Mental Health Nursing II NURS 2310 Unit 1 Basic Concepts of Mental
advertisement
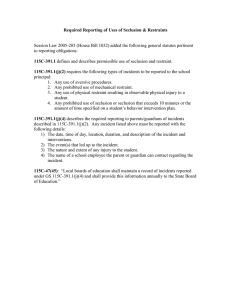
Mental Health Nursing II NURS 2310 Unit 1 Basic Concepts of Mental Health and Mental Illness Objective 1 Exploring the historical overview of care of the mentally ill client In the Beginning No known treatment for the mentally ill before 1840 – Mental illness perceived as incurable – Only “reasonable” intervention was removing mentally ill persons from the community The Birth of Community Mental Health Provided for reimbursement of mental health services through Medicare and Medicaid Resulted in the “deinstitutionalization” of the mentally ill Deinstitutionalization of the Mentally Ill The deinstitutionalization movement occurred throughout the late 1950’s and early 1960’s – 500,000 people lived in state mental hospitals in 1955 – Right to freedom at issue Communities unable to sustain care for mentally ill – Insufficient planning – Budget cuts reduced mandated services – Mentally ill became homeless – Outcome is “revolving door” syndrome The Problems That Remain The mentally ill comprise a great majority of the homeless population Many person with chronic mental illness end up in jails and emergency rooms Not enough community services/facilities to provide adequate care for mental illness Medicaid, Medicare, and other 3rd-party payers do not reimburse mental health services at the same rate as medical services Continuing stigma of mental illness Objective 2 Reviewing concepts related to mental health and mental illness Mental health The successful adaptation to stressors from the internal or external environment, evidenced by thoughts, feelings, and behaviors that are ageappropriate and congruent with local and cultural norms. Mental illness Maladaptive responses to stressors from the internal or external environment, evidenced by thoughts, feelings, and behaviors that are incongruent with local and cultural norms, and interfere with the individual’s social, occupational, and/or physical functioning. Self-esteem One’s opinion of oneself; a confidence and satisfaction in oneself. Self-awareness An awareness of one’s own personality or individuality. Sanity Soundness or health of mind; one’s ability to bear legal responsibility for one’s actions. Resilience Ability to recover from or adjust easily to misfortune or change. Well-being The state of being happy, healthy, or prosperous. Empowerment To promote the self-actualization or influence of. Assertiveness The expression of opinions, needs, and feelings without negating the opinions, needs, and feelings of others. Objective 3 Identifying members of the mental health team and their roles Psychiatrist Medical doctor with special training in mental illness and behavioral/emotional problems Diagnoses conditions and prescribes medical treatment Clinical psychologist Provides individual and group therapy Performs psychiatric testing Therapist Provides individual therapy Conducts group therapy sessions Social worker Community resource education Discharge planning Recreation therapist Incorporates leisure activities in group settings to demonstrate healthy coping mechanisms Nurse Administers medications Conducts group education sessions Provides patient support and directs patient care Psychiatric technician Assists nursing staff Provides support to client Objective 4 Reviewing the ANA Standards of Psychiatric and Mental Health Nursing Practice The American Nurses’ Association (ANA) has identified five standards of psychiatric and mental health nursing practice: Standard I – Assessment Standard II – Diagnosis Standard III – Outcome Identification Standard IV – Planning Standard V – Implementation Standard V includes milieu therapy, promotion of self-care activities, psychobiological interventions, health teaching, case management, health promotion and health maintenance Objective 5 Describing the composition of the Board of Mental Health in Nebraska and Iowa Iowa’s mental health committals are handled by the county court in which the ill individual resides. The Board of Mental Health in Nebraska consists of: 2 2 2 2 2 licensed mental health practitioners certified marriage and family therapists certified master social workers certified professional counselors public members Members of the BOMH serve for 5 years, with no more than 2 consecutive 5-year terms. At least one member of the board must be a member of a racial or ethnic minority. The professional members of Nebraska’s BOMH must meet the following requirements: Be actively engaged in the practice of his/her profession Be working in his/her profession within the State of Nebraska Be working under a license issued in this state Have a 5-year history of working in his/her profession just preceding the appointment The public members of Nebraska’s BOMH must meet the following requirements: Be a resident of this state Attained the age of majority Represent the interests and viewpoints of consumers Not be a present or former member of a credentialed profession, an employee of a member of a credentialed profession, or an immediate family or household member of any person presently regulated by such board Objective 6 Examining psychiatric client rights Universal Bill of Rights for Mental Health Patients Mental Health Systems Act of 1980 Right to the least restrictive treatment alternative Right to informed consent Right to refuse treatment Right to confidentiality Right to keep personal items Right to the least restrictive treatment alternative The nurse must attempt to provide treatment in a manner that least restricts freedom Right to informed consent Informed consent is the client’s permission to perform treatment Legal liability for informed consent lies with the physician The nurse acts as the client’s advocate to ensure informed consent was obtained Right to refuse treatment The patient has the right to refuse treatment to the extent permitted by law, and to be informed of the medical consequences of his or her action Right to confidentiality Pt’s privacy is protected by Amendments IV, V, and XIV Protection of client records and communications per state statute Right to keep personal items People in a hospital or other treatment facility retain the right to keep their personal possessions Items must be protected and returned upon release from the facility Exceptions include: – the belonging poses a serious threat to self or others – items that may be dangerous would be held in a secure place during hospitalization – personal items must be returned to the client upon release from the facility – (each facility has own guidelines regarding confiscated illegal items) Psychiatric patients have the right to freedom from restraint or seclusion except in an emergency situation: Restraints or seclusion are used for an individual whose behavior is out of control and who poses an inherent risk to the physical safety and psychological well-being of the individual and staff or others. Restraints or seclusion are never used for punishment or for the convenience of staff. Mechanical Restraints – set of leather straps 5-point maximum use 2-point minimum use – used to restrain the extremities of the individual – individual is always in seclusion if in restraints Physical Restraints – Seclusion (solitary confinement in a locked room) – Holding (used with smaller children) Requires 1:1 supervision Restraints and Seclusion Guidelines Restraints or seclusion can be initiated without a physician’s order in an emergency Physician must be notified for an order within 1 hour of initiation Renewal of restraint or seclusion orders – Every 4 hours for adults – Every 2 hours for children 9 years and older – Every 1 hour for children younger than age 9 Restraints and Seclusion Guidelines (cont’d) In-person evaluation of individual in restraints or seclusion by the physician – Within 4 hours of initiating restraints or seclusion for an adult – Within 2 hours of initiating restraints or seclusion for a child In-person re-evaluation of individual in restraints or seclusion by the physician – Every 8 hours for an adult – Every 4 hours for a child The nurse must assess and document circulation, respiration, nutrition, hydration, and elimination every 15 minutes Concepts related to the Right to Freedom False imprisonment = the deliberate and unauthorized confinement of a person within fixed limits (can be verbal or physical) – may include taking a client’s clothes for purposes of detainment against his or her will Assault = an act that results in a person’s genuine fear and apprehension that he or she will be touched without consent Battery = the touching of another person without consent (harm or injury may or may not occur Major Elements of Informed Consent Knowledge Competency Free will Treatment may be performed without obtaining informed consent under these conditions: The client is mentally incompetent to make a decision and treatment is necessary to preserve life or avoid serious harm Refusal endangers the life or health of another An emergency situation Client is a minor Therapeutic privilege (full disclosure would complicate treatment, cause severe psychological harm, or be so upsetting as to render a rational decision impossible) Objective 7 Discussing confidentiality in psychiatric care Health Insurance Portability and Accountability Act (HIPAA) of 1996 The individual has the right to access his/her medical records The individual has the right to have corrections made to his/her medical records The individual has the right to decide with whom his/her medical information may be shared Breach of Confidentiality Revealing aspects about a client’s case Revealing that an individual has been hospitalized Defamation of Character Sharing of malicious and false information that is detrimental to an individual’s reputation Client may seek legal restitution if making the information known resulted in harm Libel = information shared in writing Slander = information shared orally Invasion of Privacy Searching a client without probable cause Objective 8 Discussing criteria for hospitalization of a mentally ill client In order to be considered eligible for admission to an acute inpatient psychiatric unit, an individual must meet one or more of the following criteria: The client is an imminent threat to himself/herself The client poses an imminent threat to the safety and/or well-being of others The client is unable to provide for his/her basic needs in spite of having adequate resources The client is out of control Objective 9 Comparing voluntary hospitalization, involuntary hospitalization, and involuntary commitment Voluntary Hospitalization Admission process similar to medical hospitalization Patient may stay as long as treatment is deemed necessary Patient can leave at any time Involuntary Hospitalization Client is hospitalized without consent Situation must be considered an emergency Client receives observation and treatment for mental illness May occur when an individual is unable to take care of his/her basic needs in spite of having adequate resources to do so Involuntary Commitment In the State of Nebraska, an individual can be involuntarily committed subject to due process and as a result of being a danger to self or others as manifested by: Recent threats or acts of violence Substantial risk of serious harm evidenced by inability to provide for basic human needs, including food, clothing, shelter, essential medical care, or personal safety Types of Involuntary Commitment “Voluntary” commitment via a guardian Emergency Protective Custody (EPC) Physician hold Board of Mental Health hold Board of Mental Health commitment “Voluntary” Commitment via a Guardian Guardian may voluntarily commit ward to a mental health treatment facility No due process required Emergency Protective Custody (EPC) Police custody 36-hour time limit Terminates automatically or by county attorney intervention Physician Hold May follow EPC or voluntary admission 48-hour time limit Board of Mental Health (BOMH) Hold Petition can be filed by anyone at any time Petition must include sufficient documentation that an individual is at imminent risk of harming self/others Once approved, client brought to hospital/psychiatric facility – BOMH hearing set for 7 calendar days – Client served with copy of BOMH petition – Client has the right to attend hearing and be represented by an attorney Physician can drop petition after assessment of client with approval from the county attorney Board of Mental Health (BOMH) Commitment BOMH determines whether a client should be involuntarily committed to inpatient or outpatient treatment during the BOMH hearing following the filing and approval of the petition BOMH treatment plan must be approved during the process of the hearing as this directs client’s care throughout his/her commitment Committal must be reviewed periodically, as well as upon appeal by client/client’s attorney or physician Ultimate goal of the BOMH is to use the least restrictive means possible to ensure the client receives necessary treatment