Pituitary Adenomas Chien Wei OMS IV September 14, 2006
advertisement

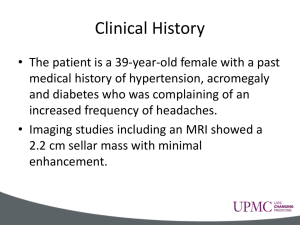
Pituitary Adenomas Chien Wei OMS IV September 14, 2006 Overview Background Clinical Presentation Classification Is it beneficial to give RT after transsphenoidal resection How much time post-RT should pt. be followed? Is there benefit to GKS? General Management Complications Anatomy 60 mg midline structure in sella turcica Bordered by diaphragma sellae, tuberculum sellae, dorsum sellae, lateral sinuses, and sphenoid sinuses Anterior and posterior lobes Function Anterior Lobe: FSH LH ACTH TSH Prolactin GH Posterior Lobe: ADH Oxytocin Epidemiology Etiology is unknown Not associated with environmental factors 10-15% of all primary brain tumors 20-25% of pituitary glands at autopsy found to have adenomas 70% of adenomas are endocrinogically secreting 25% of those with MEN-I develop pituitary adenomas Natural History Pituitary adenomas have long natural history Vary in size and direction of spread Microadenomas < 10 mm – may cause focal bulging Macroadenomas > 10 mm – cause problems due to mass effect Clinical Presentation Most common are endocrine abnormalities – hyper-/hyposecretion of ant. pituitary hormones HA Vision changes – bitemporal hemianopsia and superior temporal defects Endocrine-Active Pituitary Adenomas Prolactin – Amenorrhea, galactorrhea, impotence Growth hormone – Gigantism and acromegaly Corticotropin – Cushing’s disease, Nelson’s syndrome post adrenalectomy TSH - Hyperthyroidism Non-functioning Adenomas 25-30 % of patients do not have classical hypersecretory syndromes May grow to a large size before they are detected Present due to mass effect Visual deficits HA Hormone deficiency Evaluation MRI Visual field assessment Endocrine evaluation Tests of normal gonadal, thyroid, and adrenal function Radioimmunoassays – for hormone levels Classifying Imaging/surgical classification Clinical/endocrine – functional vs. nonfunctional Pathological classification WHO classification – reconciles the three systems above Classification Microadenomas – Grades 0 and I Macroadenomas – Grades II to IV Grade 0: Intrapituitary microadenoma with normal sellar appearance Grade I: Nml-sized sella with asymmetric floor Grade II: Enlarged sella with an intact floor Grade III: Localized erosion of sellar floor Grade IV: Diffuse destruction of floor Classification Type A: Tumor bulges into the chiasmatic cistern Type B: Tumor reaches the floor of the 3rd ventricle Type C: Tumor is more voluminous with extension into the 3rd ventricle up to the foramen of Monro Type D: Tumor extends into temporal or frontal fossa Pathologic Classification Benign or malignant Chromophobic – Non-functioning Basophilic – Cushing’s Acidophilic - Acromegaly Mixed WHO Classification Five-tiered system Clinical presentation and secretory activity Size and invasiveness (e.g. Hardy) Histology (typical vs. atypical) Immunohistologic profile Ultrasturctural subtype The long-term efficacy of conservative surgery and radiotherapy in the control of pituitary adenomas Retrospective study of 411 patients treated with EBRT for pituitary adenomas Goal is to assess both long-term efficacy and toxicity of conservative surgery and RT in the management of pituitary adenomas M. Brada et al, Clinical Endocrinology (1993) 38, 571-578 Method 252 of 411 pts with non-functioning pituitary adenomas 131 of 411 pts had functional pituitary adenomas (62 acromegaly, 60 prolactinomas, 7 Cushing’s, 1 TSH, 1 Gn secreting) 338 had surgical intervention; 11 with complete resection 187 transfrontal approach, 24 trans-sphenoidal approach, 35 had no surgery Median f/u of 10.5 yrs M. Brada et al, Clinical Endocrinology (1993) 38, 571-578 Radiation Therapy Post-op RT to prescribed dose of 45-50 Gy in 25-30 fxs delivered at ≤ 1.8Gy/fx Three-field technique aimed at a target volume encompassing the tumor and a 12cm margin Patient treated in supine position M. Brada et al, Clinical Endocrinology (1993) 38, 571-578 Results Years after RT Progression free survival 5 96% 10 94% 20 88% M. Brada et al, Clinical Endocrinology (1993) 38, 571-578 Results Extent of surgical resection did not correlate with outcome Relative risk of death compared with normal population was 1.76 (p<0.001) No prognostic factors for survival were identified Morbidity of RT was low 1.5% of pts had assumed radiation induced visual deterioration Cumulative risk for 2nd brain tumor at 20 yrs was 1.9% M. Brada et al, Clinical Endocrinology (1993) 38, 571-578 Conclusions High tumor control rate and low toxicity in nonfunctional pituitary adenomas suggests that limited surgical approach and postsurgical conventional fractionated EBRT should be the treatment of choice M. Brada et al, Clinical Endocrinology (1993) 38, 571-578 Results of surgery and irradiation or irradiation alone for pituitary adenomas Retrospective review of all patients with pituitary adenoma treated with RT alone, surgery and RT, or RT following surgical failure Grigsby et al, J of Neuro-Oncology 6: 129-134 (1988) Methods 212 patients with pituitary adenoma underwent treatment between 1954 and 1982 Median f/u was 11.9 yrs Radiologic evaluation consisted of skull films, angiography, pneumoenchephalography, ventriculgraphy, CT and MRI 73% had transfrontal approach Grigsby et al, J of Neuro-Oncology 6: 129-134 (1988) Radiation Therapy RT Number of Patients Orthovoltage X-rays 12 Cobalt 60 8 4 MV X-rays 13 18-25 MV X-rays 175 Grigsby et al, J of Neuro-Oncology 6: 129-134 (1988) Radiation Therapy Most patients treated with parallel-opposed portals Mean field sizes: 32.1 cm2 for EBRT alone, 45.3 cm2 for surgery and EBRT, and 40.3 cm2 for EBRT for surgical failures Median dose for all patients is 4967 cGy Pts receiving EBRT only had a mean dose of 3989 cGy; post-op EBRT 4493 cGy, and 4553 for EBRT salvage of surgical failures Grigsby et al, J of Neuro-Oncology 6: 129-134 (1988) Grigsby et al, J of Neuro-Oncology 6: 129-134 (1988) Grigsby et al, J of Neuro-Oncology 6: 129-134 (1988) Grigsby et al, J of Neuro-Oncology 6: 129-134 (1988) Conclusion Overall survival after treatment for all patients is not significantly different from an age, sex, and race matched population Patients receiving surgery and post-op RT had a greater control of local disease EBRT salvage of surgical failures is possible EBRT treatment results in a low complication rate Grigsby et al, J of Neuro-Oncology 6: 129-134 (1988) Gamma-Knife Radiosurgery Gamma knife radiosurgery for pituitary adenomas Retrospective review of 79 pts treated with GKS for pituitary adenomas Purpose: To look at the clinical results of GKS and both its efficacy and safety in treatment of pituitary adenomas Masahiro et al, J of Neurosurgery (Suppl 3) 93:19-22,2000 Methods 79 of 108 pts treated between 1993 to 1999 with GKS whom f/u exceeded 6 mo. 56 FAs ( 29 acromegaly, 15 prolactinomas, 12 Cushing’s) and 23 NFAs Mean age 50.2 yrs (26 y/o – 82 y/o) 49 female and 30 male Mean tumor vol. 7.1 cm3 Masahiro et al, J of Neurosurgery (Suppl 3) 93:19-22,2000 Radiosurgical Treatment 40 pts (24 FAs and 16 NFAs) underwent pre-GKS surgical resection Mean margin dose – 22.5 Gy (FA 24.2 Gy, NFA 19.5) Highest possible isodose (50-70%) used Mean f/u period of 26.4 months Tumor control= decreasing or unchanged tumor vol. Endocrinologic improvement=fall in elev. hormone level Masahiro et al, J of Neurosurgery (Suppl 3) 93:19-22,2000 Results Tumor control – 93.6% (NFA 95.6%, FA 92.8%) Tumor shrinkage – 24.1% (NFA 26.1%, FA 23.2%) Endocrinological improvement – 80.3% Endocrinological normalization – 30.3% 5/6 pts with preexisting visual field showed improvement 3 pts. developed complications Masahiro et al, J of Neurosurgery (Suppl 3) 93:19-22,2000 Conclusion Tumor growth control results achieved with GKS is similar to those for fractionated RT GKS may produce better results than conventional RT in tx of pituitary adenoma produced endocrinopathies GKS seems to be safer than fractionated RT in terms of complications Masahiro et al, J of Neurosurgery (Suppl 3) 93:19-22,2000 Pituitary Adenoma: The efficacy of RT as the sole treatment Retrospective study of 29 patients with nonfunctional or prolactin secreting macroadenomas Tumor dose – 4500 cGy in 4-5 wks Tumor controlled in 93% of pts Conclusion: RT is effective for improving vision and can normalize hyperprolactinemia Doses need not exceed 4500 cGy in 25 fxs Rush SC, Newall J., Int J Radiat Oncol Biol Phys 1989; 17:165 General Management Pituitary adenoma management is complex and is dictated by size, symptoms, and character of tumor Treatment options require multiple modalities, including: Surgery, RT, SRS, and medical management General Management Multidisciplinary approach Goals: Define tumor extent Evaluate hormone activity Remove tumor mass Control hypersecretion Correct endocrine deficiencies General Management Microadenomas: transsphenoidal surgery or RT Macoradenomas: initial surgery with postop RT Medical Management Bromocriptine Somatostatin Treatment Algorithm Pre-treatment MRI Close to Chiasm? yes Visual field testing Deficit yes Surgery no Surgery EBRT no Surgery EBRT SRS/gamma-knife Appropriate for GKS Contraindication for GKS RT Dosing Guidelines Nonfunctioning tumors Functioning tumors EBRT (1.8Gy/fx) Radiosurgery (optic chiasm dose < 9 Gy) Local Tumor Control Biochemical Control 45-50.4 Gy 12-24 Gy to margin 95% NA 45-54 Gy 25-30 Gy to margin 9095% 33-95% Complications Hypopituitarism Vision loss Carcinogenic Radiation necrosis Cerebral Infarction Future Directions Profiles of toxicity in the 2-D vs. 3-D era Thank You Faculty Residents