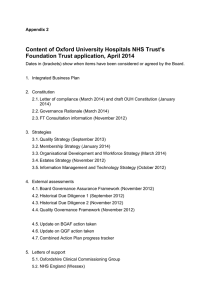
Current developments: A View from Social Care Terry Dafter
advertisement
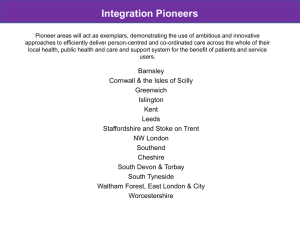
Current developments: A View from Social Care Terry Dafter Chair of ADASS Informatics Network November 2014 Background and Challenges • Ageing population – • Rising numbers of people with multiple long term conditions – – – • 70% of all health and care spending As of 2011 – 52% of over 65s had a limiting longterm health condition or disability – a rise of 50% in the decade since 2001 Over next 30 years number of people with dementia will double Public services under financial pressure – – • Over next 20 years, proportion of population 85+ will more than double Funding gap from rising demand set to be £30bn by 2021 (Nuffield/ NHS) LGA projecting a funding gap for local government of £16.5bn by 2020 (largely because of rise in social care costs) Pressures on services – – Over the 5 years to 2013, the number of over 80s attending A&E rose by 65% NAO suggest 20% of emergency admissions are for existing conditions that primary, community or social care could manage. Policy Drivers • • • • • Care Act – delivering the most significant change in the legal framework, funding and provision of adult social care for over 50 years Integration – Better Care Fund and Pioneers accelerating joint working and new models of care between primary, acute, community and social care Personalisation – increasingly putting the citizen at the heart of the system, in control of their health and their care and support (Web of Support) Quality – seeking continuous improvement in the quality and experience of health and care services, including greater transparency and use of data Prevention – exploring ways to reconfigure services to manage increasing demand better across health and care Current and Future State Current •Systems designed with the provider/ commissioner in mind, not end-user •Too many paper based processes in health and social care •Risk averse cultures around IG leads to little information shared between professionals or systems •Traditional market model, with small number of suppliers focusing on council back office systems •Use of apps under-developed at a time of innovation Future •User at the heart of the system, with the same level of customer service/ interaction as in other areas of life •ASC professionals and providers embracing technology as a key part of getting the job done •A fully joined up information ecosystem within health and care, including other critical agencies •Use of big data: effective prediction (through analytics) and prevention (preemptive interventions) •Dynamic market, open to innovation System Differences • • In Health the systems predominantly: – Support clinical governance and payment by results – Coding and standards based around clinical conditions and pathways. Social care systems – Support a person-centred customer journey and care management arrangements – Provide performance information and link to systems for billing and payment purposes. – Frequently operate complex interfaces to corporate systems. – Sometimes interface with third sector and private sector organisations. Our current infrastructure, processes and practices are a challenge Citizen focused health and care Data (e.g. NHS Number, standards, open APIs) Information Governance (e.g. aligned IG Toolkits) Network (e.g. PSN, N3) DH – Leading the nation’s health and care We need to clearly understand the levels of intervention required to ensure alignment: • What must happen nationally? • Where do we need collaboration and agreement across the whole system? • How can local innovation flourish? • How can we support cultural change? Delivery of core priority programmes Achieving broader strategic objectives Care Act implementation Integration & interoperability Pioneers Integration & interoperability Standards Information Governance Integration & interoperability – IDCR & Tech Fund Transparency & Comparative Data Infrastructure and systems Economic case Citizen-focussed technology Current state Market development Target future state Capability & leadership National work programme focused on two broad areas 1) delivery of key programmes, and 2) how to start to develop a wider consensus around investment and change Being in Newcastle: Wider Issues around Federation • 3 Elements of functionality – Portal functions: publish search and find items across the systems – Switch functions: orchestrate processes and perform transactions – Index functions: name and identify things and register relationships • Systems now exist that will support – Federated identity – Relationship management – Document sharing • Challenge therefore is to federate in a local system and then beyond • Not an issue of technology more one of trust and leadership Wider moves to build around the user? • National move towards access to GP record • Social care has a model of ‘web of support’ • Care accounts are coming with respect to the Care Bill • Giving the person more involvement helps with data ownership and sharing • Raises issues around capacity and informed consent • Can the technology support this • What about issues of identity and authentication In Summary • • • Feels like we are building a moving train Not so much what is unplanned but rather what is planned that is problematic Need to understand it’s not just health and social care organisations – User and Independent Sector • Important that the various national programmes are synchronised and consistent – Better Care Fund – Tech Fund – Pioneers • • • • Technology is there The will is there Need for local and national leadership if we are going to deliver Best chance we have to do something in a generation