Alphabet Soup A Primary Care Physician’s Guide to Idiopathic Interstitial Pneumonitis
advertisement

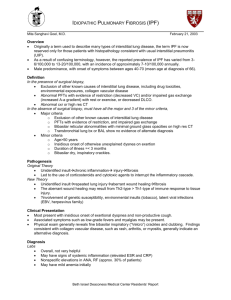
Alphabet Soup A Primary Care Physician’s Guide to Idiopathic Interstitial Pneumonitis Matt Mundy MS3 Idiopathic Interstitial Pneumonitis : The Dilemma Identification of this class of diseases is notoriously difficult. Uncertain etiologies, discrepancies in the descriptions of the clinical, radiographic and pathologic characteristics of the disease processes and the necessity for multidisciplinary communication and cooperation in the clinical investigation all add to the challenge of making an accurate diagnosis. Combined with a seemingly endless string of acronyms used to refer to specific disease subtypes, these factors can make Idiopathic Interstitial Pneumonitis a seemingly insurmountable challenge to clinicians. So……… 1. For a Primary Care Physician, what are the most important questions to ask about Idiopathic Interstitial Pneumonitis? 2. What are the major subtypes of Idiopathic Interstitial Pneumonitis? 3. What are the important Clinical, Pathologic, and Radiographic findings in each of these subtypes? 4. What therapies are available when a diagnosis is ultimately made? What are the most important questions to ask? •By understanding the acronyms and answering just a few questions, a primary care doctor can have good insight into a patients’ disease and its prognosis. This understanding can then be used to guide future therapy and clinical decision making. Welcome to IIP 101 An quick and easy guide to the basics of Idiopathic Interstitial Pneumonitis A, B, C, D, E, F, G……….. Question #1 What do all the acronyms mean? Clinical Diagnosis Pathologic Diagnosis Idiopathic Pulmonary Fibrosis (IPF)……………………..……..Usual Interstitial Pneumonia (UIP) Desquamative Interstitial Pneumonia (DIP)……………….……………………………….…….….same (DIP) Respiratory Bronchiolitis Interstial Lung Disease (RBILD)…….…………….same (RBILD) Acute Interstitial Pneumonia (AIP)…………………………..…Diffuse Alveolar Damage (DAD) Nonspecific Interstitial Pneumonia (NSIP)………………………………………………………same (NSIP) *adapted from: The American Thoracic Society / European Respiratory Society International Multidisciplinary Consensus Classification 2002 Important clarifications about the acronyms 1. Each pathologic diagnoses has a distinct pattern 2. Each of the pathologic patterns has unique and consistent radiographic findings 3. The pathologic and radiographic patterns can have multiple etiologies 4. A clinical diagnosis of a corresponding Idiopathic Interstitial Pneumonitis can only be made when no cause for the pathology can be identified ILD Vs. DLD: What, more acronyms? •Interstitial Lung Disease (ILD), a term used by pathologists refers to the same set of diseases that radiologists call Diffuse Lung disease(DLD). •There are over 150 identified processes that fall under this description •All of them can lead to lung scarring and respiratory failure •Examples include: occupational, exposure related and drug induced diseases, eosinophilic pneumonias, sarcoidosis, collagen vascular related ILD, granulomatous disease and finally Idiopathic Interstitial Pneumonitis So……… IIP is a subset of ILD And……….. IPF, DIP, RB-ILD, AIP and NSIP Are all subtypes of IIP See. It’s not so scary after all. Question #2 What is the most important distinction to make? UIP Vs. Everything Else Why? Complete recovery is possible with all types of Idiopathic Interstitial Pneumonitis Except UIP/IPF!!! • Because of its poor prognosis and refractoriness to treatment, it is essential to identify cases of usual interstitial pneumonia / idiopathic pulmonary fibrosis • Things to remember: 1. Immunosuppression or smoking cessation will improve survival all types of IIP EXCEPT UIP/IPF 2. The median survival after diagnosis for UIP/IPF is 2.5-3.5 years 3. No therapy has been shown to reduce the severity of pathologic findings or improve the prognosis of UIP/IPF The diagnosis of UIP/IPF does not require pathologic confirmation •With a high clinical suspicion, the characteristic radiographic findings of UIP are specific enough to be sufficient for diagnosis •Studies show that combining clinical history, including pulmonary function tests, and CT findings alleviates the need for biopsy in up to 89% of patients •When conflicting or inconclusive findings arise, a biopsy specimen can solidify the diagnosis Again……. The diagnosis of UIP/IPF implies many things, including: 1. There is probably no need for a biopsy 2. Treatment of any sort is likely to have little, if any effect 3. MOST IMPORTANTLY: UIP/IPF implies a very poor prognosis for the patient no matter what their age, gender or extent of disease Question #3 What is “ground glass” anyway? *many of the radiographic patterns of IIP involve ground glass opacities, therefore, the ability to identify ground glass on a CXR and CT is essential Ground Glass Opacity: “focal or diffuse areas of ill-defined, hazy, increased lung attenuation, which cause pulmonary vascular indistinctness, yet through which vessels can still be identified.”* *Nowers et al Ground Glass Opacity: The ground glass pattern can be identified on both CT and conventional radiographs Ground Glass Opacity: Ground glass falls on a spectrum of increasing opacification that culminates in consolidation consolidation Ground glass What are the major subtypes of IIP? and What are the most pertinent clinical, radiographic and pathologic findings? *remember that IIP is a multidisciplinary diagnosis Important subtypes of IIP 1. UIP/IPF (usual interstitial pneumonia/idiopathic pulmonary fibrosis) 2. NSIP (nonspecific interstitial pneumonia) 3. AIP/DAD (acute interstitial pneumonia/diffuse alveolar damage) 4. RB-ILD (respiratory bronchiolitis interstitial lung disease) 5. DIP (desquamative interstitial pneumonia) *RB-ILD and DIP are strongly associated with smoking and respond well to smoking cessation. Therefore, arguments have been made against classifying them as idiopathic. UIP IPF UIP / IPF (Usual Interstitial Pneumonia/Idiopathic Pulmonary Fibrosis) Clinical Presentation -History •age: usually greater than 50 •male to female ratio: between 1:1 and 2:1 •75% have a smoking history •insidious exertional dyspnea which is disabling over time •nonproductive cough - refractory to antitussive medication •fever, malaise and arthralgia reported in 50% UIP / IPF (Usual Interstitial Pneumonia/Idiopathic Pulmonary Fibrosis) Clinical Presentation - Physical Exam •tachypnea •bibasilar inspiratory crackles •75% have digital clubbing •PFTs show restrictive physiology ( VC and TLC, FEV1 to FVC ratio) •reduced diffusion capacity (DL ) CO •symptoms usually start >6 months before clinical presentation UIP / IPF (Usual Interstitial Pneumonia/Idiopathic Pulmonary Fibrosis) Digital Clubbing UIP / IPF (Usual Interstitial Pneumonia/Idiopathic Pulmonary Fibrosis) Differential Diagnosis (etiologies that can cause a UIP pattern) •asbestosis •collagen vascular disease induced interstitial lung disease •drug toxicity •chronic extrinsic allergic alveolitis UIP / IPF (Usual Interstitial Pneumonia/Idiopathic Pulmonary Fibrosis) Radiographic Findings – Chest Radiograph •Peripheral, lace-like areas of fine reticular opacity •Concentrated posteriorly in the bases •Visible fibrosis in costophrenic recesses on lateral CXR •Ground glass opacification of lower lobes UIP/IPF Peripheral reticular opacity more predominant in the bases UIP / IPF (Usual Interstitial Pneumonia/Idiopathic Pulmonary Fibrosis) Radiographic Findings – CT •Similar to CXR •Fibrosis •Traction bronchiectasis •Architectural distortion •+- honeycombing •Variable ground glass opacity •Concentrated in lower lobes UIP/IPF Peripheral ground glass No evidence of honeycombing Area of consolidation UIP/IPF Peripheral traction bronchiectasis and honeycombing More predominant in lung base UIP/IPF Bilateral peripheral honeycomb cysts UIP/IPF marked honeycombing – end stage disease UIP / IPF (Usual Interstitial Pneumonia/Idiopathic Pulmonary Fibrosis) If the clinical and radiographic findings are consistent and suggest UIP/IPF a diagnosis can be made without a biopsy. Pathologic evidence is only necessary in cases where the diagnosis is uncertain *all other forms of IIP require pathologic confirmation for diagnosis UIP / IPF (Usual Interstitial Pneumonia/Idiopathic Pulmonary Fibrosis) Pathologic Findings •Video Assisted Thoroscopic Biopsy (VATS) required because of the peripheral distribution of disease •Patchy, dense subpleural collagenous fibrosis +/Honeycombing •Fibroblastic foci of acute injury •Very little inflammation •Areas of interspersed normal lung •The hallmark is spatial and temporal heterogeneity of disease UIP/IPF – gross specimen Small, firm, fibrosed lung seen in advanced disease UIP/IPF – gross specimen White tissue represents interstitial fibrosis UIP/IPF – histologic section Spatial heterogeneity: fibrosis with interspersed normal lung UIP/IPF – histologic section Area of acute lung injury: fibroblastic foci UIP/IPF – histologic section Honeycombing: the final stage of UIP/IPF UIP / IPF (Usual Interstitial Pneumonia/Idiopathic Pulmonary Fibrosis) Treatment and Prognosis •no response to steroids or other immunosuppressive drugs •smoking cessation does not change course of disease •course marked by periods of rapid clinical deterioration •5 year survival rate: 10%-50% •median survival after diagnosis: 2.5-3.5 years •prognosis worse in men NSIP NSIP Nonspecific Interstitial Pneumonia Clinical Presentation - History and Physical •less chronic than UIP with a duration of months to years •age: 39-50 years •male to female ratio: 2:1 •68% with smoking history •dyspnea, cough and occasional fever •tachypnea, crackles, no digital clubbing •PFT’s: restrictive NSIP Nonspecific Interstitial Pneumonia Differential Diagnosis (etiologies that can cause an NSIP pattern) •collagen vascular disease induced interstitial lung disease •extrinsic allergic alveolitis •resolving acute lung injury •drug induced pneumonitis •infection (HIV) NSIP Nonspecific Interstitial Pneumonia •NSIP is further divided into subtypes •Cellular NSIP is the less severe form that occurs in younger people •Fibrotic NSIP shares many of the features of UIP and has a worse prognosis than the cellular subtype •These distinctions become important for both the radiographic and pathologic investigation of the disease •Although distinctions have been made, it is clear that the two subtypes lie on a continuum and overlap does exist NSIP Nonspecific Interstitial Pneumonia Radiographic Findings – cellular subtype •Relative predominance of ground glass opacity with fewer areas of fibrosis •Can be distributed diffusely or in a basilar predominant pattern •Peribronchovascular thickening and areas of consolidation •Occasional traction bronchiectasis secondary to chronic inflammation NSIP Nonspecific Interstitial Pneumonia Radiographic Findings – fibrotic subtype •Relative predominance of fibrosis with areas of ground glass opacity •Reticular opacities and traction bronchiectasis can be seen •Severe form can be indistinguishable from UIP •Decreased occurrence and severity of honeycombing in the face of severe fibrosis suggests NSIP NSIP Reticular opacity Ground glass Bilateral basal ground glass and reticular opacities with peripheral distribution NSIP Ground glass Reticular opacity Traction bronchiectasis NSIP Nonspecific Interstitial Pneumonia Pathologic Findings •Diffuse pattern of inflammation •Relatively more fibrosis in fibrotic subtype •Underlying parenchyma is intact •Fibrosis, when present, is temporally homogenous •Mature hypocellular collagen •Little or no honeycombing •Inflammation predominantly lymphocytes NSIP Widened alveolar walls (arrows) with increased numbers of lymphocytes adjacent to an area of normal lung NSIP Pattern of mixed inflammation and fibrosis inflammation Fibrosis *note the absence of honeycombing NSIP Nonspecific Interstitial Pneumonia Treatment and Prognosis •the two subtypes are treated the same but their outcomes are very different •glucocorticoids are the mainstay of therapy •prognosis highly dependent on amount of fibrosis present •cellular: 5 year survival - 100%, 10 year survival - 100% •fibrotic: 5 year survival - 90%, 10 year survival - 35% AIP DAD AIP/DAD Acute interstitial Pneumonia/Diffuse Alveolar Damage Clinical Presentation - History and Physical •Acute onset of respiratory distress •Mainly affects current smokers •Usually presents in 4th or 5th decade – mean age is 49 •Male to female ratio: 2:1 •Cough and dyspnea lasting weeks to months •50% have fever •50% have digital clubbing AIP/DAD Acute interstitial Pneumonia/Diffuse Alveolar Damage Differential Diagnosis – (etiologies that can cause DAD pattern) •ARDS •Shock •Sepsis •Radiation •Chemotherapy •Toxic inhalants •Viruses AIP/DAD Acute interstitial Pneumonia/Diffuse Alveolar Damage Radiographic Findings •Initial patchy ground glass opacity •Evolves into more confluent ground glass •Scattered areas of consolidation •Traction bronchiectasis and architectural distortion may be seen on CT AIP/DAD Diffuse symmetric ground glass opacities with slightly peripheral predominance AIP/DAD Bilateral ground glass AIP/DAD Bilateral ground glass opacity Air bronchogram AIP/DAD Acute interstitial Pneumonia/Diffuse Alveolar Damage Pathologic Findings •Divided into acute, organizing and fibrotic stages •Acute stage: (peak at 4 days) interstitial and air space edema, hyaline membranes, hemorrhage, fibrinous exudate •Organizing stage: (peak at 2-3 weeks) proliferation of fibroblasts, loose granulation tissue involving septa, thickened vessels •Fibrotic stage: (after 3-4 weeks) extensive, dense fibrotic remodeling, possible honeycombing AIP/DAD Organizing stage : Interstitial thickening with collapsed alveolar septa Alveolar Ducts AIP/DAD Acute Stage : fibrinous exudate Hyaline membranes AIP/DAD Acute interstitial Pneumonia/Diffuse Alveolar Damage Treatment and Prognosis •Supportive care is mainstay of treatment – mechanical ventilation is often required •Steroids and antibiotics have shown little benefit •>60% mortality •Most deaths occur within the first 6 months •People who survive usually do not have recurrence of disease RB-ILD RB-ILD Respiratory Bronchiolitis Associated Interstitial Lung Disease Clinical Presentation – history and physical •Usually asymptomatic •May have cough or mild dyspnea •Age: usually 4th or 5th decade •Male to female ratio: 1:1 •History of heavy smoking •Bibasilar end inspiratory crepitations •Coarse rales RB-ILD Respiratory Bronchiolitis Associated Interstitial Lung Disease Radiographic findings •Ill-defined ground glass centrilobular nodules •Confluent patchy areas of ground glass may also be seen •mid to upper lung zone predominant •Fibrosis not seen on CXR or CT •Progressive decrease in lung volumes •CXR is often normal RB-ILD Diffuse centrilobular opacities predominantly in lower lung zones RB-ILD Diffuse centrilobular ground glass opacities RB-ILD Respiratory Bronchiolitis Associated Interstitial Lung Disease Pathologic Findings •VATS required for diagnosis because disease is centered around terminal bronchioles •Mild interstitial mononuclear infiltrates of terminal bronchioles that extend into adjacent alveolar septa •Mild interstitial thickening •Little or no fibrosis RB-ILD •Alveolar macrophages in lumen of respiratory bronchiole •mildly thickened bronchiolar wall RB-ILD Respiratory Bronchiolitis Associated Interstitial Lung Disease Treatment and Prognosis •Smoking cessation is mainstay of therapy •Favorable but variable response to corticosteroids •100% 10 year survival DIP DIP Desquamative Interstitial Pneumonia Clinical Presentation – history and physical •>90% are smokers •Age: 4th or 5th decade •Subacute cough and dyspnea lasting weeks to months •Male to female ratio: 2:1 •Restrictive PFT’s, Decreased DLCO, hypoxemia •50% with digital clubbing DIP Desquamative Interstitial Pneumonia Differential Diagnosis (etiologies that result in DIP pattern) •Subacute extrinsic allergic alveolitis •PCP •Sarcoid •Drug toxicity •Asbestosis •Eosinophilic granulomatosis •UIP, NSIP DIP Desquamative Interstitial Pneumonia Radiographic findings •Diffuse ground glass opacities •Similar to RB-ILD, but confluent patchy areas of ground glass predominate •More likely affects basilar and sub-pleural areas •Fibrosis rarely seen on CXR or CT •Progressive decrease in lung volumes DIP Diffuse Gound Glass Opacities on CXR and CT DIP Diffuse Gound Glass Opacities on CXR and CT DIP Desquamative Interstitial Pneumonia Pathologic findings •Diffuse intraalveolar pigmented macrophage accumulation •Mild interstitial thickening •Inflammation superimposed on normal lung architecture •Fibrosis of septa •Occasional honeycombing •Hyperplasia of Type 2 pneumocytes •Temporal Homogeneity DIP Macrophage accumulation with mild interstitial thickening DIP Diffuse intraalveolar macrophage accumulation A quick recap…….. 1. IIPs are a spectrum of interstitial lung diseases for which no clear etiology can be determined 2. The primary responsibility, when confronted with a patient with IIP is to differentiate whether they have a case of UIP/IPF or a case of something else 3. Although different types of IIP can present similarly in the clinic, radiographic and pathologic findings can clarify the diagnosis - A multidisciplinary approach is essential 4. Whether it be smoking cessation, or corticosteroid therapy, all types of IIP can be effectively treated and even cured, except UIP/IPF Most Importantly………… Remember that behind the radiographs, chest CTs and histological sections, somewhere lost in the sea of acronyms is a person with a disease. Therefore, making an accurate diagnosis is essential, as it will dramatically influence the way your patient approaches the future. References 1. Myers J. Pathologic Classification of Idiopathic Interstitial Pneumonias. Up To Date, 2004. 2. Nowers K. Rasband JD. Berges G. Gosselin M. Approach to Ground Glass Opacification of the Lung. Seminars in Ultrasound, CT and MRI. 23(4): 302-323, August 2002. 3. Pandit-Bhalla M. Diethelm L. Ovella T. Sloop GD. Valentine VG. Idiopathic interstitial pneumonias: an update. Journal of Thoracic Imaging. 18(1):1-13, Jan uary 2003. 4. Reynolds JH. Hansell DM. The interstitial pneumonias: understanding the acronyms. Clinical Radiology. 55(4):249-60, April 2000. 5. Sholand MB. Clinical Approach to Interstitial Lung Disease. Seminars in Ultrasound, CT and MRI. 23(4): 269-274, August 2002. 6. Szakacs JG. Pathologist’s Approach to Diffuse Lung Disease. Seminars in Ultrasound, CT and MRI. 23(4): 275-287, August 2002.