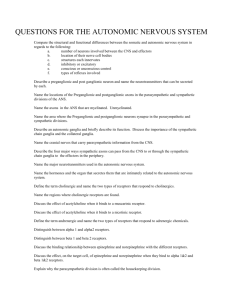
Chapter 14 Autonomic Nervous System (ANS)
advertisement

Chapter 14 Autonomic Nervous System (ANS) Due @ the final • Labs 21, 22 • Extra credit papers – Remember to mention which of the papers you read in your write up Autonomic Nervous System • Regulates the visceral response of motor neurons – Innervate smooth and cardiac muscle and glands – Make adjustments to ensure optimal support for body activities – Operate via subconscious control – Have viscera as most of their effectors • Visceral motor neurons pathways include – Preganglionic neuron (“to” the ganglion) – Postganglionic neuron (“from the ganglion) – Synapse at the ganglion Somatic versus Autonomic ANS differs from somatic • The effectors of the ANS are cardiac muscle, smooth muscle, and glands (not skeletal) • Axons of the ANS are a two-neuron chain – The preganglionic (first) neuron has a lightly myelinated axon – The ganglionic (second) neuron extends to an effector organ • Preganglionic fibers release ACh • Postganglionic fibers release norepinephrine or ACh and the effect is either stimulatory or inhibitory Two divisions of the ANS • Sympathetic • Parasympathetic Activity of both is overseen by the hypothalamus ANS: Sympathetic Division • Also called the “thoracolumbar division” and the “fight or flight” response • Involves E activities – exercise, excitement, emergency, and embarrassment • Preganglionic fibers arise from T1-L2 • Preganglionic fibers are short, postganglionic are long • All synapses are close to spinal cord Responses to Increased Sympathetic Activity 1. 2. 3. 4. 5. Heightened mental alertness Increased metabolic rate Reduced digestive and urinary functions Energy reserves activated Increased respiratory rate and respiratory passageways dilate 6. Increased heart rate and blood pressure 7. Sweat glands activated Sympathetic Division Sympathetic NS • Three parts – Sympathetic chain ganglia – Collateral ganglia – Adrenal medulla Sympathetic Chain Ganglia Communicating Rami • White Rami – preganglionic fibers • Gray Rami – postganglionic fibers Adrenal Medulla Adrenal Medulla • Preganglionic fibers entering adrenal gland proceed to center (adrenal medulla) • Modified sympathetic ganglion • Preganglionic fibers synapse on neuroendocrine cells • Specialized neurons secrete neurotransmitters into the bloodstream that act as hormones (norepinepherine, epinepherine) Sympathetic Innervation Sympathetic Neurons • Preganglionic release ACh, always stimulates the (post)ganglionic neuron • Postganglionic release NE, (except in skeletal muscles and sweat glands, which release ACh) • Remember that the response is dependent on the receptor present (NE can be excitatory or inhibitory) – Example: lung bronchi smooth muscle is inhibited by NE, opening op bronchi Postganglionic ACh • Skeletal muscles are innervated by ACh postganglionic fibers of the sympathetic division (instead of NE) • Important because ACh causes dilation of these blood vessels, whereas NE causes constriction of the blood vessels in the abdominopelvic cavity • Thus widespead sympathetic activation leads to a redistribution of blood away from skin and viscera and into skeletal muscles This allows you to run away while holding off on your digestion until later Norepinephrine • Neurons that release NE are called adrenergic • Two types of receptors bind NE – Both are indirect through G proteins • Tends to cause vasoconstriction • Much longer lasting and more modualtory than ACh ANS: Parasympathetic Division • Also known as the “rest and repose” division or the “craniosacral division” • Preganglionic neurons arise from cranial nerves 3, 7, 9, 10 and sacral segments S2-S4 and are LONG • Postganglionic neurons are short and arise close to the target organ (often in the wall of the organ itself) Parasympathetic Vagus Nerve (X) • Provides 75% of all parasympathetic outflow • Mr. parasympathetic Preganglionic fibers in the sacral segments • Do not join the ventral roots • Form the pelvic nerves Parasympathetic Nervous System Parasympathetic NS • Release ACh at both the pre- and postganglionic neurons (so ALL parasympathetic neurons use ACh) • Remember ACh binds to muscarinic and nicotinic receptors, so response will depend on type or receptor that is present Parasympathetic Activation • Centers on relaxation, food processing, and energy absorption • Localized effects, last a few seconds at most because ACh is short lived in the synapse. Why? Some Effects of Parasympathetic Activation 1. Constriction of pupils: 2. Secretion by digestive gland 3. Changes in blood flow and glandular activity associated with sexual arousal 5. Increases smooth muscle activity along digestive tract 6. Defecation 7. Contraction of urinary bladder 8. Constriction of respiratory passageways 9. Reduction in heart rate and force of contraction Comparing Sympathetic and Parasympathetic Divisions • Sympathetic: – widespread impact – reaches organs and tissues throughout body • Parasympathetic: – innervates only specific visceral structures – effects are shorter lived (why?) Anatomy of ANS Division Origin of Fibers Length of Fibers Location of Ganglia Sympathetic Thoracolumbar region of the spinal cord Short preganglionic Close to the and long spinal cord postganglionic Parasympathetic Brain and sacral spinal cord Long preganglionic and short postganglionic In the visceral effector organs Comparison of Sympathetic NS and Parasympathetic NS Effects of Drugs • Atropine – blocks parasympathetic effects • Neostigmine – inhibits acetylcholinesterase and is used to treat myasthenia gravis • Tricyclic antidepressants – prolong the activity of NE on postsynaptic membranes • Over-the-counter drugs for colds, allergies, and nasal congestion – stimulate adrenergic receptors • Beta-blockers – attach mainly to 1 receptors and reduce heart rate and prevent arrhythmias Sympathetic and Parasympathetic Autonomic Tone • Autonomic tone refers to constant activity of the cells of the ANS • An important aspect of ANS function because: – If a nerve is inactive under normal conditions, it can only increase its activity – However, if nerve maintains a constant background level of activity, then it can either increase or decrease its activity Single Innervation Case study: Blood vessels • Only contacted by sympathethic NS • NE (released at most vessels): constrictis – Thus an autonomic tone keeps the vessels half way consticted/dilated at rest • Sympathetic ACh released at skeletal muscles causes dilation Dual Innervation • Many vital organs receive instructions from both sympathetic and parasympathetic divisions (a notable exception is the blood vessels) • 2 divisions commonly have opposing effects (e.g. speed vs. slow the heart) Dual Innervation: The Heart • Receives dual innervation • 2 divisions have opposing effects: – parasympathetic division: • acetylcholine released by postganglionic fibers slows heart rate – sympathetic division: • NE released by postganglionics accelerates heart rate The Heart • Balance between 2 divisions: – autonomic tone is present – releases small amounts of both neurotransmitters continuously • Parasympathetic innervation dominates under resting conditions • How do we know this? Autonomic Innervation: The Heart • Heart rate controlled precisely through small adjustments • Crisis accelerates heart rate by: – stimulation of sympathetic innervation – inhibition of parasympathetic innervation – BOTH together allows for a bigger effect Summary: Sympathetic and Parasympathetic Divisions • Know this: Table 16-2