METROPOLITAN COMMUNITY COLLEGE – Mental Health Nursing II NURS2310
advertisement
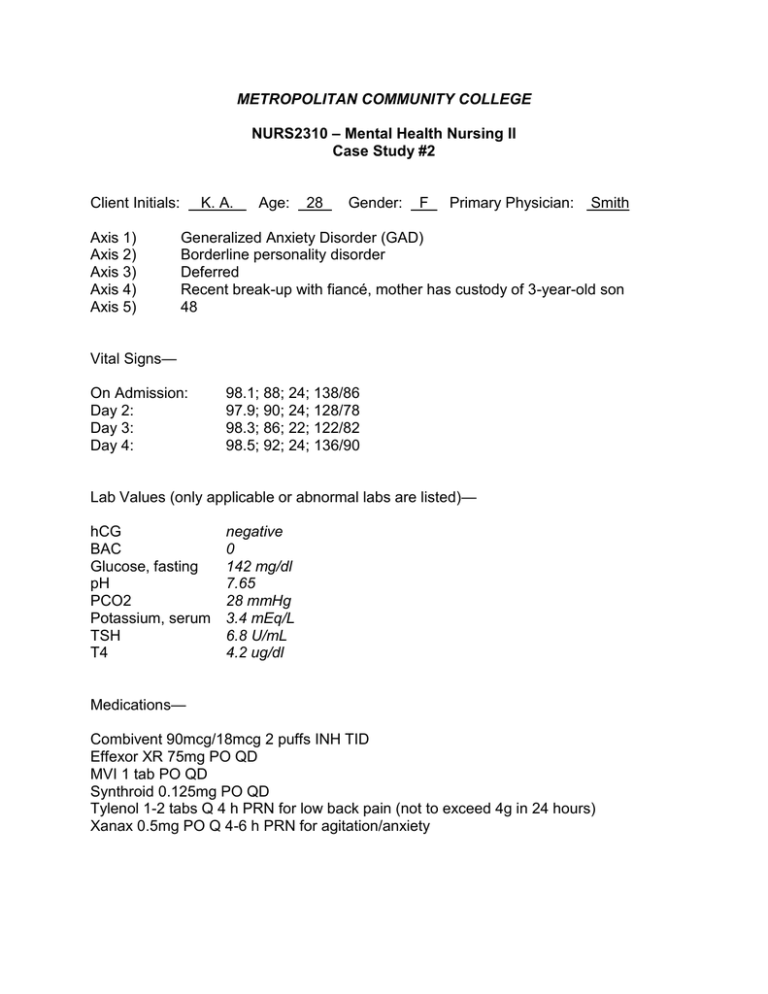
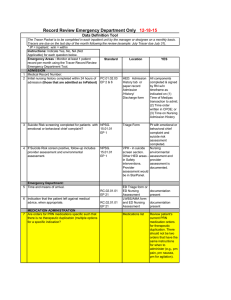
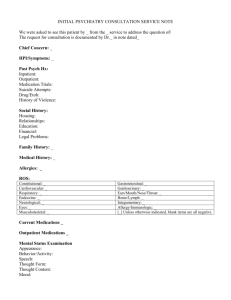
METROPOLITAN COMMUNITY COLLEGE NURS2310 – Mental Health Nursing II Case Study #2 Client Initials: _K. A. Axis 1) Axis 2) Axis 3) Axis 4) Axis 5) Age: 28 Gender: F Primary Physician: Smith Generalized Anxiety Disorder (GAD) Borderline personality disorder Deferred Recent break-up with fiancé, mother has custody of 3-year-old son 48 Vital Signs— On Admission: Day 2: Day 3: Day 4: 98.1; 88; 24; 138/86 97.9; 90; 24; 128/78 98.3; 86; 22; 122/82 98.5; 92; 24; 136/90 Lab Values (only applicable or abnormal labs are listed)— hCG BAC Glucose, fasting pH PCO2 Potassium, serum TSH T4 negative 0 142 mg/dl 7.65 28 mmHg 3.4 mEq/L 6.8 U/mL 4.2 ug/dl Medications— Combivent 90mcg/18mcg 2 puffs INH TID Effexor XR 75mg PO QD MVI 1 tab PO QD Synthroid 0.125mg PO QD Tylenol 1-2 tabs Q 4 h PRN for low back pain (not to exceed 4g in 24 hours) Xanax 0.5mg PO Q 4-6 h PRN for agitation/anxiety Day Shift Nursing Notes (from Admission to the Present…) Day 1— Nursing Notes; Admission Narrative Day 2— Nursing Notes; 1:1 with Client Client admitted to the general adult psychiatric unit under a voluntary admission for suicidal ideation with a plan to cut her wrists with a razor blade. Client reports feeling depressed due to a failed relationship with her fiancé, whom she states she had met approximately two weeks prior to becoming engaged. Client says her fiancé “broke up with me on the phone the day before our 6-month anniversary”, which she reports was two days ago. Client rates her current suicidal ideation at a 4 on a scale of 0-5 with 5 being most severe. Client is able to contract for safety while hospitalized only. Client admits to previous self-harming behaviors such as burning her legs with a lit cigarette as recently as six months ago. Client states sometimes inflicting pain on herself physically is the “only thing that makes life bearable”, but denies current thoughts to self harm. Client was initiated on Q 15-minute rounds and safety precautions for suicidal ideation. A) Client complains of feeling anxious about being in the hospital. She is restless, pacing, and unable to sit through groups without leaving to pace the hallway. Client states she is waiting for a phone call from her fiancé asking for a reconciliation, and says she doesn’t know what she’ll do if that doesn’t happen. Client admits to having other stressors, such as possibly losing her job as a hostess at a local restaurant due to her hospitalization, as well as trying to regain custody of her son who lives with her mother due to the client’s inconsistent (and at times inappropriate) living arrangements. Client appears to minimize these issues in comparison to her troubled relationship with her fiancé. Client rates her SI at a 2, depression 3, anxiety 5, anger 3, and homicidal ideation 0 on a scale of 0-5 with 5 beings most severe. I) Client was given PRN Xanax for her anxiety and encouraged to journal her feelings. Client maintained on safety precautions via 15-minute visual checks. R) Client able to verbally contract for safety, and remains cooperative and compliant with her treatment regimen this shift. Day 3— Nursing Notes; 1:1 with Client Day 4— Nursing Notes; Safety Intervention A) Client’s affect much brighter today, and she reports seeing her fiancé last evening during visiting hours on the unit. Client states her fiancé wants to resume their relationship, and she is requesting to be discharged home as a result. Client denies SI, HI, or depression this shift. Client admits to feeling anxious because she wants to leave the hospital so she can see her fiancé. Client rates her anxiety at a 5 on a 0-5 scale, and is unable to verbalize appropriate coping skills she can use to decrease her emotional distress. I) Client given PRN Xanax for anxiety. Discussed with client measures she can take to deal with her feelings, such as deep-breathing techniques, imagery, and journaling. Client encouraged to work on her safety plan so that it will be an effective tool in assisting her in maintaining her safety at home. R) Client states she will use the deep-breathing techniques she learned in patient education group as a healthy coping skill at home, and she verbalizes understanding of the importance of completing her safety plan prior to discharge. Client reports a decrease in her anxiety level to 2/5 after taking her prescribed PRN anxiolytic. A) Client approached the nurse’s station after breakfast demanding to leave immediately. Client’s speech is loud and pressured, and her pacing in the hallway has increased. Client refuses her PRN medication, and states none of her coping skills are helping. Client is threatening staff that she will call the police to report her “mistreatment and false imprisonment in this crazy place” if she is not released right away. I) Attempted to discuss with client the benefits of being in the hospital in terms of a safe environment for learning to adapt to her day-to-day stressors, but client remains uncooperative with treatment and disruptive to the unit milieu. Physician called for orders to change client’s status from voluntary admission to involuntary hospitalization under a physician’s hold. R) Client yelled obscenities at staff and ran to her room, slamming her door, after being told she would not be allowed to leave the facility until her physician has determined that she can stay safe outside of the hospital. Client remains on safety precautions via 15-minute visual rounds, and will continue to be given the opportunity to ventilate her feelings in an appropriate manner.