New Orleans EMS Airway Lecture Series: Lecture 1 Predicting the Difficult Airway
advertisement

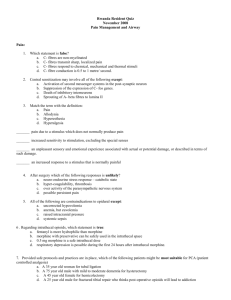
New Orleans EMS Airway Lecture Series: Lecture 1 Predicting the Difficult Airway Jeffrey M. Elder, M.D. Deputy Medical Director When To Intubate? • Failure to maintain/protect the airway – Required for successful oxygenation and ventilation – Reflexes avoid aspiration – Clear vocal communication is a good measure for airway protection/patency – Absence of a gag reflex not sensitive or specific as indicator for the need of an airway (swallowing) • Swallowing requires sensing the presence of pooled material and complex muscular actions to swallow – Spontaneous respirations ≠ airway protection When To Intubate? • Failure of Ventilation or Oxygenation – Supplemental oxygen not effective: ARDS – Respiratory fatigue/failure: Asthma – Can be reversible: Opioid overdose When To Intubate? • Anticipated Clinical Course – Deterioration of the critically ill – Patient is exposed to a period of increased risk: • Long transport time, air evacuation, etc. – Requires clinical gestalt • Examples: – Head injury/combative – Expanding hematoma Approach to Evaluating the Airway • Ask a question: What is your name? – Response can tell you about airway and neurological status – Normal voice, ability to inhale and exhale in a manner required for speech, comprehending the question – Only tells you about 1 moment in time – If unable to phonate properly: perform a detailed assessment of the airway Approach to Evaluating the Airway • Examine Mouth and Oropharynx – Bleeding – Swelling of Mouth or Uvula – Any abnormality that would interfere with the passage of air • Examine Mandible and Central face integrity Approach to Evaluating the Airway • Examine the Anterior Neck, Larynx, and Trachea: – Palpate for subcutaneous air • Tracheal injury, pulmonary injury, esophageal rupture, gas forming infections • Monitor the Respiratory Pattern – Stridor = upper airway obstruction Approach to Evaluating the Airway • Observe the chest through several respiratory cycles – Look for symmetrical, concordant chest movement – Paradoxical movement or flail chest – Diaphragmatic breathing – spinal cord injury Approach to Evaluating the Airway • Auscultation of the chest – Assess adequacy of air exchange – Decreased breath sounds in hemothorax, pneumothorax, or other pulmonary process • Monitor pulse oximetry, capnography, and mentation – ABGs rarely helpful in the decision to intubate • Anticipate clinical course! Identification of the Difficult and Failed Airway The Failed Airway • Failure to maintain acceptable oxygen saturation during or after on or more failed laryngoscopic attempts (CICO) or • Three failed attempts at orotracheal intubation by an experienced intubator, even when oxygen saturation can be maintained. Clinical presentations of the Failed Airway • There is not sufficient time to evaluate or attempt a series of rescue options, and the airway must be secured immediately because of an inability to maintain O2 sats via BVM. (CICO) • There is time to evaluate and execute various options because the patient is in a “can’t intubate, can oxygenate situation” Four Technical Operations of the Difficult Airway • Difficult Bag Valve Mask Ventilation – MOANS • Difficult Laryngoscopy and Intubation – LEMON • Difficult Extra-Glottic Device – RODS • Difficulty Cricothyrotomy – SHORT Difficult Bag-Mask Ventilation: MOANS • Mask Seal • Obstruction/Obesity • Age >55 • No Teeth • Stiff lungs Difficult Laryngoscopy and Intubation: LEMON • Look Externally • Evaluate 3-3-2 • Mallampati Score • Obstruction/Obesity • Neck Mobility Difficult Laryngoscopy and Intubation: LEMON • Look Externally • Gestalt • Gut Feeling • First Impression – “This looks bad!” Difficult Laryngoscopy and Intubation: LEMON • Evaluate 3-3-2 Rule: – Relates the mouth opening to size of the mandible to the position of the larynx in terms of likelihood of successful visualization of the glottis by direct laryngoscopy Difficult Laryngoscopy and Intubation: LEMON • Mouth must open adequately to permit visualization past the tongue when both the blade and ET tube are within the oral cavity • The mandible must be sufficient size to allow the tongue to be displaced fully into the submandibular space • The glottis must be located a sufficient distance caudad from the base of the tongue so that a direct line of site can be created to look from mouth to vocal cords as the tongue is displaced inferiorly Difficult Laryngoscopy and Intubation: LEMON • First “3” • Assesses for mouth opening • 3 fingers between the upper and lower incisors Difficult Laryngoscopy and Intubation: LEMON • Second “3” • Length of the Mandibular space • Mentum to hyoid Difficult Laryngoscopy and Intubation: LEMON • “2” • Position of the glottis in relation to the base of the tongue • Space from Chin-neck junction (hyoid) to and thyroid notch Difficult Laryngoscopy and Intubation: LEMON • Mallampati – Sitting Up – Head in sniffing position – Open mouth, protrude tongue without phonation • Class I-IV • Class I & II = low intubation failure rate • Class III & IV = intubation failure may be > 10% Difficult Laryngoscopy and Intubation: LEMON Difficult Laryngoscopy and Intubation: LEMON • Obstruction/Obesity • Four Cardinal Signs of Upper Airway Obstruction: – Muffled voice – Difficulty swallowing secretions – Stridor – Sensation of dyspnea Difficult Laryngoscopy and Intubation: LEMON • Stridor – Occurs when airway circumference is less than 50% of normal (4.5mm or less) • May quickly lead to total obstruction with administration of opiates or benzos – Loose the stenting of open airways • Prepare for double set up Difficult Laryngoscopy and Intubation: LEMON • Neck Mobility – C spine immobilization may compound the effects of other difficult airway markers • Trauma, RA, Ankylosing Spondylitis • May require video laryngoscopy Difficult Extraglottic Device: RODS • Restricted Mouth Opening • Obstruction • Disrupted or Distorted Airway • Stiff Lungs or Cervical Spine Difficult Extraglottic Device: RODS • Restricted Mouth Opening – Allowing for oral access to insert device Difficult Extraglottic Device: RODS • Obstruction – Upper airway obstruction at larynx or below Difficult Extraglottic Device: RODS • Disrupted or Distorted Airway – Seat/Seal compromised of the device Difficult Extraglottic Device: RODS • Stiff Lungs or Cervical Spine – Increased airway resistance • Severe Asthma – Decreased pulmonary compliance • Pulmonary Edema – Decreased Cervical Movement Difficult Cricothyrotomy: SHORT • Surgery or Disrupted Airway • Hematoma (infection/abscess) • Obesity • Radiation • Tumor Difficult Cricothyrotomy: SHORT • Surgery or Airway Disruption – Anatomy distortion – Halo Device Difficult Cricothyrotomy: SHORT • Hematoma – Infection – Trauma or Postop – Not a contraindication Difficult Cricothyrotomy: SHORT • Obesity – – – – Access Short neck Large pannus Subcutaneous Emphysema – Careful palpation to overcome! Difficult Cricothyrotomy: SHORT • Radiation – Distortion of Anatomy – Scar Tissue – Fixed Flexion Deformity of the Spine Difficult Cricothyrotomy: SHORT • Tumor – Extrinsic – Intrinsic Acknowledgement • Manual of Emergency Airway Management, 3rd Edition. Walls, R. and Murphy, M. 2008.