W9, A MEDICINAL PLANT OF THE EASTERN JAMES
advertisement

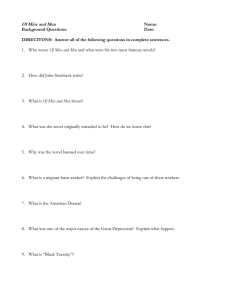
W9, A MEDICINAL PLANT OF THE EASTERN JAMES BAY CREE, MOBILIZES L6 MUSCLE GLUT4 TRANSPORTERS AND EXERTS ANTI-OBESITY AND ANTIDIABETIC EFFECTS IN VIVO. Hoda M. Eid 1,3,4, Antoine Brault 1,3,4, Meriem Ouchfoun 1,3,4, Farah Thong 5, Diane Vallerand 1,3,4, Riya Ganguly5, John T. Arnason 2,4, Gary Sweeney 5, Pierre S. Haddad 1,3,4 1 Natural Health Products and Metabolic Diseases Laboratory, Dept. of Pharmacology, Université de Montréal, Montreal, QC, 2 Phytochemistry, Medicinal Plant and Ethnopharmacology Laboratory, Dept. of Biology, University of Ottawa, Ottawa, ON, 3 The Institute of Nutraceuticals and Functional Foods (INAF), 4 Canadian Institutes of Health Research Team in Aboriginal Antidiabetic Medicines and Montreal Diabetes Research Center,5 Dept. of Biology, York University, Toronto, ON ABSTRACT W9 has been identified among species used by the Cree of Eeyou Istchee of northern Quebec to treat symptoms of diabetes. In a previous study, the ethanol extract of W9 enhanced glucose uptake in C2C12 muscle cells via stimulation of AMP-activated protein kinase (AMPK) pathway. In this study, we investigated the effect of this product on the translocation of insulin-sensitive GLUT4 transporters in skeletal muscle cells in culture. Treatment of L6 myotubes with W9 for 18 h significantly increased glucose uptake and GLUT4 translocation to the cell membrane. W9 increased phosphorylation of AMPK and P38 MAPK with no indication of increased phosphorylation of Akt. To validate the effect of W9 in vivo, the extract (1% in drinking water) was administered to KKAy mice for 10 days. Glycemia and fluid intakes were significantly reduced by W9. Moreover, W9treatment increased levels of GLUT4 content in skeletal muscle, stimulated the phosphorylation of ACC and increased the levels of PPAR-α in the liver of KKAy mice. Administration of W9 to normal C57BL/6 had no effect on blood glucose levels. The results of the present study confirm the potential of W9 for the prevention and treatment of diabetes. GLUT Family of Proteins Nature Reviews Molecular Cell Biology 3, 267-277 (April 2002) Name Tissue distribution Insulin Function sensitivity GLUT1 Ubiquitous, erythrocytes and brain No Basal glucose transport, transport across blood-brain barrier GLUT2 Liver, pancreatic β-cells, intestine, kidney No Intestinal absorption, renal re-absorption, pancreatic and hepatic control of glucose homeostasis GLUT3 Widely distributed in human tissues, restricted to brain No in other species. Immune cells. Glucose transport into neurons in brain, basal transport in many human cells. GLUT4 Skeletal muscle, cardiac muscle, adipose tissue Yes Insulin-dependent glucose transport. GLUT5 Intestine, testes, kidney. No Fructose transport. GLUT6 Leucocytes, spleen, brain. No n. d. GLUT7 Apical membrane of small and large intestine No Exhibits a low level of transport activity for fructose and glucose. GLUT8 Brain, heart Yes Role in neuronal proliferation and heart atrial activity. GLUT9 Liver, kidney, intestine No Regulator of uric acid liver. GLUT10 Liver, pancreas No n. d. GLUT11 Different tissue types No Glucose, fructose transport, main substrate has not been identified. GLUT12 Heart, prostate, musle, small intestine, WAT Yes Glucose homeostasis. GLUT13 Brain No Myoinositol transporter. GLUT14 Testis No Most likely a glucose transporter. Effect of Insulin on GLUT4 GLUT4 and Type 2 Diabetes ● GLUT4 is responsible for facilitating the transport of glucose into the cells in response to insulin. ● Type 2 diabetes is associated with mutations and reduced expression of GLUT4. As a result, glucose transport is significantly impaired. ● Drugs enhancing GLUT-4 translocation and/ or expression will provide novel treatments for Type 2 diabetes. Type 2 Diabetes ● Type 2 Diabetes is a worldwide epidemic (220 million) ● Canadian aboriginal populations : Its prevalence is 3-4 times the canadian average Its worsened by genetic predisposition, sedintary life and poor compliance to western Rx The need for culturally-adapted alternative : plants from their Traditional Medicine ● Ethno-botanical study previously identified 17 plants for the treatment of Type 2 diabetes ● In a previous study, the ethanol extract of W9 enhanced glucose uptake in C2C12 muscle cells via stimulation of AMP-activated protein kinase (AMPK) pathway OBJECTIVES ● Evaluate the downstream signalling of W9 ● Study the anti-diabetic activity of W9 in vivo Figure 1: Insulin and non-insulin dependent pathways regulating glucose transport Inhibition of mitochondrial respiration ACC Mitochondria METHODS In vitro studies • We used L6 skeletal muscle cells wild type (WT) and transiently transfected with GLUT4myc to measure : Glucose uptake : for the specific uptake of 2-deoxy-D- glucose. GLUT 4 translocation : using antibody-coupled colorimetric assay, O-phenylenediamine dihydrochloride (OPD), and anti-myc antibody. • We evaluated downstream signalling using western blot analysis: Insulin-dependent pathway (phospho-Akt) Insulin-independent pathway (phospho-AMPK, phospho-p38 MAPK and phospho-ACC) METHODS In vivo studies Animal models : • Study # 1 : Diabetic KKAy mice Group 1 mice received drinking tap water Group 2 mice were administered with 1% W9 in drinking water • Study# 2 : Normal C57BL/6J mice Group 1 mice received drinking tap water Group 2 mice were administered with 1% W9 in drinking water Parameters measured : • Blood parameters : During study (every 2 days): glycemia and fluid intake were measured Post sacrifice: toxicity, lipid profile were evaluated Liver steatosis was evaluated histologically • Western blot: PPAR-a GLUT4 RESULTS W9 stimulates glucose uptake in L6 rat muscle cells by inducing GLUT 4 translocation to the membrane Glucose Uptake GLUT 4 translocation (OPD assay) (radioactive assay) Fold increaae in GLUT4 translocation * 3 H-Deoxyglucose Uptake (% of DMSO) 180 160 140 120 100 80 60 40 20 0 2 (% of DMSO) * 200 * * Insulin Insulin W9 V.vitis 1 0 DMSO DMSO Insulin Insulin * : P<0.05 as compared to DMSO W9 V.vitis DMSO DMSO W9 stimulates AMPK pathway in L6 muscle cells, but not the Insulin pathway AMPK pathway Insulin pathway phospho-AMPK phospho-Akt phospho-p38 MAPK b-Actin b-Actin W9 significantly decreases glycemia in diabetic KKAy mice but had no effect in normal lean mice C57BL/6J KKAy mice (Study #1) C57BL/6J mice (Study #2) 35 Control 14 V.vitis 30 Control V.vitis 12 20 * 15 10 5 Glycemia (mmol/L) Glycemia (mmol/L) 25 10 8 6 4 2 0 0 -2 -1 0 1 2 3 4 5 6 7 8 9 10 -2 11 0 1 2 3 4 5 Days Days Control * : P<0.05 as compared to control -1 W9 6 7 8 9 10 11 W9 significantly decreases fluid intake glycemia in diabetic KKAy and normal C57BL/6J mice KKAy mice (Study #1) C57BL/6J mice (Study #2) 300 300 Control V.vitis 250 200 150 * * 100 50 * Cumulative fluid intake (mL) 250 Cumulative fluid intake (mL) Control V.vitis 200 150 100 * 50 0 0 -2 -1 0 1 2 3 4 5 6 7 8 9 10 -2 11 0 1 2 3 4 5 Days Days Control * : P<0.05 as compared to control -1 W9 6 7 8 9 10 11 W9 is not toxic, significantly decreases plasma triglycerides, but only tends to lower plasma insulin level in KKAy mice from study # 1 Control W9 AST (IU/L) 107.7 ± 14.5 92.0 ± 11.7 ALT (IU/L) 64.5 ± 8.7 56.0 ± 10.4 LDH (IU/L) 108.8 ± 9.4 71.5 ± 18.0 1280.7 ± 340.2 832.7 ± 219.9 112.4 ± 11.1 77.0 ± 7.9* Triglycerides (mmol/L) 4.5 ± 0.8 2.9 ± 0.5* Cholesterol (mmol/L) 2.3 ± 0.14 2.12 ± 0.19 HDL (mmol/L) 1.07 ± 0.09 1.09 ± 0.11 LDL (mmol/L) 0.5 ± 0.2 0.5 ± 0.0 Insulin (ng/mL) 35.32 ± 8.48 18.98 ± 4.22 Leptin (ng/mL) 27.12 ± 1.7 23.9 ± 0.99 Adiponectin (ug/mL) 18.17 ± 2.44 18.00 ± 2.2 Creatinine (IU/L) Alkaline phosphatase (IU/L) Treatment of KKAy diabetic mice with W9 improved liver steatosis significantly Steatosis$ Groups 0 1 2 3 Control 7 1 1 0 5 W9 7 3 1 0 3 Chi square $ n P < 0.05 Liver steatosis was evaluated histologically in control and W9 treated KKAy mice (Study # 1) W9 increased the levels of GLUT4 in skeletal muscles and those of PPAR-α in livers from diabetic KKAy mice Control KKAy mice (Study #1) W9 GLUT4 PPAR-a SUMMARY W9 treatment ● In vitro studies: ● Increased glucose transport in L6 skeletal muscle cells to levels similar to those of insulin. Increased GLUT4 translocation in L6 muscle cells. Did not stimulate phosphorylation of Akt (insulino-dependent ). Increased phosphorylation of AMPK, p38 MAPK and ACC. In vivo studies: Decreased glycemia in diabetic KKAy mice (p< 0.05). Decreased cumulative fluid intake in diabetic KKAy and normal C57BL/6J (p< 0.05). Decreased plasma triglyceride levels by 36% (p< 0.05). Attenuated liver steatosis. Increased GLUT4 content in muscle and PPAR-a content in liver of diabetic KKAy mice. ACKNOWLEDGEMENTS Study conducted in collaboration with the Cree Nation of Mistissini