Meconium Aspiration Syndrome Edited May 2005

Meconium Aspiration Syndrome
Edited May 2005
Pulmonary Vascular Resistance
Ventilation
Remove
Placenta
Pulmonary Venous Return
LA Pressure
PO
2
Foramen Ovale
Closes
RA Pressure
IVC Return
Umbilical Venous Return
L --> R ductus arteriosus shunt
Systemic Vascular Resistance
Ductus
Venosus
Closes
What is meconium aspiration?
Meconium is the first intestinal discharge of the newborn
Epithelial cells, fetal hair, mucus, bile
Intrauterine stress may cause in utero passage of meconium
Aspirated by the fetus when fetal gasping or deep breathing occurs stimulated by hypoxia and hypercarbia
Warning sign of fetal distress
Meconium: The Stats
Frequency of Mec stained amniotic fluid = 10-25%
OF MEC stained infants:
30 % depressed at birth
10 % meconium aspiration syndrome (range 2-36 %)
OF infants with MEC aspiration syndrome
17 % deliver through thin meconium (range 7-35 %)
35 % need mechanical ventilation (range 25-60 %)
12 % die (range 5-37 %)
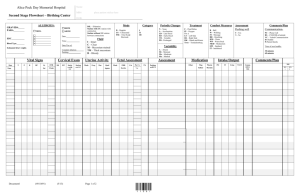
OHSU Experience: Inborn + Transfers
# Mec passed
1992-94 146
1995-97 154
DR intub
MAS MAS
+ vent
88 44
92 39
28
25
ECMO Died
4
1
3*
1*
Total 300 180 83 53 5 4
MAS = Meconium aspiration syndrome as primary pulmonary diagnosis
No pulmonary hypoplasia or major congenital anomalies
MAS+ vent = ventilated with pulmonary diagnosis of MAS or PPHN
ECMO = MAS infants transferred for ECMO
Died : * 1 infant in each of the years died with a diagnosis of severe HIE
Risk Factors for Meconium Passage
Postterm pregnancy
Preeclampsia-eclampsia
Maternal hypertension
Maternal diabetes mellitus
Abnormal fetal heart rate
IUGR
Abnormal biophysical profile
Oligohydramnios
Maternal heavy smoking
Meconium in Amniotic Fluid
Intrapartum suctioning of mouth, nose, pharynx
Infant Depressed
Infant Active
Observe
Intubate and suction trachea
Other resuscitation as indicated
Meconium Aspiration Syndrome
Pathophysiology
Airway obstruction of large and small airways
Inflammation and edema
Protein leak
Inflammatory Mediators
Direct toxicity of meconium constituents = chemical pneumonitis
Surfactant dysfunction or inactivation
Effects of in utero hypoxemia and acidosis
Altered pulmonary vasoreactivity (PPHN)
Meconium Aspiration Syndrome
Diagnosis
Known exposure to meconium stained amniotic fluid
Respiratory symptoms not explained by other cause
R/O pneumonia, RDS, spontaneous air leak
CXR changes - diffuse, patchy infiltrates, consolidation, atelectasis, air leaks, hyperinflation
Meconium Aspiration Syndrome
Treatment
Ventilation strategies
Avoid air leak, check CXR with acute deterioration
Prevent pulmonary hypertension - generous O2
HFOV if unable to maintain on conventional vent
Steroids (no human data, controversial)
ROS, Antibiotics (ampicillin, gentamicin)
Surfactant
Inhaled Nitric Oxide
ECMO
Other Things to Watch For
Hypoxia
Acidosis
Hypoglycemia
Hypocalcemia
End-organ damage due to perinatal asphyxia
Meconium Aspiration Syndrome
Outcome
High incidence long term pulmonary problems
At 6 months - 23% MAS with regular bronchodilator therapy*
FRC was higher in symptomatic infants
IPPV and O2 were not predictors of problems
Increased risk of poor neurologic outcome due to perinatal insult - seizures, CP, mental retardation
*Yuksel et al. Pediatric Pulmonology 16:358, 1993
Meconium Aspiration Syndrome
Surfactant Treatment
Methods
< 6 hours old with MAS
20 infants randomized to receive 150 mg/kg surfactant by 20 minute infusion, q6h x4 doses maximum
On ventilator - FiO
2
> 50%, MAP > 7, a:A PO
2
< 0.22
Endpoint = improvement in OI and a:A PO
2
No difference in groups
Findlay et al. Pediatrics 97 (1): 48, 1996.
Meconium Aspiration Syndrome
Surfactant Treatment
Results
No infant received more than 3 doses
Significant improvement in OI, MAP, FiO
2 within 3-6 hours after 2 nd dose of surfactant
Significant improvement in a:A PO
2 within 1 hour of 1 st dose of surfactant
Findlay et al. Pediatrics 97 (1): 48, 1996.
Meconium Aspiration Syndrome
Surfactant Treatment
Air leak
ECMO
Days MV
Days O
2
LOS (days)
D/C on O
2
Mortality (< 28 d)
Control Surf P value
5 0 0.024
6 1 0.037
11 (1) 8 (1) 0.047
20 (3) 13 (1) 0.031
24 (2) 16 (1) 0.003
8 6 NS
0 0 NS
Findlay et al. Pediatrics 97 (1): 48, 1996.