Breastfeeding Success Kirsten E. Crowley, MD Edited May, 2005
Breastfeeding
Success
Kirsten E. Crowley, MD
Edited May, 2005
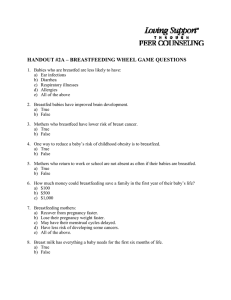
The big push
American Academy of Pediatrics
“Exclusive breastfeeding is ideal nutrition and sufficient to support optimal growth and development for approximately the first 6 months after birth.”
WHO and UNICEF
Infants should be breastfed for at least the first four months of life, and if possible 6 months
Healthy People 2010 Objective
Increase the number of mothers breastfeeding postpartum to 75%, at 6 months to 50%, and at 1 year to 25%
Benefits to the Baby
Protects against
Infection
Illness
allergies
Provides species-specific nutrition and hormones
May enhance development and intelligence
Confers long term benefits
Protection against infection
The studies
In first year of life, incidence of diarrheal illness among breastfed infants was half that of formula-fed infants
Infants who were exclusively formula-fed had a 70% increase in their risk of developing an ear infection
Formula-fed infants were 17 times more likely to be admitted for pneumonia
More infection studies
Associated with a lower incidence of RSV infection during the first year of life
Relative risk of developing a UTI of 0.38 compared to formula-fed infants
In the NICU
Among babies born at more than 30 weeks, confirmed NEC was 20 times more common in formula-fed babies
The incidence of sepsis/meningitis are significantly reduced in human milk fed VLBW infants
Other illness
There is an inverse relationship between breastfeeding and morbidity
Breastfed infants have gastroesophageal reflux episodes of significantly shorter duration
Breastfeeding is protective against SIDS
Toddlers who were breastfed appear to be healthier
Protection against allergies
In allergic families, formula introduction in the first week of life and weaning at less than 4 months were associated with increased allergies later in life
Eczema was less common and milder
Breastmilk = 22%
Soymilk formula = 63%
cow’s milk formula = 70%
Enhances development and intelligence
Controversial of course
Some studies have shown higher IQ and improved cognitive development in breastfed children
Psychomotor and social development may be improved as well
Long term benefits
Lower incidence of
diabetes
childhood cancer and breast cancer
May influence LDL concentration and mortality from ischemic heart disease
Decreased cavities
Better response to vaccines
Benefits to mom
Delays fertility due to lactational amenorrhea
Reduces risk of breast, uterine, ovarian, and endometrial cancer
Enhances emotional health
Decreases insulin requirements
Decreases osteoporosis
Promotes postpartum weight loss
Societal benefits
Encourages optimum child spacing
Improves vaccine effectiveness
Decreased expense of food (formula for one year is between $1160 and $3915)
Decreased medical expenses
1000 bottle-fed infants had 2033 excess office visits,
212 excess days in the hospital, and 609 more prescriptions = $459-$808 per family per year
Reduced absenteeism due to child illness
Protects the environment (bottles, packages, etc.)
So, how are we doing?
In 1998
64% of women initiated breastfeeding
29% were still breastfeeding at 6 months
16% were breastfeeding at one year
highest rates in several generations
Rates still fall short of the Healthy People goals of 75% initiation, 50% at 6 months, and 25% at one year
U.S. breastfeeding rates are the second lowest of all industrialized nations
Who tends to breastfeed?
Most common among women who are
college educated
white
married
older than 30 years
middle or higher income levels
More prevalent in the western regions of the country
What affects success?
Maternity hospital routines
accuracy and timeliness of breastfeeding assistance are the most important
Birth weight and health of the newborn
Peer attitudes
Length of maternity leave
Employer’s willingness to make accommodations
Opinion of the child’s father
Aggressive marketing of formula
Promoting success
Women who are better informed regarding the benefits of breastfeeding and the breastfeeding process are more likely to initiate (and probably maintain) breastfeeding
An interesting study
Kistin et al.
First controlled trial of prenatal maternal counseling by MDs
Counseling increased the rate of initiation and duration of breastfeeding in a predominantly low-income, urban, African
American population
National Assessment of
Physicians’ Breast-feeding
Knowledge, Attitudes,
Training, and Experience
Freed, et al. JAMA.. 1995; 273(6): 472-476
Residents and practitioners in peds, FP, and OB/gyn were lacking in
Breastfeeding knowledge base
Ability to give appropriate advice
The role of the pediatrician
Promote and support
Become knowledgeable and skilled in physiology and clinical management
Provide education
Parents, Colleagues, Nurses, Residents
Become familiar with local resources
Develop and promote policy
Encourage insurance coverage
Promote breastfeeding friendly workplaces
Assessing for success
The input (milk transfer)
The output (urine & stool)
The ultimate (weight)
The intake
Goal is 8-12 feedings per day
Feedings should last 10-15 minutes when the baby is a newborn
Understand the cues
Sleep arousal
Increased alertness
Hand to mouth
Tongue or mouth movements
Crying (late stage of hunger)
The output
Urine
Before the milk is in: one void for each day of age
After the milk arrives: 6-8 times per day
Stool
Days 1-4: meconium
Day 4-4 weeks: 4 yellow, seedy BM per day
1-4 months: varies from one per feed to once a week
The ultimate judge:
The Weight
Initial loss
8-10% of birthweight
Return to birthweight
10-14 days
Aggressive intervention if not by 2 weeks
Rate of gain for full term babies
First 2 months = 30 grams per day
> 2 months = 20-30 grams per day
Assess the Latch!
Incorrect latch is one of the most common etiologies for poor weight gain
Observation of the mother - infant dyad is extremely important!
Correct latch
Mother
Mom holds breast back from areola and nipple with
C-hold
Use manual stimulation to erect the nipple
Tickle the baby’s lips gently
Wait for baby to open mouth like a yawn
Center nipple quickly while pulling baby in close to the breast
Initial latch may be painful, but abates as nursing progresses
Correct latch
Baby
Tip of nose and chin touching breast
Tummy to tummy
Lips flanged over areola - fish lips
Gums bypass nipple and are over areola
(where the milk sinuses are)
Movement of facial and jaw muscles, ear wiggling
Look for suck-swallow patterns
Assessment of suck
Tongue comes over the gumline
Cupping of tongue at the lip
Feel up and down motion of the posterior tongue
Strength of suck
Nursing positions
Cradle hold
Mom upright in comfortable chair with pillows in the lap and feet supported
Tummy to tummy
Head in straight line
Ear, shoulder, and hips in straight line
Baby’s body at breast level (boppy pillow)
Baby’s head in crook of elbow
Baby’s back supported with forearm
Cup breast with free hand
Cradle hold
Boppy pillow
Nursing positions
Football hold
Mom in same position
Baby’s body and legs under mom’s arm
Head snugly in mom’s hand with neck grasped by thumb and pinky and head on palm and other fingers
Pillows under the baby (boppy)
Avoid flexing baby’s head too much
Football hold
Nursing positions:
Lying Down
Helpful after a cesarean section
Good for tired moms
Eases nighttime feedings early on if the dyad is cosleeping
Common problems
(and how to fix them)
Sore nipples
Discomfort at the beginning is OK
Improper position is the main cause
Can also be caused by infection or inappropriate nipple care
Treatment
Position correctly
Begin feeding on least sore nipple
Frequent shorter feeds
Rub expressed milk onto nipple/areola
Air dry nipples
Pump if nipples are too painful
Engorgement
Occurs on the second to fourth days
Results from hormone changes that suddenly increase milk production
Temporary!!!: The supply becomes balanced within a few days
Treatment
Nurse frequently, around the clock
Heat and massage before feeding
Express some milk if baby can’t latch
May be harmful to supply if not relieved
Mastitis
Bacterial breast infection
caused by inadequate emptying of milk
Symptoms
achy, flu-like
breast pain, redness, tenderness fever/chills
Treatment
Dicloxicillin 250 mg QID x 10 days
Keflex 500 mg QID x 10 days
Rest, fluids, pain meds, nurse often or pump after feeds, moist heat
Candidiasis
Rapid development of extremely sore nipples, burning or itching, shooting pain
Look for deep pink areas on mom and thrush or diaper candidiasis in baby
Treat both mom and baby
Topical antifungal for both, oral nystatin
Wash anything in contact with baby’s mouth or breast
Breastfeeding jaundice
Exaggerated physiologic jaundice due to lack of food in GI tract and increased enterohepatic circulation
Usually occurs in second to third day
Treatment
Increase feeding frequency
Mom should pump if baby is sleepy or poor feeder
Feed baby EMM or formula only
Use alternate feeding systems if necessary
Watch baby’s weight