Electrosurgery Units (ESU’s) 1 do not print it to pdf
advertisement

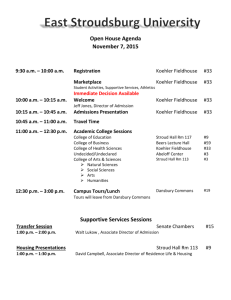
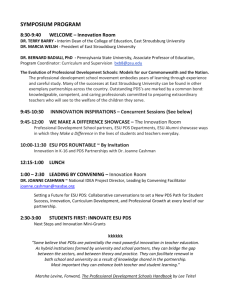
Electrosurgery Units (ESU’s) 2016-01-16 rev this is now slide 1 do not print it to pdf things to do (check off when complete): x add revision date to cover page x remove triangles x create list for pages to print in the handout 2-3,9-25,27-38,41-43,46-47,50-58,60-69,71,83 x add captions for photo slides incorporate notes taken during presentation spelling: fulguration, desiccation 2016-01-16 added key points page Electrosurgery Units (ESU’s) and their variants © D. J. McMahon 150107 rev cewood 2016-01-16 Key Points Electrosurgical Units: - typical output frequency of modern ESU’s - difference in return circuit between of monopolar and bipolar modes - difference in waveforms between Cut, Coag, and blend modes - principle of Return Electrode Monitoring - fulguration, desiccation, ablation, ligature - know what the “crest factor” is - Argon beam coagulators - hazards of return electrodes - know the principle of the harmonic scalpel - four essentials of maintenance of ESU’s A little history: Dr Harvey Cushing Wm. Bovie, PhD Electrosurgical Theory A few terms: Electrosurgery: application of a high-frequency electrical current to tissue to stop bleeding or to cut tissue. Ablation: removal of a layer of tissue Cautery: any application of heat to seal bleeding tissue Coagulation: formation of clot to seal bleeding tissue Desiccation: to dry-up (in the sense of removing fluid & blood) Eschar: dead, charred tissue Fulguration: use of sparking electrosurgery to desiccate tissue Ligature: tying or binding something tightly; sealing a vessel with ESU Electrosurgical units are radio frequency (RF) generators: Typically 450-500 kHz, but may be as high as 5 MHz (plastic surgery) higher frequency → finer cut & less ancillary damage The basic idea: ESU’s are RF generators “ESUs are little radio stations” Modulation of the RF for electrosurgical uses: Most usage is either ‘Cut’ or ‘Coag’ Typical power range: 0 - 300 watts Typical power range: 0 - 120 watts Cutting action 100% duty cycle Fulguration - highest voltage, lowest duty cycle. Higher voltage creates more heat, causing hemostasis. ‘Crest Factor’ or ‘Peak-to-Average Ratio’: Vpeak Crest Factor = VRMS ( eg, for a sine wave, CF = 1.41 pure DC would be 1.0) Crest Factor indicates the ‘quality’ of a waveform. A high CF indicates a less efficient or noisier waveform. Different tissues offer different impedances to RF: newer automatic ESU typical older ESU Basic Monopolar Electrosurgery: Bipolar mode cautery - (typical for neuro) (No need for a return pad) Current flows thru insulated forceps Typical power range: 0 - 70 watts RF Ablation: removal of a layer of tissue by use of localized RF (typical for heart, liver) Safety Issues in ESU’s: > External “second site” RF burns > Internal “second site” RF burns > RF interference on adjacent devices > Smoke plume > Fire Effective distribution of RF energy to the return pad Tissue is burned where desired, but not on exit Faulty contact of the return pad Tissue is burned where desired, and at the pad. BAD: Alternate Site Burns in a Basic Monopolar System BETTER: The Isolated Electrosurgical System Isolated system is deactivated if the return path is opened, but burns can still occur if there is a path to ground. BEST: the Return Electrode Monitoring (REM) system: Typical REM signal is 80 kHz @ ~10µA Return pad has two conductive plates, which are monitored by the ESU for continuity. aka ‘Contact Quality Monitoring’ Internal “second site” burns during endoscopy: Hazardous practices to be aware of: > “Buzzing” the hemostat: touching the active electrode to a hemostat (or several hemostats) clamped to tissue in order to save time. Can result in shocks or burns. > Wrapping the active lead wire around metallic instruments. > Stacking other medical electronics on or under the ESU. RF from the ESU can trigger or alter the function of other equipment. ESUs are the primary source of ignition for O.R. fires. O.R. personnel are expected to take appropriate precautions: - Eliminate the use of alcohol-based prep solutions - Minimize “fuel loading” (flammable materials on & near the site) - Minimize oxygen flooding around the surgical site. - Have a fire extinguisher within ready access. Smoke plume Smoke plume from electrosurgery is just as much a hazard to staff as is plume from lasers. - Gases and particulates are toxic and carcinogenic. OSHA and the AORN both encourage the routine use of smoke evacuators, high-filtration masks, and eye protection when using electrosurgical units. - Compliance has not been universal. Smoke-evacuation for ESU’s: older Valleylab current Valleylab Buffalo ‘ViroVac’ Megadyne ‘Vac Plus’ Variations on Electrosurgery: Argon Beam Coagulators - Essentially an enhanced ESU - still has cut, coag, bipolar - Use high voltage from the ESU to ionize a stream of Argon gas - Resulting plasma acts to provide a cleaner, wider coagulating effect Conmed’s Argon Beam Coagulator model 7500 Valleylab’s ‘Force Argon’ argon beam coagulator used with their Force-FX Variants on the ESU: Valleylab’s ‘Ligasure’ vessel-sealing system Proprietary Variants on Electrosurgery > Specific to a surgical procedure > Often use a higher frequency > 500kHz > Usually a surgeon’s preference > Usually use a unique disposable Arthrocare Corp: ‘Coblator II’ for ENT surgery Elmed 50-P: for Gynecological surgery Medtronic Corp: ‘Cardioblate’ for ablation of heart tissue Hologic Corp: ‘NovaSure’ for thermal ablation of the uterus http://www.novasure.com/info/novasure-and-heavy-periods/novasure-patient-animation.cfm Somnus: Somnoplasty (for snoring) Conmed’s “Hyfrecator” Low energy cautery, without a grounding pad Hyfrecator output modes: Bipolar mode Monopolar with return pad Monopolar without pad Variants on the ESU: The Harmonic Scalpel (Ethicon / Johnson & Johnson) -- NOT an electrosurgical unit -- Uses piezoelectric component to create an axial vibration (at ~56 KHz) at the surgical tip -- Use a variety of surgical probes and extensions specific to the surgical procedure -- Technically elegant; calibration pretty simple Testing ESU’s: (usually 500 Ω) Generic ESU tester – > Derives a small DC voltage from the RF from the ESU > DC value is proportional to the output power Functional Check: 1) Return Electrode Monitor - Measure the resistance from the REM connector to ground: should be >20M Ω. - For single conductor return electrodes, verify that the unit alarms and does not deliver power if the resistance across the REM leads is >10 Ω. - For “split pad” return electrodes, verify that the unit alarms and does not deliver power if the resistance across the REM leads is < 5 Ω or >150 Ω. (Depends on the model - check the manual!) Functional Check: 2) RF Power Output - Use your analyzer or external non-inductive resistors as appropriate load impedances for Bipolar, Cut and Coag modes, (typically 100Ω, 300Ω, and 500Ω). - Test the unit in the Cut, Coag, and Bipolar modes, at a low power and at maximum power. - 5 watts for the low end - maximums typically 300W for Cut, 120W for Coag 70W for Bipolar - Power readings should be ±5W or ±15% Functional Check: 3) RF Leakage (not 60 Hz current) - Configure the analyzer for RF Leakage - For any monopolar output, with appropriate load, RF leakage should be < 100mA (not µA!) - For the bipolar output, RF leakage should be < 60 mA. (Check the manual - some models allow 150mA) Thorough testing an ESU includes power output tests at a variety of load impedances, in order to simulate the variable loads in the different types of tissue encountered by the active electrode during surgery. Current ESU analyzers enable the user to test in each mode and power setting at several impedances sequentially. Functional Check: 4) Electrical Safety Check - per your department protocol and finally, Document ! - the ESU control number is entered in the surgical record by nursing staff for each surgery. If there is any “sentinel event”, your maintenance record can be used in a legal action. ESU Test Equipment - Fluke 454A (legacy) ESU Test Equipment - Fluke QA-ES ESU Test Equipment BC Group’s ESU-2300 Test setup with load resistors Typical Troubleshooting - Surgeons complain about poor output - Active lead wires increase resistance with age - Foot pedals fail from abuse - ESU signals cause interference on video displays - REM pad connectors break and become intermittent Major Players in: General Electrosurgery: - Valleylab - Conmed - Erbe Argon Beam Coags: - Valleylab - Conmed Harmonic Scalpels: - Ethicon - Olympus Valleylab Force 2 (legacy) Valleylab Force FX Valleylab switch for simple or split return pad Valleylab’s “Force Triad”: combines a Force FX with a Ligasure Valleylab Surgistat II Atmos RS 221 2.2MHz, 100W Entermed ESG -01-01-21: 4.0 MHz, 130W Conmed More information: Non-Valleylab ESU service website: www.servicingvalleylabgenerators.lefora.com Valleylab tech reference site: http://energysolutions.covidien.com/content/biomedconnect Nice history of electrosurgery: http://www.electrotherapymuseum.com/Museum.htm Very nice review of electrosurgery principles, safety issues, and surgical video: http://www.youtube.com/watch?v=ZeHNJSyrLPk