OSA in Children An ENTs Perspective Haidy Marzouk, MD Assistant Professor
advertisement

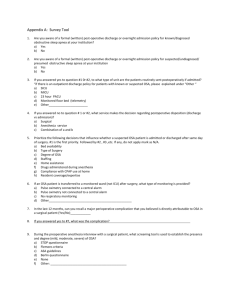
OSA in Children An ENTs Perspective Haidy Marzouk, MD Assistant Professor Department of Otolaryngology SUNY Upstate Medical Center FINANCIAL DISCLOSURES None OTHER DISCLOSURES Worried parents and tough questions make us better OUTLINE Do we really have to do this? Will he/she behave better? Will he/she lose weight? How is the recovery like? What are the risks? Is tonsillectomy and adenoidectomy all you can offer? DO WE REALLY HAVE TO DO THIS? INTRODUCTION Long term affects of sleep apnea include: T&A can improve – BP, inflammatory markers, and correlation with reduction in asthma symptoms shown pulmonary and cardiovascular changes Failure to thrive in some Impaired cognition, focus, behavioral disturbance Increased inflammatory markers in the body Abnormal bite Impaired quality of life Those who have preop PSG – 38% severe BP and inflammatory markers don’t improve as much in obese children Won’t it affect his immune system?? Well can’t he/she just grow out of it?? It’s just mild… It’s just mild Apnea Research has demonstrated poor correlation between AHI and QOL Neither obstructive AHI or REM AHI correlates with OSA-18 scores Exception is oxygen saturation Prospective study Other PSG parameters don’t reflect burden on QOL in children Baldassari CM, Alam L, Vigilar M, Benke J, Martin C, Ishman S. Otolaryngol Head Neck Surg. 2014 Oct;151(4):687-91 Baldassari CM, Alam L, Vigilar M, Benke J, Martin C, Ishman S. Otolaryngol Head Neck Surg. 2014 Oct;151(4):687-91 It’s Just Mild Apnea For mild apnea specifically, T&A better than watchful waiting Studied retrospectively T&A group mean reduction in AHI from 3.5 to 2.69 Observation group worsened from 3.09 to 5.18 Average time for post op PSG 10 months Exception – obese children had no difference between groups What’s mild? In this study, considered AHI between 1 and 5 What’s cure? Trosman SJ, Eleff DJ, Krishna J, Anne S. Int J Pediatr Otorhinolaryngol. 2016 Apr;83:25-30 WILL HE/SHE GROW OUT OF IT ? Randomized control studies of children ages 5-9 PSG findings, QOL, neurocognitive functioning, attention/executive function, behavior studied over 7 months Groups early T&A vs. watchful waiting QOL and PSG findings? Kids did better in T&A group over time Normalization of AHI - 79% vs. 46%, P<0.001 Some data shows watchful waiting kids who are younger get worse over time Marcus CL, etal. ; Childhood Adenotonsillectomy Trial (CHAT).N Engl J Med. 2013 Jun 20;368(25):2366-76 Garetz SL, Mitchell RB, Parker PD, Moore RH, Rosen CL, Giordani B, Muzumdar H, Paruthi S, Elden L, Willging P, Beebe DW, Marcus CL, Chervin RD, Redline S. Pediatrics. 2015 Feb;135(2):e477-86 BUT HIS/HER TONSILS ARE SMALL?! Retrospective and case control studies– no correlation between tonsil size and OSA severity Kids with bigger tonsils had greater proportion of resolution after surgery All sizes benefitted from surgery Tang A, Benke JR, Cohen AP, Ishman SL. Otolaryngol Head Neck Surg. 2015 Aug;153(2):281-5 Hwang SH1, Guilleminault C, Park CS, Kim TW, Hong SC. Otolaryngol Head Neck Surg. 2013 Aug;149(2):326-34 WHAT ABOUT THE CENTRAL APNEAS? Children with OSA and mild CSA on preoperative PSG showed significant improvement in CAI following adenotonsillectomy 73.3% resolution CO2 retention and elevation? Otolaryngology– Head and Neck Surgery 146(3) 487–490 Changes in Central Apnea Index following Pediatric Adenotonsillectomy CENTRAL APNEA Improvement in Down’s Syndrome patients as well Otolaryngology–Head and Neck Surgery2015, Vol. 153(4) 644–648 WILL HE/SHE BEHAVE BETTER? CHAT STUDY 2013 NEJM 464 children ages 5 to 9 randomly assigned to early T&A versus watchful waiting Studied at baseline and 7 months later Developmental Neuropsychological Assessment – no difference Significantly greater improvements in overall behavioral and QOL measures Previous studies found benefits maintained longer term (2.4-3.6 years) Change not as great over time, but still significant N Engl J Med. 2013 June 20; 368(25): 2366–2376 Chung S, Hodges EK, Ruzicka DL, Hoban TF, Garetz SL, Guire KE, Felt BT, Dillon JE, Chervin RD, Giordani B. Int J Pediatr Otorhinolaryngol. 2016 Jan;80:21-5 NEUROCOGNITION 2016 meta-analysis on patients ages 2.5-14 Improved neurocognitive function and IQ Case controlled Some of the studies conflicted Correlated to AHI improvement Especially with preschool children Neuroplasticity Song SA, Tolisano AM, Cable BB, Camacho M. Int J Pediatr Otorhinolaryngol. 2016 Apr;83:205-10 Compared low IQ versus high IQ children Both have the same improvement Findings independent of BMI Chung S, Hodges EK, Ruzicka DL, Hoban TF, Garetz SL, Guire KE, Felt BT, Dillon JE, Chervin RD, Giordani B. Int J Pediatr Otorhinolaryngol. 2016 Jan;80:21-5 OSA AND DEPRESSION 2013 meta-analysis 11 studies n=894 Medium relationship between OSA and depressive symptoms Independent of BMI Medium improvement in symptoms after T&A Recommendation that children with depression get screened for SDB In both primary snoring and OSA symptoms were similarly elevated ADHD AND OSA Systematic review and meta-analysis Case controlled analysis n=1113 in treatment group, n=1405 in watchful waiting Mean age 8 years old Medium relationship between OSA and ADHD symptoms Medium relationship effect with T&A 13 month follow up Sedky K, BeAmiri S, AbdollahiFakhim S, Lotfi A, Bayazian G, Sohrabpour M, Hemmatjoo T. Int J Pediatr Otorhinolaryngol. 2015 Aug;79(8):1213-7 Bennett DS, Carvalho KS. Sleep Med Rev. 2014 Aug;18(4):349-56 WHAT ABOUT HIS/HER WEIGHT? WEIGHT GAIN OR LOSS Children usually GAIN weight greater than expected after T&A compared to watch and wait group Contrary to previous thinking When compared to kids without apnea… Obese kids tend to gain more weight compared to their obese peers Normal weight kids don’t tend to gain more in one study Children of all categories of baseline weight Children of all severities of apnea Katz ES, Moore RH, Rosen CL, Mitchell RB, Amin R, Arens R, Muzumdar H, Chervin RD, Marcus CL, Paruthi S, Willging P, Redline S. Pediatrics. 2014 Aug;134(2):282-9 THEORIES Decreased work of breathing at night creates less calorie burning They’re less hyperactive and burning less calories It’s easier to eat without large tonsils and appetite increases SHOULD OBESE CHILDREN GET T&A? Chance of cure less ~26% for AHI <1.5 ~50% for AHI <5 Still a significant AHI reduction even in severely obese children MRI findings of obese kids after T&A shown to have tendency for residual NP fullness However, these children are at risk for further weight gain, which can influence OSA as well Is it worth it to operate for mild apnea?? Still not enough evidence to not treat with T&A HOW IS THE RECOVERY? WHAT ARE THE RISKS? RECOVERY/RISKS My part is the easy part 9% risk of respiratory compromise Increased risk with: severity of OSA, low body weight, young age 2-4% risk of bleeding – lasts for 2 weeks Dehydration PAIN Recovery period about 2 weeks De Luca Canto G, Pachêco-Pereira C, Aydinoz S, Bhattacharjee R, Tan HL, Kheirandish-Gozal L, Flores-Mir C, Gozal D. Pediatrics. 2015 Oct;136(4):702-18 PARTIAL INTRACAPSULAR TONSILLECTOMY (PITA) Tonsil “debulking” leaving a small amount of tonsil behind Biological dressing Efficacy equivalent with regards to OSA Less pain Less risk of dehydration Faster return to diet and activity Less risk of bleeding Shorter admissions (less cost?) Risk of regrowth - ~3.5% Risk of recurrent tonsillitis equivalent to nontonsillectomy group Acevedo JL, Shah RK, Brietzke SE. Otolaryngol Head Neck Surg. 2012 Jun;146(6):871-9 Ericsson E, Graf J, Lundeborg-Hammarstrom I, Hultcrantz E. J Otolaryngol Head Neck Surg. 2014 Jul 27;43(1):26 IS TONSILLECTOMY THE ONLY INTERVENTION? WHAT ABOUT THE NOSE? NASAL OBSTRUCTION AND SLEEP Nasal obstruction, irrespective of cause contributes to sleep quality of life Allergic rhinitis is a risk factor for OSA and decreases long term QOL after T&A Receptors present in the nasopharynx to control muscle tone in upper airway Muscle tone higher with nasal breathing during sleep Obese children have higher anterior nasal resistance The most accurate way to diagnose nasal obstruction severity in correlation with symptoms is through nasal endoscopy Alkhalil M1, Lockey R. Ann Allergy Asthma Immunol. 2011 Aug;107(2):104-9 TREATMENT OF NASAL OBSTRUCTION Mometasone Improves snoring Improves scores on OSA 18 Shrinks adenoids with 4 week trials Inferior turbinate reduction Improves nocturnal breathing When appropriate and performed with T&A, creates further improvement than T&A alone Diagnose and treat obstruction and don’t assume adenoidectomy alone is sufficient Chohan A, Lal A, Chohan K, Chakravarti A, Gomber S. Int J Pediatr Otorhinolaryngol. 2015 Oct;79(10):1599-608 Jung et al. Clin Exp Otorhinolaryngol. 2011 Mar;4(1):27-32 Cheng PW, Fang KM, Su HW, Huang TW. Laryngoscope. 2012 Dec;122(12):2850-4 CONCLUSIONS Adenotonsillectomy remains a first line and effective treatment for pediatric sleep apnea Partial Intracapsular tonsillectomy has become a valid option for treatment of pediatric OSA Considerations and appropriate counseling must be given to the obese pediatric patient with regards to surgery Nasal obstruction must be part of the treatment plan for OSA THANK YOU OTHER SOURCES Mangiardi J, Graw-Panzer KD, Weedon J, Regis T, Lee H, Goldstein NA. Int J Pediatr Otorhinolaryngol. 2010 Dec;74(12):1361-6 Odhagen E, Sunnergren O, Hemlin C, Hessén Söderman AC, Ericsson E, Stalfors J. Eur Arch Otorhinolaryngol. 2016 Jan 4 Stucken EZ1, Grunstein E, Haddad J Jr, Modi VK, Waldman EH, Ward RF, Stewart MG, April MM. Laryngoscope. 2013 Nov;123(11):2868-72 Mostovych N, Holmes L, Ruszkay N, LaHurd A, Heinle R, Nardone H. JAMA Otolaryngol Head Neck Surg. 2016 Feb 1;142(2):150-6 Vicini C, Eesa M, Hendawy E, Pari M, D'Agostino G, AlGhamdi S, Meccariello G. Int J Pediatr Otorhinolaryngol. 2015 Jul;79(7):1106-10 Mukhatiyar P, Nandalike K, Cohen HW, Sin S, Gangar M, Bent JP, Arens R. JAMA Otolaryngol Head Neck Surg. 2016 Jan 1;142(1):25-31 Duarte VM1, Liu YF, Shapiro NL. Laryngoscope. 2014 Aug;124(8):1959-64 Lee CH, Hsu WC, Chang WH, Lin MT, Kang KT. Clin Otolaryngol. 2015 Oct 5 Van M1, Khan I1, Hussain SS1. J Laryngol Otol. 2016 Mar;130(3):214-8. Burstein DH1, Jackson A, Weedon J, Graw-Panzer KD, Fahmy S, Goldstein NA. Int J Pediatr Otorhinolaryngol. 2013 Apr;77(4):525-9 Jeyakumar A, Fettman N, Armbrecht ES, Mitchell R. Otolaryngol Head Neck Surg. 2011 Feb;144(2):154-8 Com G, Carroll JL, Tang X, Melguizo MS, Bower C, Jambhekar S. J Clin Sleep Med. 2015 Apr 15;11(4):467-74 Levi J, Leoniak S, Schmidt R. Arch Otolaryngol Head Neck Surg. 2012 Oct;138(10):897-901 Lewis TL, Johnson RF, Choi J, Mitchell RB. Otolaryngol Head Neck Surg. 2015 Apr;152(4):734-9 Nandalike et al. Sleep. 2013 Jun 1;36(6):841-7 Mitchell R, Boss E. Sleep. Dev Neuropsychol. 2009;34(5):650-61 Segal S, Eviatar E, Berenholz L, Kessler A, Shlamkovitch N.Am J Rhinol. 2003 MarApr;17(2):69-73 Isaac A, Major M, Witmans M, Alrajhi Y, Flores-Mir C, Major P, Alsufyani N, Korayem M, El-Hakim H. JAMA Otolaryngol Head Neck Surg. 2015 Jun;141(6):550-5 Cheng PW, Fang KM, Su HW, Huang TW. Laryngoscope. 2012 Dec;122(12):2850-4 Alkhalil M1, Lockey R. Ann Allergy Asthma Immunol. 2011 Aug;107(2):104Sin S1, Wootton DM, McDonough JM, Nandalike K, Arens R. Laryngoscope. 2014 Nov;124(11):2640-4 Kim DK1, Han DH2. Int Forum Allergy Rhinol. 2015 Aug;5(8):741-6 Otolaryngology–Head and Neck Surgery146(6) 871–879 Otolaryngology–Head and Neck Surgery147(3) 538–543 Otolaryngology–Head and Neck Surgery 2015, Vol. 152(5) 931–940 Elisabeth Ericsson a,b,*, Inger Lundeborg c, Elisabeth Hultcrantz International Journal of Pediatric Otorhinolaryngology 73 (2009) 1254–1262