Document 16053190
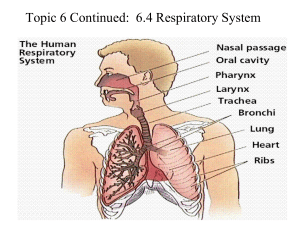
advertisement
Review Lung Volumes Tidal Volume (Vt) volume moved during either an inspiratory or expiratory phase of each breath (L) Inspiratory Reserve Volume (IRV) Reserve ability for inspiration (L) Volume of extra air that can be inhaled after a normal inhalation (L) Expiratory Reserve Volume (ERV) Volume of extra air that can be exhaled after a normal exhalation (L) Forced Vital Capacity (FVC or VC) Maximal volume of air that can be moved in one breath, from full inspiration to full expiration (L) SVC may be greater due to air trapping Residual Volume (RV) Volume of air remaining in lungs following a maximal exhalation (L) Usually increases with age Allows for uninterrupted exchange of gases Functional Residual Capacity (FRC) Volume of air in the lungs at the end of a normal tidal exhalation (end tidal) (L) Important for maintaining gas pressures in the alveoli Total Lung Capacity (TLC) Maximal amount of air in the lungs RV + VC = TLC (L) Maximal Ventilatory Volume (MVV or MBC) Maximal amount of air that can be moved in one minute (L/min) Pulmonary Ventilation @ rest, usually ~ 6 l/min Increase due to increases in rate and depth Rate: inc. 35-45 breaths/min, elite athletes: 60-70 breaths/min, max. ex. Vt 2 lit, Ve > 100 lit/min Vt may reach 2 lit, still 55-65% if VC (Tr and UNTr) Anatomic Dead Space Volume of air that is in conducting airways, not in alveoli, not involved in gas exchange Nose, mouth, trachea, other nondiffusible conducting portions of the respiratory tract Air is identical to ambient air, but warmed, fully saturated with water vapor 350 ml of 500 ml tidal volume will enter into and mix with existing alveolar air – 500 ml will enter alveoli, but only 350 ml is fresh air – 350 ml is about 1/7 of air in alveoli – This allows for maintenance of composition of alveolar air (concentration of gases) Dead space versus tidal volume Anatomic dead space increases with increases in tidal volume Increase in dead space is still less than increase in tidal volume Therefore, deeper breathing allows for more effective alveolar ventilation, rather than an increase in breathing rate Physiologic Dead Space Gas exchange between the alveoli and blood requires ventilation and perfusion matching: V/Q @ rest, 4.2 l of air for 5 l of blood each minute in alveoli, ratio ~.8 With light exercise, V/Q ratio is maintained Heavy exercise: disproportionate increase in alveolar ventilation When alveoli do not work adequately during gas exchange, it is due to – Under perfusion of blood – Inadequate ventilation relative to the size of the alveoli This portion of alveolar volume with poor V/Q ratio is physiologic dead space Small in healthy lung If physiologic dead space >60% of lung volume, adequate gas exchange is impossible Techniques of assessing lung volumes: Spirometry (cannot determine RV and FRC) Helium dilution Oxygen washout Plethysmograph (what we have) – based on Boyle’s Law: PV = P1V1 Alveolar Ventilation > 300 million alveoli elastic, thin-walled membranous sacs surface for gas exchange blood supply to alveolar tissue is greatest to any organ in body are connect to each other via small pores capillaries and alveoli are side by side at rest, 250 ml of O2 leave alveoli to blood, and 200 ml of CO2 diffuse into alveoli during heavy exercise, (TR athletes) 25X increase in quantity of O2 transfer Gas exchange in the lungs molecules of gas exert their own partial pressure total pressure = mixture of the sum of the partial pressures Partial pressure = % concentration X total pressure of the gas mixture Ambient Air @ sea level Oxygen: 20.93% X 760 mm Hg = 159 mm Hg Carbon Dioxide: 0.03% X 760 mm Hg = 0.2 mm Hg Nitrogen: 79.04% X 760 mm Hg = 600 mm Hg Partial pressure is noted by P in front, e.g., PO2 = 159 Tracheal Air as air enters respiratory tract, it is completely saturated with water vapor water vapor will dilute the inspired air mixture @ 37 degrees C, water exerts 47 mm Hg 760 - 47 = 713 Recalculate pressures, PO2 = 149 Alveolar Air different composition than tracheal air b/c of CO2 entering alveoli from blood and O2 leaving alveoli average PO2 in alveoli ~103 mm Hg PCO2 = 39 these are average pressures, it varies with the ventilatory cycle, and the ventilation of a portion of the lung FRC is present so that incoming breath has minimal influence on composition of alveolar air therefore, partial pressures in alveoli remains stable Gas Transfer in lungs PO2 is about 60 mm Hg higher in alveoli than capillaries b/c of diffusion gradient, oxygen will dissolve and diffuse through alveolar membrane into capillary CO2 pressure gradient is smaller, ~ 6 mm Hg adequate exchange still occurs b/c of high solubility of CO2 Nitrogen is not used nor produced, PN is relatively unchanged Equilibrium is rapid, ~ 1 sec, the midpoint of blood’s transit through the lungs during exercise, transit time decreases ~ 1/2 of that seen at rest during exercise, pulmonary capillaries can increase in blood volume 3X resting this maintains the pressures of oxygen and carbon dioxide Gas Transfer in the Tissues Partial pressures can be very different than those seen in the lung @ rest, PO2 in fluid outside a muscle cell are rarely less than 40 mm Hg PCO2 is about 46 mm Hg During exercise, PO2 may drop to 3 mm Hg, and PCO2 rise to 90 mm Hg O2 and CO2 diffuse into capillaries, carried to heart and lungs, where exchange occurs body does not try to completely eliminate CO2 blood leaves lungs with PO2 of 40 mm Hg, this is about 50 ml of carbon dioxide/100ml of blood PCO2 is critical for chemical input for control of breathing (respiratory center in brain) By adjusting alveolar ventilation to metabolic demands, the composition of alveolar gas will stay constant, even during strenuous exercise (which can increase VO2 and CO2 production by 25X)