Parent Child Interaction Therapy John Paul Abner, Ph.D. Milligan College
advertisement

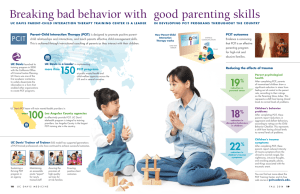
Parent Child Interaction Therapy John Paul Abner, Ph.D. Milligan College ETSU Center of Excellence for Children in State Custody Copyright 2011, PCIT International What is Parent-Child Interaction Therapy? PCIT Parent-Child Interaction Therapy (PCIT) Empirically supported treatment for young children (2.5 -7) with disruptive behavior Developed by Dr. Sheila Eyberg © Gurwitch, Funderburk, & Nelson Treatment Outcome Research and Controlled Trials Significant reductions in noncompliance and behavior problems Generalization to home and school Maintenance of gains up to six years after treatment(maximum follow up time to date) Generalization to untreated siblings Changes in parents’ interactional style © Gurwitch, Funderburk, & Nelson How does PCIT work? PCIT Balances Two Factors… 1. Positive Interaction with the Child Increase positive attention Decrease negative attention 2. Consistent Limit Setting Consistency Predictability Follow-Through © Gurwitch, Funderburk, & Nelson What makes PCIT unique among parent training programs? PCIT: Core Features Active coaching of parent with their child Grounded in developmental theory Emphasis on restructuring interaction patterns Assessment-driven Not time-limited Empirically supported COACHING PCIT: Coaching Allows therapist to: Better understand the parent-child interaction Change the interaction, not specific behavior problems Give parents specific and immediate feedback on their use of the skills Correct errors immediately Praise appropriate behaviors Assess readiness to move on to next phase or graduate PCIT: Coaching Two-way Mirror Mom Child Bug-inthe-Ear PCIT: Coaching Two-way Mirror Coach GROUNDED IN DEVELOPMENTAL THEORY Based on Developmental Theory Nurturance and limits both necessary for healthy outcomes PCIT draws from attachment and social learning theories to achieve authoritative parenting NOT TIME-LIMITED Not time-limited • • Treatment continues until family meets graduation criteria Average 14-16 weeks, could be shorter or longer Completion = Success ASSESSMENT DRIVEN EMPIRICALLY SUPPORTED PCIT: A Model Program Society of Clinical Child and Adolescent Psychology, APA Division 53 (www.effectivechild therapy.com) The National Child Traumatic Stress Network (SAMHSA, 2005; http://www.nctsn.org) Chadwick Center for Children and Families (http://www.chadwickcenter.org) National Crime Victims Research and Treatment Center (U.S. Department of Justice; http://musc.edu/ncvc) The California Evidence-Based Clearinghouse for Child Welfare (2006; http://www.cebc4cw.org) Youth Violence: A Report of the Surgeon General (www.surgeongeneral.gov/library/youthviolence) Efficacy of PCIT Two well-conducted randomized trials Participants United Sates (Schuhmann et al., 1998) Australia (Nixon et al., 2003) Preschool age (3 to 6 years) Disruptive behavior disorders Primarily Caucasian No significant developmental/cognitive delay Improvements in (compared to waitlist) Child behavior Parenting practices and stress ECBI Intensity Scale Efficacy of PCIT p < .001 d = 1.40 (Schuhmann et al., 1998) Cohen’s d PCIT Effect Size (Rosenthal et al., 1990) (Connor et al., 2002) (Schuhmann et al., 1998) Efficacy of PCIT Maintenance Short-term (1 to 2 years; Eyberg et al., 2001; Nixon et al., 2004) Long-term (3 to 6 years; Boggs et al., 2004; Hood & Eyberg, 2003) Generalization Siblings (Brestan et al., 1997; Eyberg & Robinson, 1982) Preschool classrooms (Bagner et al., 2010; Funderburk et al., 1998; McNeil et al., 1991) Meta-analytic work PCIT components associated with larger effect sizes (e.g., active coaching, teaching parents positive interactions and time out; Kaminski et al., 2008) Comparable to Triple P (Thomas & Zimmer-Gembeck, 2007) The PCIT Evidence Base: Randomized Controlled Trials 1998 Florida Disruptive Behavior Disorders (DBD) Schuhmann, Foote, Eyberg, Boggs, & Algina 2003 Australia Disruptive Behavior Disorders Nixon, Sweeney, Erickson, & Touyz 2004 Oklahoma Physically Abusive Parents Chaffin, Silovsky, Funderburk, et al. 2006 Puerto Rico Attention Deficit Hyperactivity Disorder Matos, Torres, Santiago et al. 2007 Florida Comorbid Mental Retardation and DBD Bagner & Eyberg 2010 San Diego Mexican-American Children with DBD McCabe & Yeh 2010 Rhode Island 2010 Oklahoma Toddlers Born Premature with DBD Bagner, Sheinkopf, Vohr, & Lester Abusive and Neglectful Parents Chaffin, Funderburk, et al. Autism? Copyright May 2008 Sheila Eyberg REV May Relationship Enhancement: Child Directed Interaction (CDI) Goals of CDI Enhance relationship between parent and child Reduce frustration/anger Improve social skills Improve self-esteem Improve organization and attention Improve speech/language skills © Gurwitch, Funderburk, & Nelson MAIN RULE OF CDI: LET THE CHILD LEAD THE PLAY CDI: Features Special Time The Do’s and Don’ts of Special Time Tactical Ignoring Coaching to Criteria © Gurwitch, Funderburk, & Nelson CDI: Special Time Parents learn to set up a 5-minute “special time” with their child in which they practice the CDI skills to enhance their relationship Therapists help parents problem solve: Time Place Toys to use © Gurwitch, Funderburk, & Nelson CDI: Don’t skills Lead the play Give commands Ask questions Criticize © Gurwitch, Funderburk, & Nelson CDI: Do skills Praise Reflect Imitate Describe Enjoy © Gurwitch, Funderburk, & Nelson CDI: Handling Misbehavior Ways to handle annoying, obnoxious behavior during Special Time Returning attention when positive behavior occurs Addressing aggressive or destructive behavior © Gurwitch, Funderburk, & Nelson CDI: Mastery Criteria Determines when family may be ready to move on to the next phase 10 Labeled Praises 10 Behavior Descriptions 10 Reflections 3 or fewer total of Commands, Questions, & Critical statements © Gurwitch, Funderburk, & Nelson Discipline and Minding Skills: Parent-Directed Interaction (PDI) PDI: Features Giving good directions Contingent consequences Gradual generalization from clinic minding exercises to “real life” discipline Planned responses to Refusal to stay in timeout Impulsive, destructive, and dangerous behaviors Behavior disruptions in public settings © Gurwitch, Funderburk, & Nelson PDI: Time-Out What is time-out Setting up time-out place How long Getting to time-out Staying in time-out Getting out of time-out Back-ups After time-out © Gurwitch, Funderburk, & Nelson PDI: Mastery Criteria At least 75% of commands given are effective commands At least 75% correct follow through © Gurwitch, Funderburk, & Nelson PCIT: Graduation Criteria Caregivers’ CDI skills at mastery levels Caregivers’ PDI skills at mastery levels Child’s behavior rated as within ½ standard deviation of mean Caregivers report feeling comfortable with using the skills © Gurwitch, Funderburk, & Nelson PCIT: Graduation Review progress (use summary sheet, ECBIs, tapes, etc) Lots of praise Schedule booster or follow-up as needed Managing future behavior problems © Gurwitch, Funderburk, & Nelson QUESTIONS?