Cooperative Education: A Transprofessional Education Model for Oral Health and Primary
advertisement

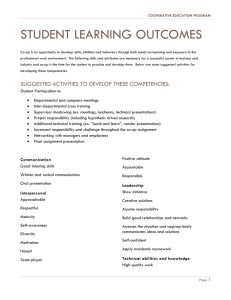
Cooperative Education: A Transprofessional Education Model for Oral Health and Primary Care Practice Integration 2015 Collaborating Across Borders V Roanoke, VA September 30, 2015 Authors Northeastern University: Maria Dolce, PhD, RN, CNE Jessica Holloman, MS, BSDH Dierdre Jordan, MS Veronica Ramirez, Health Sciences Student c/o ‘16 Boston Health Care for the Homeless Program: Pooja Bhalla, RN Colleen Anderson, DDS Learning Outcomes • Discuss the importance of integrating oral health and primary care practice. • Describe a Co-op model for integrating oral health and primary care competencies. • Apply Co-op strategies at your institution. Panel Overview • Bouvé College of Health Sciences at Northeastern University • Innovations in Oral Health Program • Oral health & primary care integration • Co-operative education • Co-op model: – Development, setting, implementation, evaluation • The student perspective Founded 1898 1,157 full-time faculty 30,000 students Bouvé College of Health Sciences 2,800 students 205 full-time faculty 3 Schools Three Schools: • Nursing • Pharmacy • Health Professions – Counseling & Applied Educational Psychology – Health Informatics – Health Science – Physical Therapy – Speech-language Pathology/Audiology – Physician Assistant Studies – Public Health 2013 - 2018 Strategic Plan Goal 1. To be a national model for interprofessional health education. In preparing students for interprofessional practice through campus-based learning and experiential education, the College will: •Incorporate interprofessional education and practice throughout student learning experiences. •Assess and expand the College’s capacity to engage in interprofessional education and practice. •Promote interprofessional education and practice through scholarship. Innovations in Oral Health: Technology, Instruction, Practice, Service The DentaQuest Foundation is committed to optimal oral health for all Americans through its support of prevention and access to affordable care, and through its partnerships with funders, policymakers and community leaders. For more information, please visit dentaquestfoundation.org Improve Workforce Training and Capacity Building • Primary care • Rural and medically underserved areas • Preventive medicine • Public health • Behavioral health • Oral health • Team management of chronic disease Experiential Curriculum Guiding Principles • Core competencies collaborative practice • Person- and family centered • Integrated care • Primary care and communitybased settings SimulationLearning • Students from two or more disciplines • Team-based • Standardized patient cases • Scenarios address health care needs of vulnerable and underserved populations Cooperative Education • “Co-op” • Integrate academic study and full-time employment • Work-based learning • Integrate classroom learning and real-world experiences Community Service-LearningLearning • Faculty-led partnerships with communitybased entities • Address needs or interests identified by the community • Hands-on roles and projects 100+ Years of Co-op History 1909 2015 Co-op Connects Academic and Experiential Traditional Approach • Students attend classes • Students complete internship or work assignment • Classes and work are two distinct experiences Innovative Approach • Classes and Co-op are integrated – Co-op preparation course – Guided reflection during and after Co-op – Related online coursework during Co-op Class Class Co-op + Co-op Co-op Cycle POWERFUL LEARNING MODEL Intellectual Inquiry Experiential Education Global Opportunities Required Core Courses • American Healthcare Systems • Community and Public Health • Communication Skills for the Healthcare Professional • Biostatistics • Healthcare Management • Race, Ethnicity and Health • Health Education & Program Planning • Health Policy Required Courses • • • • • • • • • Chemistry 1 & 2 Biology 1 & 2 Anatomy and Physiology 1 & 2 Calculus Nutrition Foundations of Psychology Healthcare Research College and Advanced Writing Professional Development Coop • Capstone BEHRAKIS HEALTH SCIENCES CENTER: AN INNOVATIVE LEARNING ENVIRONMENT • State-of-the-art classrooms and labs • Arnold S. Goldstein Simulation Laboratories with nine highfidelity patient simulators, video capture technology, four simulation bays, and two debriefing rooms • Interdisciplinary healthcare team approach • Clinical faculty who are practicing professionals HEALTH SCIENCE @ NU: INTELLECTUAL INQUIRY • What is Health Science? • Challenging coursework • Flexibility • Outstanding faculty Essentials for Co-operative Education 1. Mindfulness in learning 2. Reflections promote deep learning 3. Student-Employer goal planning 4. Student self-evaluations & Employer evaluation Competency Frameworks Job Description • Assist with risk assessments & oral health evaluations • Develop patient education tools • Provide oral health education to patients • Collaborate with medical and dental providers • Participate in medical/dental integration meetings • Develop resource and referral networks for use at medical sites • Design and conduct a survey for patient needs at outreach sites 22 Student Learning Outcomes IPEC: •Engage other health professionals – appropriate to the specific care situation – in shared patient-centered problem solving. •Perform effectively on teams and in different team roles in a variety of settings. HRSA: •Conduct preliminary patient-specific, oral health risk assessments on all patients. •In collaboration with a dental provider, perform oral health evaluations linking patient history, risk assessment, and clinical findings 23 Workshops • Teamwork & Communication in Health Care • Risk Assessment • The Oral Exam • Fluoride Varnish 24 Evaluation Methods • TeamSTEPPS® T-TAQ • Oral Health Knowledge, Skills, and Attitudes Survey • Workshop Evaluation Forms • BHCHP Data • Student reflections 25 Patient-Centered Medical Home BHCHP Mission To provide & assure access to the highest quality health care for Boston’s homeless men, women & children Photos courtesy of J O’Connell Homeless Health • Acute & chronic health problems • Morbidity & mortality • Premature aging • Delayed treatment & reliance on ED • Access to health care • Follow-up • Trust & hope BHCHP Care Model • Patient-centered • Comprehensive • Collaborative, team-based • Culturally competent • High quality Jean Yawkey Place Boston Medical Center Family Team Street Team Suffolk Downs Racetrack Barbara McInnis House Evolution to PCMH • • • • • Care teams CCM & Risk Stratification Population Management Open Access EMR Changes – Med Rec – Goal Setting – Visit Summaries Case Conferencing What is PCMH, again? • Improved access and continuity for patients • Collecting and using data in EMR to better care for patients • Care coordination across settings • Providing patients with selfmanagement support • Data gathering and quality improvement Oral Health in the Homeless Population • Oral disease is very prevalent in the homeless population – Higher incidence of caries, gum disease, tooth loss, and oral pain • Disease conditions are more often severe when diagnosed • Access to treatment is often difficult to obtain • Often a low priority for patients • At BHCHP, Dental sees less than 25% of our overall patients How do we provide oral health care to the rest of our patients? 38 Medical and Dental Integration at BHCHP Formed a multidisciplinary Integration Team • 1st Goal: increase the oral health care patients receive in medical settings • Oral exams to identify/screen for disease • Provide oral health education • Identify acute issues for immediate referral • Connect patients with dental clinics • Target: • Primary care patients at our main medical clinic • Family Team patients at a variety of family shelter settings Initial Integration Steps Changes to EMR medical notes 40 • • • • Challenges Resources are limited Staff may not feel they have the right skills There are many competing priorities How do you make the connections? 41 The Co-op Position • A new role for BHCHP “oral health coordinator/oral health community support worker” • An oral health ambassador to other parts of the program -both patients and staff! • A researcher and resource finder • An organizer – events, publicity, patient education • A care coordinator for individual patients Training and Position Development • • • • • • Site visits Medical and dental conditions common to the homeless population Assisting and observing in the dental clinic Work shops on oral health topics for all BHCHP co-ops Time for the student to help develop and define the role Scheduled to rotate in the main medical clinic, three family team sites, and the dental clinic. Integration Efforts • Staff knowledge and attitude survey • Adult and pediatric oral health risk assessment tools • Staff trainings • Oral health fairs at family team sites • Resources for staff and patients • Events to raise staff awareness and encourage oral exams • Risk assessments, patient education, and care coordination within our medical clinic and family team clinics Student Perspective Veronica Ramirez, Health Sciences Student c/o ‘16 Background • Grew up in an urban setting as a culture and community oriented individual • Interested in the field of dental medicine for over 8 years • Involved in a student driven interprofessional organization • Currently a senior majoring in Health Sciences at Northeastern University 46 The Co-op Search • Looking to –Gain clinical experience in a dental setting with patient interaction –Expand my knowledge and skills in interprofessional education –Work with an underserved population –Practice my bilingual medical terminology 47 Professional Development • Practiced leadership skills by – Coordinating dental care for patients and providing education on the oral-systemic connection – Designing a risk assessment tool for non-dental staff – Participating in the development of a simulation-based training on oral health for medical staff and case managers – Organizing oral health fairs and an oral exam challenge for the medical staff 48 Improving Oral Exam Count 49 Results • Scheduled a total of 110 appointments • Applied fluoride varnish to 29 children • Increased percentage of patients receiving oral health exams in the medical setting by 21% 50 Professional Development • Patient interaction – Building rapport – Translating book knowledge to simple conversational language – Problem solving and critical thinking • Academic knowledge – Variety of working environments that highlighted the interprofessional environment – In depth opportunities to learn about dental treatment plans, protocols and procedures 51 Personal Development • Clarification of professional goals • Became a more compassionate, patient and dedicated individual • Helping to achieve patient centered care • Stronger understanding of interprofessional education and competencies in medical and dental setting 52 The DentaQuest Foundation is committed to optimal oral health for all Americans through its support of prevention and access to affordable care, and through its partnerships with funders, policymakers and community leaders. For more information, please visit dentaquestfoundation.org Thank you QUESTIONS ? m.dolce@neu.edu j.holloman@neu.edu