The Team Check-up Tool On the CUSP: STOP BSI © 2009
advertisement
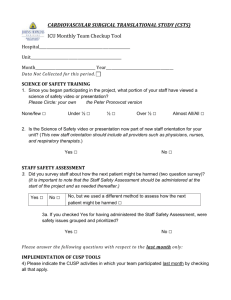
On the CUSP: STOP BSI The Team Check-up Tool © 2009 Learning Objectives • To understand the tool we use to: – Describe the anticipated activities of your ICU quality improvement team – Track implementation progress and the context of progress – Assess barriers to progress – Monitor interactions on the team • To think about how the tool can be useful to you © 2009 The Quality Improvement Team • Core team working on the CUSP/ CLABSI project • The small group that spreads the intervention to the rest of the ICU © 2009 Importance of the Quality Improvement Team • This team has the greatest impact on how the intervention is “rolled out” at your site (absolute power) • Potential implications of a poor job − Slower implementation − Gaps/ uneven implementation − Higher continued risk (infection, $, lives) © 2009 TCT Measures: • Engagement/ educational activities of the QI team (on BSI and CUSP) • Participation in CUSP activities • Extent of implementation on unit • Barriers to progress • Interactions on team © 2009 Team Activities-Keeping on Track • Team meetings (recommend 2/mo) • Review of data (monthly) • Meet w/ Exec Partner on unit (monthly or more) • Executive review of data (monthly) • Presentations to the Hospital Leadership and Board of Directors © 2009 Education and Engagement Activities on the Unit • Modeling the line placement steps; stopping insertions that violate protocol; having one-on-one talks where necessary • CUSP Activities − Science of safety video − How will we harm the next patient? exercise − Daily Goals − Morning Briefing − Learning from a defect − Executive Partnership © 2009 Education and Engagement Activities on the Unit • More Activities (add your ideas!) − Internal seminar for staff − Present project at all committee meetings − Make BSI prevention part of a skills fair − Have IC dept visit/ give a talk − In-services/ demos − New written policy − Post the steps and progress updates − Put the prevention practices on all clipboards − Update/ prepare line cart/ kit with checklist − Hand out Fast Facts one-page info sheet © 2009 Barriers to Progress • Turnover on QI Team • Spread to other parts of the hospital • Disruptive events • Lack of skills • Lack of time • Lack of buy-in • Lack of support • Lack of autonomy © 2009 Interactions among Team Members • Team agrees on goals • Team values individual contributions • Team can resolve conflicts • Team is unified © 2009 Action Items • Look over the tool • Think about what elements are most important to watch • Share TCT data with executive partner • Make a strategic plan to address identified barriers early © 2009 Reference List • Lubomski, Lisa H., Jill A. Marsteller, Yea-Jen Hsu, Christine A. Goeschel, Christine G. Holzmueller, and Peter J. Pronovost, “The Team Checkup Tool: Evaluating Quality Improvement Team Activities and Giving Feedback to Senior Leaders,” Joint Commission Journal of Quality and Patient Safety, October 2008. • Marsteller, Jill A., Christine G. Holzmueller, Martin Makary, J. Bryan Sexton, David Thompson, Lisa H. Lubomski and Peter J. Pronovost. “Developing Process-Support Tools for Patient Safety: Finding the Balance Between Validity and Feasibility,“ Joint Commission Journal of Quality and Patient Safety, October 2008. © 2009