Attending to Affective Disorders in Primary Care : INTRODUCTION RESULTS
advertisement

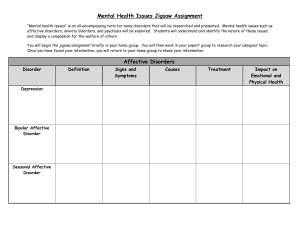
Attending to Affective Disorders in Primary Care : Medicate, Refer, or Both? APPLIED PSYCHOLOGY LABORATORY East Tennessee State University http://www.etsu.edu/apl/ Johnson City, Tennessee Druery R. C., Steffey, S. K., Miesner, M.T., & Dula C.S. INTRODUCTION RESULTS •It is known that patients with mental illness will more readily seek treatment from their primary care physician (PCP) than a mental health expert. Approximately 80% of treated patients will receive their treatment from a primary care physician (Strosahl, 1998). Data were subjected to a Chi Square. Mental Health Referrals differed as a function of Affective Disorders , X2 (2)=9.05, p <.001 Affective Disorders Noted in Chart vs. Mental Health Referral 60 • The National Comorbidity Survey ( NCS) and the NCS- replication reported having a 60% overlap between anxiety symptoms & Mental lifetime major depression disorder. Kessler et al. (1996) Health • Research indicates that only one third of patients in primary care are properly diagnosed as having a mood disorders. Up to 50% of the potentially effected may be incorrectly diagnosed (Munoz et al., 1994). Further research demonstrated 72% of the positive screeners sought professional help for the symptoms of mood disorders, only 8.4% were actually diagnosed with said disorder (Das et al., 2005). DISCUSSION Referrals No 50 40 No Yes 30 20 Yes None 50 0 Anxiety 30 7 Mood Disorder 31 7 Note: 26 patients were diagnosed with anxiety and mood disorders. 10 0 None Anxiety Mood Disorder Affective Disorders Noted Note: 6 of the 7 overall mental health referrals had both anxiety and mood disorders. LIMITATIONS Affective Disorders and Treatments Given • In 2006 Wagner, et al., demonstrated that primary care assessments, of those with anxiety disorders often failed to detect anxiety as the key problem, and subsequently, those with anxiety disorders reported longer delays in reaching specialist care (>9 years). 20 HYPOTHESES H1: It was hypothesized that mood disorders and anxiety are commonly recognized in primary care, with a positive correlation, but are rarely referred to a mental health expert. H2: When affective disorders are treated in primary care they are done so in a pharmacological manner using combinations of Selective Serotonin Reuptake Inhibitors (SSRI) or Tricyclic Antidepressants (TCA), Antipsychotics, and Benzodiazepines. H3: A significant amount of patients with an affective disorder will not be treated or referred to a mental health expert by their primary care physician, or PCP. None Anxiety Mood Disorder SSRI's TCA's 4 2 18 7 19 6 • There was no way to verify that the medical charts were complete in regards to the patients medical history. • The scope of this project limited us from accurately gathering the type of affective disorder as well as the severity of the disorder due to medical chart review nature. 18 16 14 None Anxiety Mood Disorder 12 Treated Patients 10 8 6 Note: Some patients were given multiple medications. 4 2 0 SSRI's TCA's Antipsychotics Medication Prescribed by PCP Future studies are planned, in which multiple interventions will be tested. Interventions such as education to physicians about affective disorders, providing brief assessment tools, and strategies on how to refer their patients with affective disorders to mental health providers in integrated primary care. Das, A. K., Olfson, M., Gameroff, M. J., Pilowsky, D. J., Blanco, C., Feder, A., et al. (2005). Screening for bipolar disorder in a primary care practice. JAMA : the journal of the American Medical Association, 293, 956-63. Noted in Chart but Untreated with no Referral Noted in chart but untreated/ no referral 15 Untreated 10 Patients Without Referrals 5 IMPLICATIONS & FUTURE DIRECTIONS SELECTED REFERENCES Benzodiazepines METHOD Method: Data was collected using 8 undergraduates trained to review medical charts in the integrated primary care practice. Information that was obtained relative to affective disorders was the treating physician, first notation of an affective disorder, method of treatment, any medications which could be used (including off label uses) to treat the particular affective disorder, and if a mental health referral occurred. • Data was only collected from one primary care site. Antipsychotics Benzodiazepines 1 2 5 6 8 4 20 Participants : 100 medical charts were reviewed at a rural family medicine clinic. • One of the problems in detecting a mental health disorder in primary care is the ability for a patient to effectively communicate with their PCP. This may be in part to many patients having trouble overcoming the negative stigma associated with receiving mental health treatment. The findings of this pilot study concerns the amount of affective disorders noted, and additionally, how these disorders were handled. • During chart review, it was found that when a possible serious affective disorder was noted often no record of a referral to a mental health expert was made by a PCP. While impossible to draw definitive conclusions from the pilot study regarding how well affective disorders are being treated by PCP’s, it is possible to conclude that interventions in primary care is necessary to help physicians detect these disorders and treat them more effectively . Kessler, R.C, Nelson, C.B., McGonagle, K.A., Liu, J., Swartz, M., Blazer, D.G., (1996). Comorbitidy of DSM-III-R major depressive disorders in the general population: results from the US National Comorbidity Survey. Br. J. Psychiatry 17-30 Suppl. Anxiety 11 Mood Disorder Muñoz, R. F., Hollon, S. D., McGrath, E., Rehm, L. P., & VandenBos, G. R. (1994). On the AHCPR Depression in Primary Care guidelines: Further considerations for practitioners. American Psychologist, 49, 42-61. 17 Strosahl, K. (1998). Integrating behavioral health and primary care services: The primary mental health care model. In A. Blount (Ed.), Integrated primary care: The future of medical and mental health collaboration.(pp 139-166). New York: W.W. Norton & Co., Inc. 0 Anxiety Mood Disorder Affective Disorders Noted Note: Some patients are being represented more than once due to multiple diagnoses, treatments, and / or misdiagnosis. CONTACT: Ryne_Druery@yahoo.com or Chris S. Dula, dulac@etsu.edu Wagner, Renate; Silove, Derrick; Marnane, Claire; Rouen, David; Journal of Anxiety Disorders, Volume 20(3), 2006. pp. 363-371.