Online Depository Factors Influencing Duration of Exposure with Symptoms
advertisement

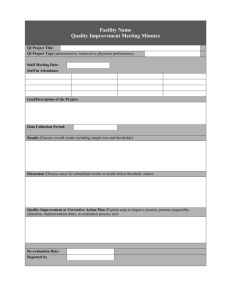
1 Online Depository 2 3 Factors Influencing Duration of Exposure with Symptoms 4 and Direct Costs of Occupational Asthma 5 6 David Miedinger, M.D., Jean-Luc Malo, M.D., Herberto Ghezzo, Ph.D. 7 Jocelyne L’Archevêque, R.T., Maria-Victoria Zunzunegui, Ph.D. 8 9 Methods 10 11 This is a cross-sectional study investigating subjects who claimed compensation for 12 occupational asthma (OA) at the Workers’ Compensation Board of Quebec 13 (Commission de la santé et sécurité du travail du Québec; CSST) between the years 14 2004 to 2006. Subjects were exposure-free from the offending allergens causing OA 15 for two years or more and were evaluated by two of the four Quebec CSST medical 16 committees in Montreal (Montreal Chest Institute and Hôpital du Sacré-Coeur) for 17 permanent disability indemnity. In Québec, all subjects who claim compensation for 18 OA undergo specific inhalation testing for evaluation. All claimants scheduled for 19 evaluation by the committees were asked to participate in this study on a voluntary 20 basis. We added questions regarding current employment status, participation in past 21 rehabilitation programs and other socioeconomic factors as well as validated 22 psychological and quality-of-life questionnaires to in our investigation. Subjects were 23 assured that the medical committee would not be informed of their acceptance or 24 refusal to participate in this study nor of the results of these tests. Subjects were 25 granted compensation to cover expenses like loss of salary and transportation and/or 26 parking fees. All study subjects gave written consent for their participation. The 27 research protocol was approved by the Research Ethics Committee of our hospital. 28 The data is reported in accordance with STROBE guidelines[1]. 29 All subjects answered a questionnaire on chest and upper airway symptoms, 30 medication use, home allergen exposure and tobacco consumption. Furthermore, 31 subjects were asked to fill out a questionnaire about the type of agent causing the 32 occupational asthma and if in fact, they were still being exposed to it. A questionnaire 33 about socioeconomic outcomes like current employment, salary, schooling, country 34 of origin, number of dependent children and family members relying on the 35 household income, information about the Workers’ Compensation Board’s Social 36 Rehabilitation Program (job education, full or partial participation in the Job Education 37 Program, use of the employment agency) and the WCB records were consulted to 38 obtain information concerning costs for compensation for loss of income and 39 compensation for functional impairment. 40 The number of years of exposure in the workplace with symptoms before 41 removal from exposure (YWS) was determined by consulting the Workers’ 42 Compensation Board file. We recorded the time period as noted by the local medical 43 committee in the initial official report. The cut-off values for low income have been 44 issued by Statistics Canada and take into account the individual’s place of residency 45 and the number of dependent family members[2]. We defined low income as having 46 an income at diagnosis that was less than 110% of the cut-off value for low income 47 according to the definition laid out by Statistics Canada. 48 All subjects underwent spirometry according to ATS guidelines before and 49 after receiving bronchodilator medication to determine forced expiratory volume for 50 one second (FEV1) and forced vital capacity (FVC)[3]. Reference values for FEV1 51 and forced vital capacity (FVC) were calculated according to the formulas derived by 52 Knudson and co-workers[4]. Methacholine challenge tests were performed according 53 to a previously published protocol[5]. In brief, subjects inhaled methacholine in 54 increasing concentrations using a Wright’s nebuliser (output=0.14 mL*min -1; Aerosol 55 Medical Ltd., Colchester, UK) with a maximum concentration of 32mg*mL -1. The test 56 was ended when a significant fall of FEV1 greater or equal to 20% compared to the 57 baseline measurement occurred. Normal responsiveness was set at a provocative 58 concentration of methacholine causing a 20% fall (PC20) in FEV1 of greater than 16 59 mg*mL-1[6]. Changes in PC20 were considered significant when there was a 3.2-fold 60 or greater difference from the value obtained at the time of diagnosis[7]. 61 Skin prick tests were performed to assess atopic status according to the 62 method described by Pepys[8]. For sputum induction, subjects inhaled increasing 63 concentrations (3%, 4%, and 5%) of hypertonic saline and the samples were 64 processed according to a previously published protocol[9, 10]. 65 The asthma severity at diagnosis, at re-evaluation and the proportion of 66 permanent disability that was allocated were calculated according to the Quebec 67 Workers’ Compensation Board Scale for OA: 0% low severity, 100% Maximum 68 severity)[11]. This scale incorporates three factors in the same way as the one 69 proposed by the American Medical Association[12]: level of bronchial calibre, degree 70 of bronchial responsiveness and need for medication to control asthma [13]. We 71 estimated the change in asthma severity by substracting the score at re-evaluation 72 from that at diagnosis. For some analysis we dichotomized the data by using a cut-off 73 of 18%. This severity reflects mild obstruction (FEV1%predicted 71-85%), mild 74 bronchial hyperresponsiveness (PC20 2-16 mg*mL-1) and regular of if needed 75 bronchodilatator use. 76 We consulted the participant’s file at the Québec Workers’ Compensation 77 Board to determine the compensation costs for OA. The compensation for loss of 78 income and compensation for functional impairment as well as total costs are 79 reported in this study. Compensation for loss of income corresponds mainly to 80 compensation for lost salary during the rehabilitation period (up to two years) after a 81 worker is removed from the workplace harbouring the offending work agent. 82 Compensation for functional impairment is allocated at the time of re-evaluation by 83 the orkers’ Compensation Board, i.e., about two years after diagnosis and after 84 subsequent removal from the workplace and is calculated according to the orkers’ 85 Compensation Board Scale for OA. 86 87 Results 88 89 90 Change of objective measurements between diagnosis and re-evaluation There was no significant change in spirometric results between diagnosis and 91 re-evaluation. 50 subjects (83%) underwent methacholine challenge testing at 92 diagnosis and at re-evaluation. The proportion of subjects with hyperresponsiveness 93 (PC20≤16mg/ml) decreased significantly (at diagnosis 57 (98%) vs. 36 (69%), 94 p<0.001). When considering the change in airway responsiveness, 35 (70%) had an 95 increase of ≥2-fold, 10 (20) a increase <2-fold and 5 (10) a decrease in PC20. Thirty- 96 four subjects (57%) were able to produce interpretable induced sputum 97 measurement at diagnosis and 46 (77%) at re-evaluation. Eosinophil, neutrophil and 98 total cell count did not change significantly between diagnosis and re-evaluation. 99 The proportion of those receiving no treatment for asthma, being on treatment with 100 only a short-acting bronchodilator, being on inhaled steroids and the dose of inhaled 101 steroids administered did not change significantly between diagnosis and re- 102 evaluation. There was an increase in the proportion of subjects inhaling long-acting 103 bronchodilators (12 (20%) at diagnosis vs. 25 (42%) at re-evaluation, p=0.004). The 104 distribution of subjects according to smoking status remained unchanged, but one 105 smoker had stopped smoking and one former smoker had resumed smoking. 106 Overall, the amount of improvement in asthma severity in this cohort was only 107 moderate (improvement 3.1% mean ±14.3%, 5% median (Q1;Q3:-2.0%;9.5%). 108 Sixteen subjects (27%) saw a worsening of their asthma, in 29 subjects (48%) 109 asthma severity remained unchanged or the improvement was less than 9% and 15 110 subjects (25%) experienced an improvement of 10% or more at re-evaluation. 111 We classified subjects according to the results of the methacholine challenge 112 test at re-evaluation as either hyperreactive or normoreactive. Those classified as 113 hyperreactive had a significantly higher hyperreactivity to methacholine at diagnosis, 114 a higher asthma severity score at re-evaluation (16% (Q1;Q3: 13%;28%) vs. 11% 115 (Q1;Q3: 8%;20%), p=0.041), longer exposure in the workplace with symptoms before 116 removal from exposure (2.6 years (Q1;Q3: 0.5 years;7.8 years) vs. 0.6 (Q1;Q3: 0.1 117 years;1.3 years), p=0.040) and were more often from a higher income bracket than 118 CAD 30,000.— (25 (78%) vs. 7 (22%), p= 0.050). 119 120 References 121 122 1. von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke 123 JP. Strengthening the Reporting of Observational Studies in Epidemiology 124 (STROBE) statement: guidelines for reporting observational studies. BMJ 2007: 125 335(7624): 806-808. 126 2. 127 Statistics Canada ISD, ed., 2006. 128 3. 129 AmJRespirCrit Care Med 1995: 152(3): 1107-1136. 130 4. 131 maximal expiratory flow-volume curve with growth and aging. AmRevRespirDis 1983: 132 127(6): 725-734. 133 5. 134 inhaled histamine: a method and clinical survey. ClinAllergy 1977: 7(3): 235-243. 135 6. 136 concentrations of methacholine that cause 6% and 20% changes in forced expiratory 137 volume in one second in a normal population. AmRevRespirDis 1983: 128(1): 8-11. 138 7. 139 in asthma: reproducibility and sensitivity of different indices to assess response. 140 Thorax 1983: 38(7): 516-522. 141 8. 142 1972: 65(3): 271-272. 143 9. 144 Gleich GJ, Dolovich J, Hargreave FE. Indices of airway inflammation in induced Low Income Cut-offs for 2005 and Low Income Measures for 2004. In: Standardization of Spirometry, 1994 Update. American Thoracic Society. Knudson RJ, Lebowitz MD, Holberg CJ, Burrows B. Changes in the normal Cockcroft DW, Killian DN, Mellon JJ, Hargreave FE. Bronchial reactivity to Malo JL, Pineau L, Cartier A, Martin RR. Reference values of the provocative Dehaut P, Rachiele A, Martin RR, Malo JL. Histamine dose-response curves Pepys J. Skin tests for immediate, type I, allergic reactions. Proc R Soc Med Pizzichini E, Pizzichini MM, Efthimiadis A, Evans S, Morris MM, Squillace D, 145 sputum: reproducibility and validity of cell and fluid-phase measurements. 146 AmJRespirCrit Care Med 1996: 154(2 Pt 1): 308-317. 147 10. 148 Dolovich J, Hargreave FE. Spontaneous and induced sputum to measure indices of 149 airway inflammation in asthma. AmJRespirCrit Care Med 1996: 154(4 Pt 1): 866-869. 150 11. 151 of occupational asthma. EurRespirJ 1994: 7(5): 969-980. 152 12. 153 Impairment. In: Cocchiarella L, Andersson GBJ, eds. American Medical Association, 154 Chicago IL, 2001; pp. 102-104. 155 13. 156 aspects, compensation aspects, and evaluation of impairment/disabilitiy. In: 157 Bernstein IL, Chan-Yeung M, Malo JL, Bernstein DI, eds. Asthma in the Workplace. 158 Taylor & Francis, New York, 2006; pp. 319-351. 159 160 Pizzichini MM, Popov TA, Efthimiadis A, Hussack P, Evans S, Pizzichini E, Dewitte JD, Chan-Yeung M, Malo JL. Medicolegal and compensation aspects American Medical Association. Guides to the Evaluation of Permanent Bernstein IL, Keskinen H, Blanc PD, Chan-Yeung M, Malo JL. Medicolegal