to eliminate distress for transgendered individuals, many transgender-identified individuals struggle with getting their treatment paid for. Mental health services, hormones and surgical procedures are often denied coverage because they are seen as cosmetic rather than medically necessary (Byne et al., 2010). In a study conducted with over 2,000 patients who had undergone hormonal and/or surgical treatment to assist in their gender transition process, 87% of the MTF and 97% of the FTM participants reported improved psychosocial outcomes. Additionally, in another study of 325 subjects who had undergone Sex-Reassignment surgery, only 2% regretted having the procedure. Overall, both studies resulted in patients with less gender dysphoria and better psychological functioning (Feldman & Safer, 2009). However, even though medical transition procedures are shown to improve the well-being of transgender individuals, transition related costs are often extremely 33 expensive without insurance coverage and many transgender individuals go without transition related medical care (Johnson et al., 2008). With that said, for employed transgender individuals with insurance, there are some companies that will pay for transition related procedures. As of 2001, the city of San Francisco offers its city employees coverage for hormones and surgical procedures with a 15-50% copayment and maximum benefit of $50,000 (Penn, 2001). In 2007, the Human Rights Campaign reported that 67 firms are offering coverage for SexReassignment surgery including Wells Fargo, Johnson and Johnson and Toyota (Some Big Companies, 2007; Trans Rights, 2011). Moreover, the Veterans Administration has some of the most generous coverage for transition related care. The Veterans Administration provides health care for eligible transgender veterans, including SexReassignment surgery when it is deemed medically necessary. Additionally, a diagnosis of GID or Gender Dysphoria is not required in order for transgender veterans to receive services (VHA Directive, 2011). Unfortunately, even if surgical procedures are covered through certain companies, transgender individuals experience more unemployment and discrimination at work compared to the national average and thus, may have more trouble obtaining employment with decent transition related benefits. Furthermore, the work environment for employed transgender individuals may be toxic. In a national survey of the transgender community (n=6,450), 97% of respondents reported having experienced on the job harassment related to being transgender (Harmon, 2009). This shocking statistic suggests that even though there are some occupations that allow for transgender 34 individuals to receive transition related care; this does not make up for the gross inadequacies in other systems or for the rampant discrimination and stigma in the workplace. Mental Health and Transition Related Care The American Psychological Association (APA) plays a major role in transgender individuals receiving transition related healthcare. The APA has historically increased stigma for transgender individuals through asserting the GID diagnosis as valid and lacking solid guidelines for treatment. Both of these factors inadvertently support many insurance companies’ opinions that surgical procedures are in fact cosmetic. However, a recent APA Task force that was formed to investigate GID, concluded that APA needs to take a stance on effective treatment measures of care and issue a resolution that declares that hormonal and surgical treatments are medically necessary. Moreover, the APA acknowledged in their report, that their own silence coupled with the GID diagnosis has been stigmatizing to transgender individuals and therefore impedes their access to care. The APA declared the transgender community as one that is in the midst of a fight for civil rights and that treatment must not aim to make the community conform to standard care as it exists today (Byne et al., 2012). Additionally, the APA Task Force recommended that mental health professionals be given training in the area of transgender mental health care so that there are more competent service providers who are better prepared to work with the transgender community. In one study (n=93) of patient satisfaction amongst transgender individuals 35 receiving psychotherapy, there was a strong correlation between patients who were satisfied with their treatment and their psychotherapist possessing cultural competence pertaining to the transgender community (Bockting et al., 2004). Because most counseling treatments currently available further the concept of the gender binary and exclude transgender identities, these counselors are missing key information in successfully treating transgender individuals (Sanger, 2008). Currently, the APA recognizes that there are very few mental health professionals who are educated and therefore qualified to treat people with GID and Gender Dysphoria and even fewer who have direct clinical experience with transgender individuals (Byne et al., 2012). In order for transgender individuals to receive competent mental health services, mental health professionals must be trained specifically on the many societal and institutional issues that transgender individuals face. Although the World Professional Association for Transgender Health (WPATH) Standards of Care do not specify that psychotherapy is a mandatory part of a transgender individual’s path to surgery, it is a recommended part of the process when there is mental illness present. If there are co-morbid mental illnesses present such as a psychotic disorder, eating disorder or substance abuse, WPATH recommends that the individual seek treatment and show improvement before having Sex-Reassignment surgery. Treatment for co-morbid disorders may be obtained through the therapeutic process as well as through psychotropic medications. Additionally, if a transgender individual has a personality disorder, psychotherapy becomes one of the eligible criteria for surgery (De 36 Cuypere & Vercruysse, 2009). Some professionals see pre-operative psychotherapy as a way to lessen the chance of post-surgical regret experienced by some transgender individuals. Several studies show that transgender individuals who experience postsurgical regret are more likely to have not gone through the therapeutic process than those who are happy with their decision to pursue surgery. Additionally, some professionals suggest that post-operative patients can benefit from psychotherapy to assist them in their psychological and social adjustment after surgery (De Cuypere & Vercruysse, 2009). However, not everyone agrees with the current standards of care that designate a great deal of responsibility to mental health professionals. Some advocates for civil rights feel that mental health professionals sometimes act as “gatekeepers” who can too easily block a transgender person’s ability to seek medical transition related treatment (Lev, 2009, p. 75). Critics of mental health professionals’ involvement in the decision process question why transgender individuals cannot go directly to their primary care doctor for treatment (Lev, 2009). In response to this criticism, a current movement in the transgender community is evolving aimed at moving away from this authoritative way of providing healthcare into a more equal relationship between a provider and a consumer of care (Blockting, 2009). 37 Chapter 3 METHODS Study Objectives The present study sought to discover the availability of healthcare access and quality of healthcare services available to the transgender community living in the greater Sacramento area. The present study also sought to determine what barriers the transgender community faces when seeking general healthcare in addition to healthcare related to the process of transitioning medically. Past research has addressed healthcare disparities and barriers to healthcare faced by the transgender community in obtaining adequate healthcare in other parts of the country. The current study sought to determine what barriers exist and how to improve healthcare access for transgender individuals living in the greater Sacramento region. The current study utilized data from live interviews and was analyzed through a qualitative analysis of the data. Study Design The research design for this Master’s project was predominantly exploratoryqualitative. The researcher found participants through the Gender Health Center, a nonprofit counseling agency that specializes in treating transgender-identified individuals. Several transgender-identified individuals who are also transsexual (post medical transition), medical professionals Social Work professors who are experts in the field and community advocates were interviewed about their perceptions of healthcare disparities within the community. The interview questions sought to address how much access to 38 healthcare there is in the greater Sacramento area and what barriers exist for transgender individuals such as insurance/MediCal coverage, access to the medical transitioning process and possible solutions to identified barriers. Additionally, these same individuals were interviewed regarding their perceptions of how competent medical professionals are in working with the transgender community and how healthcare access and healthcare quality could be improved for transgender individuals in the greater Sacramento area. The researcher also interviewed participants regarding their experiences and opinions of the Gender Identity Diagnosis and how helpful this is in accessing healthcare. The researcher sought diversity in participants in order to provide many different perspectives, thus illustrating the full scope of what is currently going on in the greater Sacramento region in regards to transgender related healthcare. Sampling Procedures The researcher used settings to interview participants that were comfortable and in a public place such as a coffee shop or public park. Participants who self-identified as transgender and transsexual (post medical transition) in addition to several experts in the field (social workers, medical doctors, community advocates, nurses) were selected through the researcher’s internship at the Gender Health Center, a non-profit mental health agency that specializes in transgender concerns and serves the entire Lesbian, Gay, Bisexual, Transgender, Queer (LGBTQ) community. The researcher interviewed three transgender and transsexual self-identified individuals, two Social Work Professors with specific knowledge about this community, two medical doctors, one registered nurse and 39 four community advocates, all located within the greater Sacramento area to discover how much healthcare access the transgender community has and how adequate healthcare services are. The Gender Health Center assisted the researcher in finding potential research participants. The researcher approached the potential participants at the Gender Health Center by asking them if they would be interested in participating in her research. After the participants expressed interest, the researcher met with each participant individually at public locations in Sacramento. The researcher went over the consent forms with each individual research participant and had each person sign and date the consent form (see Appendix A). After obtaining consent, the researcher asked the participants detailed questions about access to healthcare, barriers to healthcare and possible solutions to these barriers and recorded the answers on a tape recorder. The consent form informed participants of their right not to be recorded. Interviews were conducted at the participants’ convenience, at a public location that was convenient to the participant. The only people who had access to the recorded interviews as well as all other data for this research project were the researcher and her faculty advisor, Dr. Serge Lee. After the research project was complete, all data, including notes and voice recordings were destroyed so that there was no potential leakage of confidential data. The data were destroyed on May 19, 2013. All subjects were informed of these procedures upon signing the consent form. 40 Instruments The researcher composed the questionnaires prior to meeting with participants. The interviews differed based on the population being interviewed. The interview for Social Work Professors and Community advocates consisted of eight questions. The interview for Medical Doctors and Nurses consisted of nine questions. The interview for transgender and transsexual-identified individuals contained 22 questions. The interviews all contained questions regarding perceived access to transition related and non-transition related healthcare, mental and physical healthcare accessed in the past year, insurance coverage, perceptions of medical and mental health professionals competence in caring for transgender-identified individuals and perceptions of the Gender Identity Disorder (DID) diagnosis as a key tool in getting transition related health care paid for by insurance companies (see Appendix B). The interview also sought basic demographic information from transsexual participants such as education level, age, socio-economic status, racial background and type of employment. Data Analysis The data for this research project were gathered from the interviews conducted with voluntary participants. The researcher performed a qualitative analysis of the data. Protection of Human Subjects The researcher submitted a Human Subjects Protocol Application to the Institutional Review Board (IRB) that discussed the research purpose and proposed methods. Before submitting her application to the IRB board, the researcher first 41 submitted her Human Subjects Protocol Application to her advisor to review. Her advisor, Dr. Serge Lee, suggested some modifications to the researcher’s consent forms including the approximate duration of the interview on the consent form as well as modifying her formatting. After modifying her application, the researcher submitted her application to the IRB on October 26, 2012. On November 8, 2012, the researcher received her application back with the status of approved with minimal risk with conditions. The conditions were to indicate that participants had the right not to be audio taped, to delete information regarding medical care in the consent form and to delete age, ethnicity, education level, and income level for social workers, medical doctors, and nurses or provide reason for their inclusion. After receiving approval with conditions, the researcher removed the demographic questions from the questionnaires for social workers, community advocates, and medical professionals and added a clause in the consent form about participants being able to decline being audiotaped. The researcher also removed the medical contacts from the consent form. The researcher submitted her modified application for full approval to the IRB on December 7, 2012. The researcher was granted full approval to begin conducting her research on February 1, 2013. The research project was approved as minimal risk with the protocol number 12-13-029. 42 Chapter 4 STUDY FINDINGS AND DISCUSSIONS The transgender community has been marginalized when it comes to receiving adequate healthcare (Brockett et al., 2007). The researcher sought to interview a variety of health professionals, transsexual individuals and community advocates in order to get a full picture of how much access the Sacramento area transgender community has to health care services and the quality of care available. Overall Findings The researcher interviewed two Social Work Professors at Sacramento State University who have knowledge regarding the transgender community as well as four Sacramento area community advocates for the transgender community. The researcher also interviewed two family practice medical residents who volunteer at a local hormone clinic run by the Gender Health Center for transgender individuals in Sacramento and one registered nurse who works in the Emergency department of a busy Sacramento hospital. Additionally, three transsexual, (post-transition) transgender identified individuals living in the Sacramento area were interviewed regarding their own personal experiences in accessing healthcare. Demographic information was collected for each transsexual participant. All three transsexual participants were Caucasian male to female (MTF) transgender identified individuals. There was a range in age of transsexual participants and included one 42-year-old, one 31-year-old and one 46-year-old. Education level also varied and included one participant with her bachelor’s degree, one participant with her 43 master’s degree and one participant with her General Education Diploma (GED). Two participants reported making less than $11,000 a year and one participant reported a yearly income of $95,000. Two participants were currently unemployed and the third stated her occupation as a “Software Engineer.” Two of the transsexual participants had accessed physical health care services within the last year and one had not. All three of these participants had accessed mental health services within the last year. Additionally, all three of these participants reported to feeling comfortable when seeking medical care and mental health services. Specific Findings Medical Professionals Two family practice resident physicians who volunteer at the Gender Health Center’s hormone clinic were interviewed for this research project. Additionally, one registered nurse who is employed in an emergency department in the Sacramento area was interviewed for the present study. All three professionals reported to having had contact with transgender individuals in their work setting. The two medical doctors had a lot of contact with transgender individuals in their work as volunteer physicians at the hormone clinic. Each physician had seen a transgender individual diagnosed with Gender Identity Disorder (GID) within the last year and one reported to diagnosing a person as having GID for “insurance purposes.” The registered nurse reported that the single transgender patient that she had seen in the last year did not have a GID diagnosis. Both physicians mentioned being opposed to the Gender Identity Disorder diagnosis. 44 Statements included “we’re fighting to get rid of the disorder and embrace the gender identity part” and “I’ll write in a diagnosis for GID but I don’t put it in their chart.” The nurse stated that diagnosing patients is outside of her scope of practice. Three open-ended questions were asked regarding these medical professionals’ perceived competence in treating transgender individuals for their medical and psychological needs. Additionally, one open-ended question was asked that sought to find out how each professional felt she could increase competency. Both doctors reported to feeling very competent in treating the transgender population’s medical needs, although less competent at treating and understanding the transgender community’s psychological needs. The registered nurse reported to feeling competent in treating the transgender community’s non-transition related medical needs but incompetent in treating transition related medical needs. Additionally, the registered nurse stated that she could use more education surrounding the biopsychosocial needs of the transgender community. Responses for perceived competence in medical needs included “I feel competent,” “I feel I’m comfortable treating them” and “very competent in medical needs but not so much for transition related needs.” Responses to perceived competence regarding psychological needs included “I think that’s a little bit trickier,” “on a scale of one to five I’d be a three if competent was a three and extremely competent was a five” and “I don’t remember studying their biopsychosocial needs in nursing school.” All three medical professionals were also asked what they would need to feel more competent in treating transgender individuals. Both doctors and the registered nurse responded that 45 they needed more training on the needs of the transgender community. Responses included “more training in the social aspects,” “more data and studies,” “class or reading material addressing transition related medical complaints” and “more experience.” Two open-ended questions were asked regarding imagined or observed barriers for transgender individuals seeking healthcare and potential solutions to these barriers. Both doctors cited lack of education among medical professionals as a barrier to healthcare access. The registered nurse reported that lack of training amongst providers in addition to gender segregated hospital rooms could be barriers for transgender patients. Specific responses to identified barriers included “there’s a lot of physicians out there that have no idea what’s going on,” “the physician is completely ignorant or unwelcoming of transgender patients,” “confusion among providers” and “rooms are usually shared by two females or two males. Transgender individuals would most likely be given a private room”. Additionally, one physician described how many physicians “weren’t familiar with continuing screening and combining services for [transgender individuals’] birth sex if they still have those organs.” The same physician cited “prejudice and not knowing how to respond to patients” as being a barrier to healthcare access. When asked about solutions to these identified barriers, both doctors and the registered nurse cited education efforts as being key. Responses included “education, cultural change and general awareness of transgender issues and transgender people,” “awareness and sensitivity training” and “more staff education on transition related medical complaints and on the biopsychosocial needs of the transgender community.” 46 Social Work Professors and Community Advocates Two Social Work Professors who have experience working with the transgender community as well as four community advocates were interviewed about the potential barriers to proper healthcare access that transgender individuals face. One open-ended question was asked regarding what barriers the transgender community faces when seeking healthcare. Several participants cited incompetent providers as being one of the main concerns. Responses included “incompetent providers,” “lack of competent professionals,” “[transgender individuals] are pathologized or turned down by their doctors, turned away and not even treated,” “physicians either don’t have enough knowledge of transgender issues or they don’t want to know about it” and “they’re (medical doctors) just not educated.” Other barriers identified included societal transphobia and lack of insurance coverage. Responses included “transphobia,” “access to health insurance,” “insurance companies don’t cover a lot of things transgender people need,” “a lot of procedures and surgery are not covered by insurance,” “the private insurance based system,” and “transphobia in our culture and society.” Two open-ended questions were asked regarding what knowledge each participant had on insurance company policies pertaining to transgender related health care. All participants agreed that insurance companies do not cover most transition related health care and that the services that are covered are hard to navigate and actually obtain for transgender individuals. Responses included “in general, there’s not a lot of coverage for it,” “it’s a difficult process,” “there’s a lot of things the insurance company 47 does cover but they don’t tell you they cover it,” “each person attempting to receive transgender-related care is going to have a different experience” and “Medical and Medicare have been quite a challenge to deal with.” One participant talked about certain insurance companies that do cover transition related healthcare. This participant stated that companies such as UC Davis, Hewlett Packard and the Veterans Administration covered most transition related care. Two open-ended questions inquired into each participant’s opinion of perceived competence among medical and mental health professionals when it comes to working with the transgender community. Many participants described that medical professionals and mental health professionals are largely incompetent when it comes to treating transgender individuals. Responses for perceived competence among medical doctors included “not very [competent] at all unless they are hormone specialists,” “if you see a general physician because you have a cough and they see that you’re taking these hormones, they won’t know what they do,” “not very competent,” “not competent,” “they need more training on it” and “95% of doctors have no idea or awareness about the issues.” Responses for perceived competence among mental health professionals included “you hear stories from folks who tried to access therapy and it didn’t go well,” “on average, not very” and “as a whole, they’re not very competent” and “they’re not competent because there isn’t any training in graduate schools about mental health work with transgender folks.” 48 One open-ended question asked each participant to give their opinion about the Gender Identity Disorder (GID) diagnosis and proposed Gender Dysphoria diagnosis and how helpful or unhelpful it is for transgender individuals seeking healthcare. Almost all of the participants acknowledged that having a diagnosis assists transgender individuals in getting transition related care covered but also hurts individuals with the stigma such labels perpetuate. Responses included “you need a label in order to get assistance in insurance coverage but the label can be a very real and painful aspect of one’s life,” “It’s a double edged sword. It’s good to have a label so you can get the services that you need but…it leaves people feeling like something is wrong with them,” “it’s good for insurance but it doesn’t make them feel good that just because they’re trans, they have a disorder,” “I understand they need a code to write down but transgender folks should be covered without needing a mental health diagnosis,” and “I strongly oppose the GID diagnosis because it says in black and white that it’s a disorder just to cross identify. I think ideally, it should be a medical condition, not a psychiatric condition.” One participant did not agree that the diagnoses are helpful for transgender people at all. This participant’s response to the question stated, “I’m glad they are getting rid of Gender Identity Disorder. People internalize the diagnosis as a disorder and this will help people realize that they are not crazy.” One open-ended question asked participants what solutions they proposed in order to ensure that the Sacramento area transgender community has access to satisfactory healthcare. Proposed solutions were varied and included educating professionals, 49 creating more transgender focused community health clinics and advocating and empowering those in the transgender community. Specific responses included “changing healthcare and insurance policies,” “more clinics and health centers like the Gender Health Center,” “physicians to become more aware,” “advocacy,” “train professionals and empower individuals,” “education and legislative advocacy,” and “community clinics where we are modeling our care after transgender specific needs because when you’re able to provide for the most marginalized community within a marginalized community, you end up providing for a wider, regional community.” Transsexual Identified Individuals Four open-ended questions were asked regarding what barriers each participant had experienced in finding and receiving adequate transition and non-transition related mental and physical healthcare and what potential solutions to these barriers could be. Barriers that participants faced when seeking transition related care included not knowing where to access services, not having insurance coverage and experiencing a lack of professionals that are educated about the transgender community’s needs. Responses included “I don’t have any insurance,” “it wasn’t easy to gain access to hormones,” “I haven’t seen a general practitioner in 6 years” and “the biggest hurdle was finding people that have the knowledge to help, especially [with] psychological help.” In seeking non-transition related medical care, respondents reported that money and lack of insurance coverage was the largest barrier that they faced. One participant reported having insurance coverage through Kaiser Permanente; however, the other two 50 participants reported having no insurance coverage. Responses about the barriers to accessing non-transition related care included “no insurance” and “it’s a lot of money,” third participant’s response (with insurance). In responding to what solutions could help alleviate these barriers, participants identified educating medical doctors and mental health professionals about transgender related health care and requiring that doctors treat transgender patients. Responses included “they need to start educating and they need to help people despite how they feel about their lifestyle” and “more education for doctors and providers.” Other identified solutions included “more community agencies specializing in transgender issues” and “a national insurance program.” Since two participants were uninsured, only one participant could answer the question about how helpful insurance has been in covering transition related care. This participant answered, “they covered hormones but that’s it.” Four open-ended questions were asked in regards to personal experiences that informed each participant’s opinion about mental health professionals and medical doctors’ competence in treating transgender individuals. Each participant described personal experiences with medical doctors who they felt were incompetent in treating transgender individuals. Responses included “they’re not [competent] at all unless they have been doing it for a while” and “not competent.” One participant, who accessed the hormone clinic that the Gender Health Center provides, stated that the doctors were “quite competent.” The participants’ experiences with mental health professionals varied. Participants who sought mental health services through the Gender Health Center 51 found mental health professionals to be more competent than the participant who went outside of the center for therapy. Responses from participants who saw someone from the Gender Health Center included “not competent but open to learning” and “this was the first time I ever had a counselor who I don’t have to educate.” The third participant described seeing a mental health professional who was not affiliated with the Gender Health Center. This participant described this particular mental health professional as being “not competent” when it came to issues of gender identity. One open-ended question inquired into participant’s opinions of the Gender Identity Disorder (GID) diagnosis/ proposed Gender Dysphoria diagnosis. One participant reported liking the diagnosis and feeling that there needs to be stronger gateways to getting hormones and beginning a medical transition due to her personal experience in seeing “lives ruined” from transitioning. Her response included “I think the gateways are there for a reason and need to stay there. I think they could be a little bit tighter even.” Another participant had opposite feelings about the diagnoses. This participant responded, “I don’t like the disorder diagnosis…it has nothing to do with my mind.” The third participant acknowledged both the harmful and helpful aspects of the diagnoses. This participant responded, “It’s a double edged sword. I feel like I don't want it in there, I don't feel it's a disorder, but I know that the medical community needs something on paper in order for them to really provide services.” The last question asked participants what they feel needs to happen for the transgender community to receive adequate healthcare. All three participants agreed 52 professionals need more training and education. Responses included “training,” “educate” and “awareness.” Other responses included “people need to change their attitude,” “more affordable services” and “easier access to information about the process to receive services.” Interpretations of the Findings The results portray certain themes throughout the interviews with a variety of individuals involved in the Sacramento region’s transgender community. These themes offer a lens into the availability of healthcare access and quality of care for the transgender community in the Sacramento region. Most of the interview participants cited lack of competent and knowledgeable medical and mental health professionals as one of the key barriers that exists for transgender individuals seeking adequate healthcare. Additionally, many participants identified transphobia and ignorance among health professionals as another common barrier to accessing good healthcare. All participants identified education, training and spreading awareness as being key tools to addressing these barriers that currently exist for transgender patients. The opinions of the participants about the Gender Identify Disorder (GID) and proposed Gender Dysphoria diagnoses varied somewhat. The views varied among each group of participants interviewed. Opinions varied greatly from one participant agreeing with the diagnosis and believing there needs to be stricter gateways to accessing hormones and surgeries, to a the diagnosis becoming a medical one instead of a mental health disorder, to wanting to get rid of a diagnosis for transgender individuals entirely. 53 Many participants saw the diagnoses as having benefits in that the diagnosis merits medical coverage for transition related care and negative consequences pertaining to the stigma and pathologizing of the transgender identity that the diagnoses help further. Both medical doctors admitted that the GID diagnosis is helpful in getting insurance companies to cover transition related medical needs; however, the nurse reported to seeing a transgender patient that did not possess the diagnosis. The nurse was unaware of the individual’s insurance situation and so one cannot know if the GID diagnosis was needed for potential coverage for treatment. The results about how much insurance coverage there is for transgender-identified individuals also varied. Two of the transsexual participants interviewed had no health insurance whereas the third possessed a high paying job and reported having good health insurance. However, the one transsexual participant interviewed who possessed health insurance coverage, reported that insurance only covered hormones and no other medical interventions related to her medical transition. Several participants identified lack of access to insurance in addition to lack of coverage for medical procedures for those who are insured as major barriers to healthcare for the transgender community. Additionally, several participants cited a confusing insurance system where it is unclear what is covered and what is not as being another barrier to healthcare. Several participants mentioned a change in our health care system as well as National Health Insurance program as being solutions to barriers to healthcare access. Furthermore, many participants described needing more community health agencies specializing in the needs 54 of transgender individuals such as the Gender Health Center as a solution to the lack of access to care. Summary In examining results from interviews with health professionals, transsexual individuals, Social Work professors with knowledge about the transgender community and other community advocates, we see a clearer picture of what is getting in the way of transgender individuals seeking and obtaining adequate healthcare, in addition to some possible solutions to these barriers. Incompetent and ignorant medical and mental health professionals and the need for more training and education about the medical and psychological needs of the community are barriers to the transgender community when it comes to receiving adequate care. Additionally, transphobia in our society as well as stigmatization related to the Gender Identity Disorder/proposed Gender Dysphoria diagnoses perpetuate and create barriers that exist for transgender individuals. Lastly, lack of insurance access in addition to confusing policies and lack of insurance coverage for transition related medical needs prevents many transgender individuals from obtaining both transition and non-transition related medical care. National Health Care programs as well as more community health centers specializing in the transgender community were identified as solutions to the barriers with health insurance companies. 55 Chapter 5 CONCLUSION, SUMMARY, AND RECOMMENDATIONS Summary of Study The present study sought to examine the availability and quality of healthcare for transgender individuals in the greater Sacramento region. In this chapter, I first identify evidence from the present study that did or did not support the research hypothesis and discuss possible reasons for these results as related to the review of the literature. Following, I present the limitations of the present study in addition to the implications for Micro and Macro Social Work practice. Lastly, I make suggestions for future research. Discussion The researcher expected to find that healthcare access for the transgender community in the Sacramento region was going to be grossly inadequate. This hypothesis was largely validated through the present study’s results. Past research shows that transgender individuals are the largest uninsured group in the LGBTQ community. Additionally, the transgender community experiences high rates of denials to proper treatment whether from insurance or providers due to their gender identity (Johnson et al., 2008, Kenagy, 2005). The present study indicated that lack of insurance access and coverage is a major barrier for transgender individuals in the Sacramento region. Two of the transsexual participants interviewed did not currently possess health insurance and the other participant with insurance coverage reported that insurance only covered hormones. Additionally, such as the researcher suspected, several participants identified better 56 insurance access and coverage as well as a National health insurance program as solutions to these barriers. Insurance access and transition related coverage appear to be two of the main factors that need to be addressed in order for transgender individuals to receive proper healthcare. Supplemental to the results from the interviews with participants is the researcher’s perusing of local private insurance plans in the Northern California area as well as looking into what MediCal covers. Two local private health insurance plans stated that the transgender patient would be denied a private insurance policy simply based on their Gender Identity Disorder (GID) diagnosis. When looking into MediCal coverage, the researcher found a complicated web where it was unclear what was covered and what was not. In looking at a group plan through a local University, the researcher found through this insurance plan, every transgender patient has access to transition related medical care up to a lifetime limit of 75,000 dollars. However, one has to be an employee of the University to access these benefits. Several participants in the current study mentioned that insurance coverage is a confusing network to navigate and often times it is unclear what is covered and what is not covered. Additionally, the one transsexual participant who reported having health insurance described that her insurance company solely covered her prescribed hormones and nothing else transition related. It appears that insurance coverage for transition related medical needs differ between different group insurance policies and that private plans may not even take a transgender patient in the first place. Because the participant 57 that possessed insurance coverage was employed with a salary of $95,000 annually, she was able to sign up for a group plan through her work that provided some transition related coverage. However, the two other transsexual individuals who reported annual incomes below $11,000 had no insurance coverage. It appears from the present study and independent research into local health insurance policies, that private insurance policies are difficult for transgender individuals to be approved for, especially if they have a GID diagnosis and that many insurance companies are confusing to navigate when it comes to transition related medical coverage. The researcher also sought to determine the consensus on whether the Gender Identity Disorder (GID) diagnosis/proposed Gender Dysphoria diagnosis was helpful or harmful to the transgender community when seeking satisfactory healthcare services. Previous research shows that critics of the diagnosis view the fact that transgender individuals are labeled with a mental disorder, as feeding the stigma and discrimination that exists towards the transgender community. However, previous research indicates that the GID diagnosis can be also be extremely helpful in getting insurance companies to cover transition related health care services (Sennott, 2011). The present study found varied opinions of the diagnoses and how helpful or harmful they can be, similarly to previous research done on the subject. One interesting finding is related to the transsexual participant who reported liking the GID diagnosis and desiring even further “gateways” for individuals seeking to transition. Because this participant is Caucasian, upper-middle class and possesses adequate health insurance and resources to pay for 58 procedures that aren’t covered, she may not see the negative effects of the diagnoses or experience the stigmatizing nature of the diagnoses as other transgender individuals who are less financially stable might experience. However, even though this participant had a view that differed from the rest of the participants on the GID/Gender Dysphoria diagnoses, this participant still reported to having personally experienced both mental health professionals and medical professionals who were incompetent and ignorant about the medical and psychological needs of transgender individuals. Previous research shows that both medical professionals and mental health professionals are lacking in knowledge about the transgender community (Lombardi, 2001). Likewise, almost all of the participants in the present study identified education, training and efforts towards awareness for health professionals as being key to transgender individuals obtaining proper healthcare. Furthermore, many participants mentioned that community health centers like the Gender Health Center in Sacramento that specialize in transgender needs could also be a solution to the lack of quality healthcare available for transgender individuals. One community advocate discussed how community health centers such as the Gender Health Center focus on the most marginalized community within the LGBTQ community and therefore are able to serve the entire community. Because of this, medical and mental health clinics that specialize in the needs of the transgender community could be part of the solution towards greater healthcare access and better services for transgender individuals. In addition to health clinics, the results make clear that there needs to be more training and educational efforts 59 aimed towards health professionals in the Sacramento region surrounding cultural competency. The overwhelming mention of incompetent professionals in the current study from transsexual participants, community advocates and health professionals suggests the lack of culturally competent professionals in the Sacramento region, not unlike previous research done in other parts of the country. Previous literature identified gender segregated bathrooms as a barrier to healthcare for transgender individuals. Similarly, the Registered Nurse who was interviewed for the present study reported that transgender patients would be given a private room in a hospital due to their gender identity. Previous research and the Nurse’s report make clear that health professionals are largely uneducated surrounding the needs of transgender community. With this said, all three transsexual participants interviewed reported being comfortable seeking mental health and physical health care. This could be due to the fact that Sacramento has the Gender Health Center that provides mental health services as well as a hormone clinic for transgender individuals and specializes in the needs of the transgender community. Had the researcher interviewed transsexual participants that were unfamiliar with the Gender Health Center, she could have seen different results with transsexual individuals that reported feeling uncomfortable seeking healthcare services. Additionally, had the researcher interviewed transgender individuals prior to their medical transition, the comfort levels in accessing care could have been different. 60 Social Work Implications The present study contains many useful implications for social workers that are employed in both micro and macro level positions. Social workers, like medical professionals, need to be educated about transgender issues in order to be culturally competent in their practice. The present study portrays the fact that many clinicians remain ignorant about the psychosocial needs of the transgender community. Social workers in the clinical realm need to be aware of the stigma and prejudice that the transgender community faces and the psychological impacts on individuals and on the community as a whole. Additionally, clinical social workers need to learn about what language to use with transgender-identified individuals, such as using a transgender person’s preferred pronoun when addressing a client. Moreover, social workers that diagnose clients need to be careful when diagnosing a transgender person with Gender Identity Disorder/ Gender Dysphoria and not use these diagnoses in a pathologizing manner. Through the interviews done with transsexual participants, a wide range of opinions emerged about the use of the GID diagnosis; however, most of the participants agreed that the fact that the diagnosis is considered a mental illness is inherently stigmatizing. With that said, as many participants pointed out in the present study, it may be necessary to utilize the diagnoses for insurance coverage purposes. Macro level social workers that are working in advocacy and policy positions need to be aware of the transgender community’s marginalized status, even within the LGBTQ community. When social workers fight for social justice for the LGBTQ 61 community, they should keep the transgender community’s needs in mind instead of solely sticking them under the umbrella of LGBTQ and subsequently forgetting about the unique issues that this community faces with problems in accessing healthcare, stigma and discrimination. Social workers that are employed in policy design and implementation should make sure that the policies that they create are transgender friendly and do not further marginalize the community. Future Research The present study also provides several ideas for future research in this area. Because training, education and awareness were identified as potential solutions to incompetent health care providers, the researcher recommends that future research studies focus on the best ways are to educate and train mental and medical health professionals in the needs of the transgender community. Once education and training efforts have been implemented, the researcher recommends that these programs be analyzed for their effectiveness and whether increased knowledge decreases the marginalization of the transgender community and increases the quality of and access to healthcare. Another recommendation for future research is to determine the impact on the transgender population once Gender Identity Disorder is taken out of the next edition of the Diagnostical and Statistical Manual on Mental Disorders and replaced with Gender Dysphoria. Because the new diagnosis could theoretically be less stigmatizing, it has the potential to decrease discrimination and pathologization of the community. It will also be interesting to see how the new diagnosis affects insurance coverage for transition related 62 care. Additionally, with the Affordable Care Act being instituted in 2014, the researcher recommends that further research be done on how the new health care system impacts the transgender community’s access to health care. Lastly, this researcher recommends that future researchers study how culturally accepted binaries of gender are impacted by increased awareness and education about the transgender identity. It is the hope of this researcher that through lessening the grip on socially constructed ideologies of gender and breaking through these binaries, the transgender community will experience less discrimination, stigma and greater access to healthcare. 63 APPENDICES 64 APPENDIX A Consent Forms Consent to Participate in Research: Medical Professional/Mental Health Professional/Expert in the Field/ Community Advocate Purpose of the research You are being asked to participate in research that will be conducted by Annie Temple, a graduate student in the Division of Social Work at California State University, Sacramento. The purpose of the study is to investigate the current access and barriers to healthcare available to the transgender community in Sacramento. Research procedures Upon written consent, you will be given an interview regarding your perceptions of questions related to the availability, quality, barriers, and general access to healthcare for transgender individuals in Sacramento. The interview will be audiotaped and will require approximately 30 minutes of your time. Risks I want to inform you that some of the questions in the interview may seem personal, but you don’t have to answer any if you don’t want to. You have the right to not be audio taped and the interview will not be taped if you don’t want it to be. You may participate as much or as little in the interview as you wish. In addition, I want to let you know that you can stop the interview at any time with no explanation required. Benefits You may not personally benefit from participating in this research. However, it is hoped that the results of the study will be beneficial to the Transgender community in identifying current barriers in healthcare access and proposing potential solutions to these barriers. Confidentiality I want you to know that your responses to the questionnaires will be anonymous. A pseudonym will be used when reporting the data to protect your privacy. With your permission, the interview conducted will be audio taped. Those tapes will be destroyed as 65 soon as the interviews have been transcribed, and in any event no later than one year after they were made. Until that time, they will be stored in a secure location. All results reported will be completely confidential. Compensation Unfortunately, you will not receive any compensation for participating in this research. If you have any questions about this research, you may contact the researcher, Annie Temple at 530-219-6703 or by email at annielouisetemple@gmail.com. You may also contact her faculty advisor, Dr. Serge Lee at 916-278-5820 or by e-mail at lees@saclink.csus.edu. You may decline to be a participant in this study without any consequences. Your signature below indicates that you have read this page and agree to participate in the research. ________________________________ Signature of Participant ____________________ Date 66 Consent to Participate in Research: Transsexual Participants Purpose of the research You are being asked to participate in research that will be conducted by Annie Temple, a graduate student in the Division of Social Work at California State University, Sacramento. The purpose of the study is to investigate the current access and barriers to healthcare available to the transgender community in Sacramento. Research procedures Upon written consent, you will be given an interview regarding your perceptions of questions related to the availability, quality, barriers, and general access to healthcare for transgender individuals in Sacramento. The interview will be audiotaped and will require approximately 30 minutes of your time. Risks I want to inform you that some of the questions in the interview may seem personal, but you don’t have to answer any if you don’t want to. You have the right to not be audio taped and the interview will not be taped if you don’t want it to be. You may participate as much or as little in the interview as you wish. In addition, I want to let you know that you can stop the interview at any time with no explanation required. Benefits You may not personally benefit from participating in this research. However, it is hoped that the results of the study will be beneficial to the transgender community in identifying current barriers in healthcare access and proposing potential solutions to these barriers. Confidentiality I want you to know that your responses to the questionnaires will be anonymous. A pseudonym will be used when reporting the data to protect your privacy. With your permission, the interview conducted will be audiotaped. Those tapes will be destroyed as soon as the interviews have been transcribed, and in any event no later than one year after they were made. Until that time, they will be stored in a secure location. All results reported will be completely confidential. Compensation 67 Unfortunately, you will not receive any compensation for participating in this research. If you are interested in talking more about these issues or desire counseling services, you may contact Ben Hudson, Executive Director of the Gender Health Center at 916-4552391. If you have any questions about this research, you may contact the researcher, Annie Temple at 530-219-6703 or by email at annielouisetemple@gmail.com. You may also contact her faculty advisor, Dr. Serge Lee at 916-278-5820 or by e-mail at lees@saclink.csus.edu. You may decline to be a participant in this study without any consequences. Your signature below indicates that you have read this page and agree to participate in the research. ________________________________ Signature of Participant ____________________ Date 68 APPENDIX B Questionnaires Interview for Social Work Professors who are Experts in the Field/Community Advocates Occupation: In your opinion, what are the current barriers that the greater Sacramento area transgender community faces when seeking adequate physical and mental health care? In your opinion, what needs to happen for the reduction/elimination of these barriers? Do you have any knowledge about insurance company policies on the coverage of transition related health care? What has your experience been with clients/acquaintances who attempt to seek coverage for transition related care? In your opinion, how competent do you think medical doctors are in transgender related health care? Please explain your opinion. In your opinion, how competent do you think mental health professionals are in transgender related mental health care? Please explain your opinion. What is your personal opinion about the Gender Identity Disorder/ proposed Gender Dysphoria diagnosis? How helpful/unhelpful do you feel these are for transgender individuals in receiving proper mental/physical healthcare? What solutions do you propose to ensure that the Sacramento area transgender community has access to satisfactory healthcare? 69 Interview for Medical Doctors/Nurses Occupation: How competent do you feel you are when it comes to treating transgender patients for non-transition related medical needs? How competent do you feel you are when it comes to treating transgender patients for transition related medical needs? How comfortable/competent/educated do you consider yourself when it comes to the bio/psycho/social needs of the transgender community? What would you need in order to feel more competent/comfortable as a medical service provider to transgender individuals? How much contact have you had with transgender individuals in the last year of your practice? How many patients have you seen with a Gender Identity Disorder (GID) diagnosis? How many times during the last year have you diagnosed someone as having GID? What barriers have you observed or imagine exist for transgender individuals when seeking sufficient healthcare? In your opinion, what are the potential solutions to these identified barriers? 70 Interview for Transsexual Individuals Age: Ethnicity: Occupation: Education Level: Income Level: What kinds of barriers have you personally experienced in finding/receiving adequate transition related mental and physical healthcare? In your opinion, what needs to happen for the reduction/elimination of these barriers? What kinds of barriers have you personally experienced in finding/obtaining adequate non-transition related mental and physical healthcare? In your opinion, what needs to happen for the reduction/elimination of these barriers? Are you insured? If so, who is your insurance company? If you do have health insurance, how helpful has insurance been in obtaining/getting coverage for adequate mental/physical healthcare? If you do have health insurance, how helpful has insurance been in obtaining/getting coverage for transition related healthcare? How competent do you feel medical doctors are when it comes to transgender related health care? What personal experiences do you have with doctors’ competence/incompetence when treating transgender individuals? What is your personal opinion about the Gender Identity Disorder (GID)/ proposed Gender Dysphoria diagnosis? How helpful/unhelpful do you feel it is for you when trying to obtain proper mental/physical healthcare? Have you utilized mental health services in the last year? If yes, how competent were these mental health professionals in transgender related care? Have you utilized physical health care services in the last year? 71 If yes, how competent were these medical professionals in transgender related care? If not, what is your reason behind not utilizing these services? How comfortable do you/would you feel in seeking mental health care? How comfortable do you feel in seeking physical health care? In your opinion, what needs to happen for transgender identified individuals to receive satisfactory healthcare? 72 REFERENCES Alegria, C. (2011). Transgender identity and health care: Implications for psychosocial and physical evaluation. Journal of the American Academy of Nurse Practitioners, 23(4), 175-182. American Psychiatric Association (APA). (2000). Diagnostic and statistical manual of mental disorders (4th ed., text rev.). Washington, DC: Author. Bockting, W. O. (2009). Transforming the paradigm of transgender health: A field in transition. Sexual & Relationship Therapy, 24(2), 103-107. doi:10.1080/14681990903037660 Bockting, W. W., Robinson, B. B., Benner, A. A., & Scheltema, K. K. (2004). Patient satisfaction with transgender health services. Journal of Sex & Marital Therapy, 30, 277-294. Bouman, W., Bauer, G., Richards, C., & Coleman, E. (2010). World professional association for transgender health consensus statement on considerations of the role of distress (criterion d) in the DSM diagnosis of gender identity disorder. International Journal of Transgenderism, 12, 100-106. Brockett, D., McNair, A., & Suniewick,Brockett E. (Directors). (2007). Transforming health care. [Film]. USA. Butler, J. (1988.) Performative acts and gender constitution: An essay in phenomenology and feminist theory. The Johns Hopkins University Press, 40, 519-531. 73 Byne, W., Bradley, S., Coleman, E., Eyler, A., Green, R., Menvielle, E. J., MeyerBahlburg, H. F.,…Tompkins, D. A. (2012). Report of the American Psychiatric Association task force on treatment of gender identity disorder. Archives of Sexual Behavior, 41, 759-796. Cavender, A. (2011). Sexually sidelined. Nursing Standard, 25(22), 26-27. Chapman, R., Watkins, R., Zappia, T., Combs, S., & Shields, L. (2012). Second-level hospital health professionals' attitudes to lesbian, gay, bisexual and transgender parents seeking health for their children. Journal of Clinical Nursing, 21, 880887. De Cuypere, G., & Vercruysse, H. (2009). Eligibility and readiness criteria for sex reassignment surgery: Recommendations for revision of the WPATH standards of care. International Journal of Transgenderism, 11, 194-205. Department of Veterans Affairs. (2011, June 9). VHA Directive 2011-024. Washington, DC: Author. Retrieved from www.paloalto.va.gov/docs/VA_Transgender_Directive.pdf Feldman, S., & Safer, J. (2009). Hormone therapy in adults: Suggested revisions to the sixth version of the standards of care. International Journal of Transgenderism, 11, 146-182. Ford, Z. (2012). APA revises manual: Being transgender is no longer a mental disorder. Retrieved from http://thinkprogress.org/lgbt/2012/12/03/1271431/apa-revisesmanual-being-transgender-is-no-longer-a-mental-disorder/?mobile=nc 74 Grossman, A. H., & D'Augelli, A. R. (2006). Transgender youth: Invisible and vulnerable. Journal of Homosexuality, 51(1), 111-128. Harmon, A. (2009). The gender identity divide. Advocate, (1033/1034), 50-52. Hines, S. (2007). Transforming gender: Transgender practices of identity and intimacy. Great Britain: Policy Press. Hulstein, M. J. (2012). Recognizing and respecting the rights of LGBT youth in child custody proceedings. Berkeley Journal of Gender, Law & Justice, 27, 171-197. Johnson, C. V., Mimiaga, M. J., & Bradford, J. (2008). Health care issues among lesbian, gay, bisexual, transgender and intersex (LGBTI) populations in the United States: Introduction. Journal of Homosexuality, 54(3), 213-224. Johnson, M. M., & Rhodes, R. (2010). Human behavior and the larger social environment, a new synthesis. United States: Allyn & Bacon, Inc. Kenagy, G. (2005). Transgender health: Findings from two needs assessment studies in Philadelphia. Health & Social Work, 30(1), 19. Lev, A. I. (2009). The ten tasks of the mental health provider: Recommendations for revision of the World Professional Association for Transgender Health's Standards of Care. International Journal of Transgenderism, 11(2), 74-99. Lombardi, E. (2001). Enhancing transgender healthcare. American Journal of Public Health, 91, 869-870. Lombardi, E. (2009). Varieties of transgender/transsexual lives and their relationship with transphobia. Journal of Homosexuality, 56, 977-992. 75 Nagoshi, J., & Brzuzy, S. (2010). Transgender theory: Embodying research and practice. Affilia, 25, 431. National Association of Social Workers (NASW). (2008). Code of ethics. Washington, DC: Author. Penn, D. (2001). San Francisco to expand transgender employee healthcare benefits. Lesbian News, 26(9), 16. Reis, E. (2004). Teaching transgender history, identity, and politics. Radical History Review, (88), 166-177. Rochman, S. (2007). What's up, Doc? Advocate, (997), 32-35. Roen, K. (2001). Transgender theory and embodiment: The risk of racial marginalisation. Journal of Gender Studies, 10, 253-263. doi:10.1080/09589230120086467 Sanchez, N. F., Sanchez, J. P., Danoff, A. (2009). Health care utilization, barriers to care, and hormone usage among male-to-female transgender persons in New York City. American Journal of Public Health, 99, 713-719. Sanger, T. (2008). Queer(y)ing gender and sexuality: Transpeople’s lived experiences and intimate partnerships. In L. Moon (Ed.), Feeling queer or queer feelings? Radical approaches to counseling sex, sexualities and genders. New York: Taylor and Francis. Sax, L. (2002). How common is intersex? A response to Anne Fausto-Sterling. Journal of Sex Research, 39, 174. 76 Schechter, L. (2009). The surgeon’s relationship with the physician prescribing hormones and the mental health professional: Review of version 7 of the World Professional Association for Transgender Health’s Standards of Care. International Journal of Transgenderism, 11, 222-225. Sennott, S. (2011). Gender disorder as gender oppression: A transfeminist approach to rethinking the pathologization of gender non-conformity. Women & Therapy, 34(1-2), 93-113. Sherriff, N. S., Hamilton, W. E., Wigmore, S., & Giambrone, B. B. (2011). 'What do you say to them?' Investigating and supporting the needs of lesbian, gay, bisexual, trans, and questioning (LGBTQ) young people. Journal of Community Psychology, 39, 939-955. doi:10.1002/jcop.20479 Shipherd, J. C., Magnun, S., Skidmore, C., & Abromovitz, S. (2011). Traumatology. 17(2), 56-67. Shipherd, J., Green, K., & Abramovitz, S. (2010). Transgender clients: Identifying and minimizing barriers to mental health treatment. Journal of Gay & Lesbian Mental Health, 14(2), 94-108. Some big companies now pay for transgender surgery. (2007). Contemporary Sexuality, 41(3), 15. Trans Rights Go Corporate. (2011). Advocate, (1053), 49. 77 van Kesteren, P. J., Gooren, L. J. & Megens, J. A. (1996). An epidemiological and demographic study of transsexuals in the Netherlands. Archives of Sexual Behavior, 25, 25. World Professional Association for Transgender Health (WPATH). (2011). Standards of care for the health of transsexual, transgender and gender nonconforming people. Version 7. United States: Author.