On the CUSP: STOP BSI Improving Situational Awareness by
advertisement

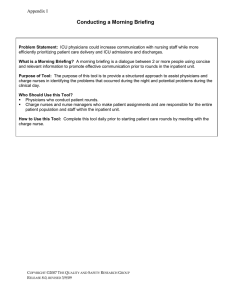
On the CUSP: STOP BSI Improving Situational Awareness by Conducting a Morning Briefing Situation Awareness An Overview • Members of the team have an understanding of “what’s going on” and “what is likely to happen next.” • Teams are alert to developing situations, sensitive to cues and aware of their implications. 2 Briefing Defined A Briefing is a discussion between two or more people, often a team, using succinct information pertinent to an event. What a briefing immediately does: 1. Maps out the plan of care 2. Identifies roles and responsibilities for each team member 3. Heightens awareness of the situation 4. Allows the team to plan for the unexpected 5. Allows team members’ needs and expectations to be met 3 Effective Briefings Sets the tone for the day… chaotic versus organized and efficient Encourages participation by all team members Owned by all team members • Organized in thought regarding the procedure • Establishes competence: • who has what skills • who performs what • who knows what • Predicts what will happen later • Plans for the unexpected (include equipment, medications, consults) 4 When to Conduct Briefings Beginning of the day - Morning Briefing Prior to any procedure in any setting Situational – change in patient status results in deviation from plan of care Reporting-off-breaks, change of shift 5 Who Participates 1. The Physician doing rounds who is responsible for the ICU patients that day 2. The Night Charge Nurse 3. The Day Charge Nurse 6 Morning Briefing Process • Three simple questions: – What happened overnight that I need to know about? – Where should I begin rounds? – Do you anticipate any potential defects in the day? 7 What Happened Overnight That I Need to Know About? • You should be thinking about…was there adequate coverage? • Were there any equipment issues? • Were new cases posted to the ICU? • Unexpected changes in patient acuity? • Were there any adverse events? 8 Where Should Rounds Begin? 1. Is there a patient who requires my immediate attention secondary to acuity? 2. Which patients do you believe will be transferring out of the unit today? 3. Who has discharge orders written? 9 As you continue planning rounds 4. How many admissions are planned today? 5. What time is the first admission? 6. How many open beds do we have? 7. Are there any patients having problems on an inpatient unit? 10 Do You Anticipate Any Potential Defects in the Day? • Patient scheduling • Equipment availability/ problems • Outside Patient testing/Road trips • Physician or nurse staffing • Provider skill mix 11 When You Identify Defects / Problems • Want to assign a person to the issue - have them follow up • Identify actions taken to meet any patient or unit needs • Report back to the staff what those actions were or will be • If ongoing - continue to report it during morning briefing until it is resolved or alternatively use Appendix E Status of Safety Issues. 12 Appendix E Status of Safety Issues- Cusp Unit: ___________________________________________ Date Date Safety Issue New and Ongoing Contact Status Goal Safety Issue Completed Contact Status Goal Please return this form to your project leader On the CUSP: Shadowing Another Provider 14 Why Do We Need to Shadow? • To gain perspective of the other providers – Practice – Responsibilities – Work environment • To identify issues that affect teamwork and communication that may impact patient care, patient care delivery and outcomes 15 Who should have this experience? • Patient care areas as part of the Comprehensive Unit Based Safety Program (CUSP) • Staff involved in the delivery of patient care in units where culture score indicate a poor score in teamwork and safety • When there is a difference of > 20% in culture scores between provider types • As part of orientation to a new unit • Units with little collaboration between disciplines 16 How To? • Review the tool prior to your shadowing experience • Follow your health care provider through their daily activities. • Review your list of communication and teamwork problems • Discuss with the Provider • Make a plan for resolution 17 Review the Tool Set up with questions and prompts for the personnel using it. You should make changes that are specific to your unit! 18 Section 1 1. Were any health care providers difficult to approach? – Things to think about: – How did that impact the health care provider you followed? (obtained an order, ignored etc.) – What was the final outcome for the patient? (delay in care, etc.) 19 Section 2 2. Did one provider get approached more often for patient issues? – Things to think about: Was it because another health care provider was difficult to work with? 20 Section 3-5 3. Did you observe an error in transcription of orders by the provider you followed? 4. Did you observe an error in the interpretation or delivery of an order? 5. Were patient problems identified quickly? 21 If You Were Following a Nurse: 1. Did you observe that in a crisis or when there was an important issue, a nurse’s page or phone call was not returned quickly? 2. What was the outcome for this patient? 22 If You Were Following a Physician 1. If you are following a physician, what were the obstacles that a physician faced in returning calls or pages? 2. What other factors impacted their ability to see patients? 23 How Would You Assess • Handoffs • Communication During a Crisis • Provider Skill • Staffing 24 III. What will you do differently in your clinical practice? IV. What would you recommend to improve teamwork and communication Specific Recommendations Actions taken 25 Our Findings • Handoffs for 4 hour shifts not thorough, increased opportunity to forget key details as this increased the total number of people… • Physician consults usually obtained but not always read by the requesting team… • Nurse often most informed but does not always speak up 26 Our Findings • Nurse is the provider most often left with patient information to pass on to another provider - few conversations from MD to MD. • Pharmacists did not realize how critical supplying Pyxis and stock drugs were. • Some providers avoided… • EMR was not accessed… 27 Our Findings • Nurses did not realize how complicated sterile processing was, efforts made to keep trays together. • POE removed an important step - communicating to RN of stat order. • Physicians unaware of unit policies, depend on RNs to complete task. 28 Our Findings • Some nursing practice should be used hospital wide such as labeling. • Isolation policies not adhered to - primarily physician personnel, consults - Required RNs to speak up. • Assertiveness training indicated. 29 Discussion • Questions? 30