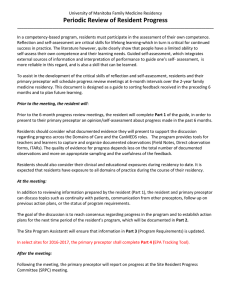
The Six-Step Preceptor
advertisement

The Six-Step Preceptor Peter DeBlieux, MD, LSUHSC EM Director of Faculty and Resident Development, pdebli@lsuhsc.edu “We are honored not for how tall we stand, but for how often we bend to help, comfort and teach”- Freemason Quote Six Steps I. A. B. C. D. E. F. Get a commitment Probe for supporting evidence Teach general rules Reinforce what was done correctly Correct mistakes Praise again with a plan Making a commitment to: work-up, diagnosis, or therapeutic plan II. III. Encourages information processing Identifies teaching opportunities or not… No commitment is a lost teaching opportunity-it is your cue to say. “What do you think is going on?” “What tests do you think are indicated?” “What is your goal for this patient encounter?” Enables the preceptor to assess the resident’s needs as a learner List other statements or hints for obtaining a commitment Probe for supporting evidence linked to the commitment IV. Identifies the process that is linked to the commitment Helps identify what the resident does and does not know Use nonjudgmental questioning “What led you to that diagnosis, those diagnostic studies, those treatment choices?” “What other diagnosis did you consider and what kept you from those choices?” Should avoid the sense of “grilling”, thinking out-loud should be encouraged What are other ways to seek and understand the resident’s thought process Focus on teaching generalities, avoiding specifics-if possible Instruction is more likely to be retained and transferred as a generality, avoiding facts and linking principles Avoid idiosyncrasies and anecdotes Offer critical pathways, consensus statements-utilizing expert sources-look it up together V. “Wrist injury coupled with a normal radiograph should be treated as a possible scaphoid fracture if snuff box tenderness is present. All soft tissue injuries should be treated with rest, ice, compressions, elevation, and NSAIDS” “I have never seen one of these rashes before… Let’s call dermatology or look through the atlas to figure out what this may be.” Describe other ways to stress generalized teaching points. Reinforce what is done correctly- Catch the resident doing something right VI. To encourage repetition of appropriate actions, praise them Positive feedback establishes professional self esteem Be specific-avoid compliments such as “You were great today!” Instead try“I like the way you professionally handled that difficult patient who demanded narcotics for his contused hand” “It was to the patient’s benefit that you considered her income and other medications prior to prescribing antibiotics in managing her acute bronchitis” “Your documentation of serial neuron exams in this head injured patient paints an excellent picture” Describe some ways you can catch residents doing something right in their presentations or write ups Correct mistakes VII. Public praise and private negative feedback Immediacy is best and a full story is helpful Ask the resident to critique their own performance first-an insight gauge Avoid judgmental generalized statements- “That whole case was handled like a third year medical student” “You idiot, never-ever care for a patient in my ED” Avoid this maneuver at the patient’s bedside-if at all possible “The patient with crushing chest pain in the monitor cubicle is signing out AMA after your exam-why?” “I called you into my office to discuss your heated, public argument with our consultant-is there a better way to handle such encounters?” “AHA no longer recommends administration of prophylactic lidocaine to uncomplicated AMIs-can you think of any reasons for this?” Praise again with a plan Complete the feedback sandwich- Praise-Correct-Praise. Be specific Get a commitment to reflect or review material that relates to this case later “I want you to look up the top five causes of…” “When you get home think about how your interactions with your patient led to success in this case” Reference: Neher JO, Gordon KC, Meyer B, Stevens N. A Five-Step “Microskills” Model of Clinical Teaching. J Am Board Fam Pract 1992:5:419-24