Incontinence in Women Neena Agarwala, M.D.
advertisement

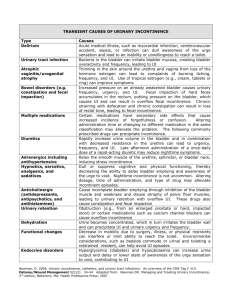
Incontinence in Women Neena Agarwala, M.D. Prevalence • • • • 8-51% in community Atleast 50% in nursing homes 25% suffer from severe incontinence Greatest in older women and increases with age • Incontinence 6-10x greater in women than in men • By 2040 22% of female population will be>65 Impact on quality of life • Significant worldwide health problem • Affects 16 million women in US • Cost of diagnosing and managing UI exceed $26 billion annually in US • Adult diaper sales $5-6 billion/yr • Great social impact as well • Leaking – depression – stop exercise – gain weight – and so on --- ---- Approach • Every woman is different • Consider quality of life from the patient’s point of view • History • Voiding diary • Quality of life assessment Normal Bladder Function • Functional urethra is intra-abdominal • Increased abdominal pressure transmitted equally to bladder and urethra • With increased stress urethro-vescial junction responds to stress by closing tight • Bladder is a voluntary smooth muscle • Inherent ability to maintain low pressure with filling-increase in volumecompliance History • • • • • • • Diabetis mellitus Thyroid disease Multiple sclerosis Stroke Back pain or injuries Surgery Medications – – – – – – – – Alpha methyldopa Prazosin Phenothiazines Diazepam Diuretics Antihistamines Anticholinergics Dosage increases • Closed angle glaucoma Physical Examination • • • • • • • • • • • • • • • • • • • Age Estrogen status – menopause - hormones Weight – Obesity Neurologic status Mobility and gait Thoracic, lumbar and sacral nerves Motor strength Sensory status and anal wink Pelvic muscle strength – Kegel squeeze Vulva – atrophy Vagina – infection Urethra – diverticula, urethritis Urethral mobility Urine in vagina Prolapse – cystocele, rectocele, uterine or vault prolapse Stress test with bladder ~1/2 full Post void residual Urinalysis and culture Simple or complex cystometric evaluation Classification • Genuine (true) Stress incontinence ~50% • Urge incontinence ~30% • Mixed incontinence ~20% • Overflow incontinence • Total incontinence • Unclassified incontinence Stress Incontinence • Continent at rest or minimal activity • Incontinent with stress – – – – Exercise Coughing Sneezing Heavy lifting • UV junction is no longer above the urogenital diaphragm and doesn’t see the increased stress Signs and symptoms • History of loss of urine with stress • Absence of frequency, urgency, dysuria – Nl U/A and negative culture • PE shows loss of anterior support, possible cystocele – Q-tip test shows greater than 30 deg deviation • May have other prolapses • Demonstrated loss of urine with cough • Neurological exam – sensory & motor- nl Cystometric Evaluation • Simple- After void, insert foley, measure PVR, <50cc. Attach syringe to foley, instill sterile saline. Normal first desire ~200cc. • Observe column of saline, unusual waves suggest detrusor dyssynergia. • Maximum bladder capacity ~500 cc. • Remove ~250 cc, remove foley, ask to cough, loss of urine suggests GSI. Definition Genuine Stress Urinary Incontinence (GSUI) • involuntary loss of urine with a rise in intra-abdominal pressure in the absence of any rise in detrusor pressure • Urethral hypermobility Helpful hints • Stress induced detrusor instability – May be confused with GSI – See loss of urine after cough, but delayed – Bladder overactive after stress • Incontinence may only be seen in standing position • Correction of the cystocele may produce incontinence since UVJ slightly kinked Non surgical therapy • Occlusive devices – Pessaries – Incontinence dishes • Strengthening pelvic floor musculature – Kegel exercises – Physical therapy for pelvic floor rehabilitation • Biofeedback • Electrical stimulation • Local Estrogen therapy Surgery? • Bonney test: Gentle support of bladder neck during exam and asking patient to cough again • If continent, surgical repair is likely to be successful • Surgical repairs aim at elevation of bladder neck and correction of the pubovesical fascia tears – Burch Urethropexy, Marshall-Marchettikrantz procedure – Sling procedures – Anterior colporrhaphy – Paravaginal repair Intrinsic sphinteric deficiency • Incontinence type III, a variant of GSUI • Unhealthy urethra • • • • – – – – Advanced age Inadequate estrogen Neurologic lesions Vaginal surgery Severe incontinence Leaks with each step Supporting the UVJ will not help Need to bulk up the urethra – almost obstruct it Urge Incontinence • Loss of urine associated with uncontrollable urge to void • Uninhibited, involuntary detrusor contractions • Pressure-volume relation out of balance • Also called unstable bladder • Frequency • Urgency • nocturia • Chronic irritation due to infection, irritation or tumors Treatment • Primarily medical • Most commonly anticholinergics – – – – Ditropan – oxybutynin chloride Detrol Imipramine Levbid, cytospaz – hyoscyamine sulphate • Side effects- dry mouth, constipation etc. • Behavioral – Bladder retraining – Pelvic-floor rehabilitation Mixed Incontinence • Some degree of both stress and urge • More difficult to treat • Need to do complex urodynamic studies to determine major component • Precisely predict success with surgery • Surgery may worsen the urge component • Properly counsel patient Overflow Incontinence • Neurogenic bladder – Multiple sclerosis, spinal cord lesions, stroke – Diabetis – Trauma – Radical hysterectomy • Normal innervation absent or damaged • Loss of vesical reflexes and emptying sensation • Overdistended bladder with overflow • Complaints of fullness, pressure • Large bladder capacity • Absence of uninhibited bladder contractions • Treatment – medical – Cholinergics to increase tone and contractility • Urecholine- bethanechol Complex Urodynamic Evaluation • Needed in special circumstances – – – – – Need for surgery Failed surgical procedure Mixed incontinence anticipate voiding dysfunction post surgery Advanced prolapse • Large residual capacity • Very small bladder capacity • Urge incontinence – not characteristic, discrepancy b/w history and exam • Complex history and symptoms • Cystometry Studies • Compliance, fd 90-150ml, nd 200-300ml, sd 400-550 ml, true subtracted detrusor pressures • Valsalva leak point pressure • Amount of intraabdominal pressure needed to leak • <60 cm H2O is ISD • Urethral pressure profile • Full bladder, catheter pulled along urethra • Urethral closure pressure >30 cm H20 nl, <20 is ISD • Uroflow • Rate and pattern of urine flow • Peak flow 20-30 ml/sec • Pressure flow test • Details voiding mechanism, obstructive dysfunction, poor contractility • Voiding detrusor pressure 10-30 cm H20 is nl • Electromyography • Electrical activity of pelvic floor musculature • Timing and degree of muscle relaxation impacts voiding mechanism Urodynamic evaluation answers • 1. Does the patient have stress incontinence ? – Stress test – Valsalva leak point pressure • 2. Does she have ISD ? – Urethral pressure profile – Valsalva leak point pressure • 3. Does she have overactive bladder? – Multichannel urodynamics • 4. What is the voiding mechanism? – Uroflow – Pressure flow study – Electromyography Examination of bladder and urethra • Cystoscopy • Urethroscopy Non surgical therapy • Occlusive mechanical devices – Pessaries – Incontinence dishes • Have no serious side effects • can be done at home • Do not limit future treatment options • Often successful in treating mild to moderate incontinence. Goal of incontinence surgery Now…… • 1. Restore and/or reinforce the pubourethral ligaments at the midurethra. • 2. Restore and/or reinforce the suburethral vaginal hammock at the mid-urethra. • 3. Reinforce the paraurethral connective tissue. Support materials • Autologous • Allograft • Synthetic • Xenograft • • • • Patient’s own tissue Thigh, hip or abdomen Second incision No rejection • Donor tissue from cadavers • Have risk of disease transmission • Fascia seems to disappear • • • • Synthetic materials Foreign body reaction Prone to erosion No risk of disease transmission • Non-human donor tissue • May have risk of disease transmission • Tissue remodeling Tension free vaginal tape procedure Sling placement Guide the Needle Tip to the Abdominal Incision Tension Free…… Risks: Bladder perforation Intrinsic sphinteric deficiency • Unhealthy urethra – Advanced age – Inadequate estrogen – Neurologic lesions – Previous vaginal surgery – Radiation • Severe incontinence with spontaneous relaxation of urethra without bladder contractions • Leaks with each step • Need to bulk up the DurasphereTM • A sterile, nonpyrogenic injectable bulking material composed of pyrolytic carbon coated beads suspended in a water based carrier gel containing beta glucan. The water based carrier gel is approximately ninety seven percent water by volume and three percent beta glucan. • Injected sub-mucosally at the bladder neck. • Creates increased tissue DurasphereTM • Helps the weak muscles of the bladder neck by adding bulk to the area. The added bulk allows the bladder neck to close enough to help stop urine from leaking. InterStim® Therapy -- Sacral Nerve Stimulation (SNS) for Urinary Control • A revolutionary approach to managing urinary retention and the symptoms of overactive bladder, including urinary urge incontinence and significant symptoms of urgency-frequency alone or in combination in patients who have failed or could not tolerate more conservative treatments. Sacral Nerve Stimulation • Used for refractory urgency, frequency and non-obstructive retention • Needs a minimally invasive surgery for implantation • Simplified implant procedure, now performed percutaneously with only local anesthesia.