Congenital Heart Disease: Not Just for Kids Anymore
advertisement

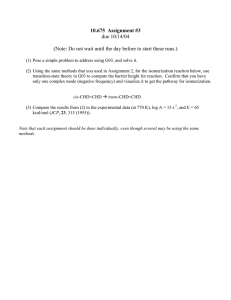
Congenital Heart Disease: Not Just for Kids Anymore Jane E. Crosson, MD Associate Professor, Pediatric Cardiology Director, Adult Congenital Heart Disease program Johns Hopkins Hospital Goals of Talk • Define congenital heart disease • Discuss how improved treatment has ballooned the number of adults living with these conditions • Review barriers to effective treatment of adult congenital heart disease patients What is congenital heart disease? aka “CHD” • Defects in the heart structure that occur during fetal heart development • Almost 1% live births (most common birth defect) • Range from simple ‘holes’ in the heart, or narrowed heart valves to hearts with only ½ of the needed structures Normal heart What is congenital heart disease? aka “CHD” “Tricuspid atresia” is an example of a heart with only ½ of the needed structures Blue blood has to go to the other side of the heart Severely underdeveloped right side of the heart: no heart valve between upper and lower chambers Left (only) pumping chamber The Journey to Survival • Prior to the 1940s, children with severe CHD had an >80% chance of dying before they reached adulthood • Now they have a 90% of surviving well into adulthood How did we get there? Collaboration: cardiologists, surgeons, researchers Johns Hopkins Hospital circa 1940 Dr. Alfred Blalock, surgeon Dr. Helen Taussig, pediatric cardiologist Vivian Thomas, lab technician extraordinaire Johns Hopkins 1944: “Something the Lord Made”: The Blalock-Taussig Shunt 1st “blue baby” surgery Goal: provide reliable blood flow to the lungs •Partners of the Heart: Vivien Thomas and His Work with Alfred Blalock, by Vivien T. Thomas, University of Pennsylvania Press, 1985. ISBN 0-8122-1634-2 The modern era: increasing survival for patients with CHD • 1952: Heart-lung bypass machine 1st used successfully for CHD repair • 1963: Mustard: First successful operation for babies with fatal CHD condition called “transposition of the great arteries” • 1971: First operation to separate the blue and the red blood in patients with only one pumping chamber like tricuspid atresia (“Fontan” procedure) • 1981: First surgery for “HLHS”, previously uniformly fatal …..And on and on Dr. Mustard in the Parlor 1st “Mustard” patient at her 16th birthday party Arterial Switch Operation: 1980s-present Simple! move hair thin structures in a heart the size of a walnut <½ inch! Detach/Re-implant coronary arteries) PA AO Fast-forward 70 years: Continued improved survival in CHD due to: Expanding population of adults with CHD Improved re-operation, treatment for arrhythmias Lower perioperative mortality Improved surgical techniques Fetal diagnosis Congenital Heart Disease Early complete repair PGE1, Advances in NICU care Great problem to have: Survival into Adulthood with CHD ~90% 1980s 1970s 1960s 1940s 0% 20% 40% 60% 80% 100% The changing face of Congenital Heart Disease 2010 Adults Children 1985 1965 0% 20% 40% 60% 80% 100% • More adults now than children with CHD • >1,000,000 adult CHD pts in US • Increasing by 5% per year Meeting the needs of adults with congenital heart disease Most patients with CHD are not ‘cured’ of their disease – They get sick more often and have a higher risk of death than general population – Majority are self-supporting, but others have physical and cognitive limitations – Life-long follow-up is needed, but 30-50% of patients are lost to follow-up in adulthood Where do we go from here…. Now that all of the children are growing up? • Need well-trained specialists to take care of all these adults with very specialized problems • However, adult cardiologists traditionally have not been trained to care for these patients, since they didn’t live long enough to reach adulthood Barriers to effective care for adult CHD patients • Lack of enough dedicated adult CHD facilities • Fragmented care among primary care doctors, adult cardiologists, & pediatric cardiologists • Paucity of adult cardiologists with CHD experience • Lack of coordinated management of contraceptive and pregnancy needs Improved insurability • Historically, patients had limited health options: insurance – Work for a large company – Go on disability (not always qualifying) • Changes in SSI regulations have expedited disability processing for the most severely affected (2012) • ACA has enabled most others to obtain health insurance without the burden of paying for their pre-existing condition Congenital Heart Futures Act authorized NIH funding for CHD research & created National Congenital Heart Surveillance System Canadian Model for Adult CHD Care • 15 Regional Adult CHD Centers The Good: • Well-coordinated, top-of-the-line care • Database support for outcomes research The Bad: • Big country, lot of traveling to get to these regional centers for many patients How well does the Canadian model work? Survey of 360 young adult CHD pts, ages 19-22 in Canada – Less than ½ successfully transferred care to specialized adult CHD clinics – 27% had no cardiac follow-up since turning 18 – Successful transfer associated with • More heart surgeries • Older age at last follow-up in pediatric center • Documentation of advice to follow-up in ACHD center Attending clinic without parents ** strongest predictor hands-down** Reid, et al. Pediatrics 2004 32nd ACC/AHA Bethesda Conference • Convened in 2000 by American College of Cardiology to study the needs of adult CHD patients • Major Recommendations: – Increase education of adult CHD providers – Need 30-50 US regional ACHD care centers – Adults with moderate or complex CHD to receive regular care at these centers – Physicians without specific expertise in CHD should see patients in collaboration with adult CHD center – Major interventions should be performed in regional centers Problems with nd 32 Bethesda Conference • Patients unwilling/unable to travel to regional centers • Not enough physicians trained – New board certification now available may actually inhibit increase in personpower (another $2800 plus study time, etc.) • Pediatric and adult cardiologists unwilling to “give up” patients: emotional, economic factors, etc. Most recommendations have not translated into action Different models evolving • Programs based in children’s hospitals with adult hospital affiliations, or vice versa • Johns Hopkins: Pediatric cardiologists consult on management of inpatients with CHD, run outpatient service • Baltimore-Washington area – Separate programs in major academic centers – Most link pediatric and adult cardiologists; surgical colleagues cover pediatric and adult operating suites – Regional consortium that meets quarterly to discuss cases, exchange ideas, work on research projects Conclusions • Successful care of congenital heart disease has resulted in steady increase in number of adults living with wellpalliated disease • Most adult CHD patients can live long and productive lives • Goals: – build on the work done by the pioneers like Taussig and Blalock – improve health care delivery to these patients • Better data collection and outcomes research needed