Lecture 7-214.ppt
advertisement
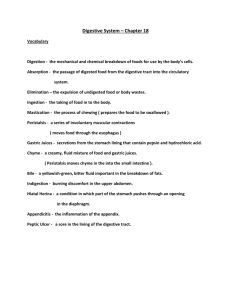
Digestive System Digestive System The organs that break down food to molecular size before it can be absorbed by the digestive system and used by the cells Digestive System Composed of the GI tract and accessory structures Digestive System GI tract – a tube open at both ends for the transit of food and wastes during processing Digestive System 1. 2. 3. 4. 5. 6. GI tract includes Mouth Pharynx Esophagus Stomach Small intestine Large intestine Digestive System Acessory structures contribute to food processing Digestive System 1. 2. 3. 4. 5. 6. Accessory structures include Teeth Tongue Salivary glands Liver Gallbladder pancreas Digestive System Includes six basic processes Layers of GI Tract 1. 2. 3. 4. Mucosa Submucosa Muscularis Serosa Mucosa Consists of 1. Epithelium 2. Lamina propria 3. Muscularis mucosa Epithelium Non-keratinized stratified squamous epithelium in the esophagus Epithelium Simple columnar in the rest of the tract Lamina propria Contains loose connective tissue Lamina Propria Blood and lymph vessels Lamina Propria Nerves and sensors Muscularis Mucosa Causes local folding of the mucosal layer to increase surface area for digestion and absorption 2. Submucosa Consists of areolar connective tissue Submucosa Submucosal plexus Submucosa Glands and lymphatic tissue 3. Muscularis The mouth, pharynx, and superior part of the esophagus contains skeletal muscle that produces voluntary swallowing Muscularis Skeletal muscle forms the external (voluntary) anal sphincter Muscularis Consists of smooth muscle in an inner sheet of circular fibers and an outer sheet of longitudinal fibers Muscularis Stomach contains an inner oblique layer also 3. Serosa Superficial layer of the GI tract Serosa The esophagus is covered by an adventitia instead of serosa Serosa Inferior to the diaphragm also called the visceral peritoneum Peritoneum Largest serous membrane of the body Peritoneum Two layers Peritoneum 1. 2. Parietal peritoneum Visceral peritoneum Parietal Peritoneum Lines the wall of the abdominal cavity Visceral Peritoneum Covers some of the organs Peritoneal Cavity The space between the parietal and visceral portions that contains serous fluid Mouth Oral cavity Mouth Formed by the cheeks, hard and soft palate, lips, and tongue Mouth The space extends from the gums and teeth to the fauces Mouth Fauces – opening between the oral cavity and pharynx Salivary Glands Lie outside the mouth and pour their contents into ducts that empty into the oral cavity Salivary Glands Produce saliva Salivary Glands 1. 2. 3. Three pairs Parotid Submandibular Sublingual Salivary Glands Saliva lubricates and dissolves food Salivary Glands Saliva start the chemical digestion of carbs Salivary Glands Parasympathetics stimulate secretion of watery saliva Salivary Glands Sympathetics stimulate the secretion of thick, tacky, saliva Mumps Inflammation and enlargement of the parotid gland Mumps Symptoms include fever, pain, and swelling of one or both glands Tongue Composed of skeletal muscle covered with mucous membrane Tongue The upper surface and sides are covered with papillae Tongue Some papillae contain taste buds Tongue On the dorsum of the tongue are glands that secrete lingual lipase Teeth Adapted for mechanical digestion Teeth 1. 2. 3. Consists of Crown Neck Root Teeth Teeth composed of dentin Teeth Dentin – calcified connective tissue that gives the tooth its basic shape and rigidity Teeth Dentin of the crown is covered by enamel Teeth The dentin of the root is covered by cementum Teeth Cementum – attaches the root to the periodontal ligament Teeth The dentin encloses the pulp cavity in the crown and the root canals in the root Teeth 1. 2. Two sets of teeth Deciduous (primary) Pemanent (secondary) Teeth Salivary amylase – converts polysaccharides (starches) to disaccharides (maltose) Pharynx Composed of skeletal muscle and lined by mucous membrane Pharynx 1. 2. 3. Consists of Nasopharynx Oropharynx laryngopharynx Pharynx Swallowing moves food from the mouth to the stomach Esophagus Behind the trachea Esophagus Connects the pharynx to the stomach Esophagus Serosa called the adventitia Esophagus Contains an upper and lower esophageal sphinchter Esophagus Highly coordinated, propulsive contractions (peristalsis) of the muscularis push the bolus distally Stomach J-shaped Stomach Begins at the bottom of the esophagus and ends at the pyloric sphincter Stomach Pyloric sphincter – separates the stomach from the duodenum Stomach Mixing and holding area for food Stomach Begins the digestion of food Stomach Water, HCL, and pepsin covert the bolus of food to a clear liquid called chyme Stomach Can absorb water, alcohol, and apirin Stomach 1. 2. 3. 4. Three regions Cardiac Fundus Body Antrum Stomach When stomach is empty, the mucosa lies in folds called rugae Stomach Surface of the mucosa is a layer of simple columnar epithelium Stomach Epithelial cells extend down into the lamina propria forming gastric pits and the narrower and deeper continuations of the these, called gastric glands Stomach 1. 2. 3. Gastric glands consist of 3 types of exocrine glands Mucous neck cells Chief cells Parietal cells Stomach 1. Mucous neck cells – secrete mucous Stomach Mucous rich in bicarbonate and prevents gastric acid from damaging the epithelium Stomach 2. Chief cells secrete pepsinogen and gastric lipase Stomach Pepsinogen is activated by HCL into pepsin Stomach Pepsin can also activate pepsinogen Stomach Pepsin digests protein Stomach Gastric lipase splits certain molecules in butterfat of milk into fatty acids and monoglycerides Stomach Gastric lipase has a VERY limited role in the adult stomach Stomach 3. Parietal cells secrete HCL and intrinsic factor Stomach Intrinsic factor is important for absorption of vitamin B-12 Stomach Parietal cells contain H2 receptors, gastrin receptors, and Ach receptors Stomach H2 blockers such as Tagamet, Zantac , and Pepcid work here Stomach Parietal cells also have receptors for somatostatin which decrease acid secretion Stomach G cells in the antrum secrete the hormone Gastrin which increases acid secretion and motility Stomach Near parietal cells are mast cells that releases histamine in responses to gastrin or stimulation by the vagus Stomach Ach is released by parasympathetic fibers Stomach The serosa is a part of the visceral peritoneum Stomach Above the lesser curvature, the visceral peritoneum becomes the lesser omentum Stomach Below the greater curvature, the visceral peritoneum becomes the greater omentum Regulation of Gastric Secretion and Motility Gastric secretion is regulated by nervous and hormonal secretions Regulation of Gastric Secretion and Motility 1. 2. 3. Stimulation occurs in three overlapping phases Cephalic Gastric Intestinal Cephalic Phase Consists of reflexes initiated by sensory receptors in the head, such as when you see, smell, or think about food Cephalic Phase Stimulates salivary flow, gastric secretion and motility Gastric Phase Begins when food enters the stomach Gastric Phase Distension of stomach and increase in pH stimulate gastric secretion via parasympathetic neurons Gastric Phase This results in increase in HCL secretion Gastric Phase Protein, high pH, alcohol, and coffee also stimulates gastrin secretion Gastric Phase Histamine enhances the effects of Ach and gastrin Gastric Phase Gastrin secretion is limited by negative feedback Gastric Phase Low pH under 2 decreases it secretion Gastric Phase Somatostatin from endocrine cells in the gastric wall inhibit the secretion of gastrin and histamine Gastric Phase Somatostatin also inhibits acid secretion in parietal cells Intestinal phase Stimulated by distension, low pH, and increase in fats Intestinal Phase Long and short neural reflexes inhibit gastric acid secretion Intestinal Phase Hormones released by the intestinal tract such as Gastric inhibitory peptide (GIP), secretin, and cholecystokinin (CCK) inhibit gastric acid secretion Regulation of Gastric Emptying Gastric emptying – the periodic releases of chyme from the stomach into the duodenum Regulation of Gastric Emptying Stimulated by nerve impulses in response to distention of the stomach and gastrin Regulation of Gastric Emptying Most food leaves the stomach 2-6 hours after ingestion Regulation of Gastric Emptying Carbs leave first, then proteins, then fats Regulation of Gastric Emptying Gastric emptying is inhibited by CCK and GIP and short and long neural reflexes Regulation of Gastric Emptying GIP also promotes insulin secretion in pancreas Pancreas It is connected to the duodenum via the pancreatic duct and accessory duct Pancreas The pancreatic duct fuses with the common bile duct ate the ampulla of Vater Pancreas The pancreatic islets secrete hormones Pancreas Exocrine cells (acini) secrete a mixture of fluid and digestive enzymes called pancreatic juice Pancreas Pancreatic juice contains bicarbonate and enzymes that digest starch, proteins, fats, and nucleic acids Pancreas Bicarbonate converts the acid stomach contents to a slightly alkaline pH (7.1-8.2) Pancreas This halts pepsin acitvity and promotes the activity of pancreatic enzymes Pancreas Pancreatic amylase digests starch Pancreas Trypsin, chymotrypsin, and carboxypeptidase digest proteins Pancreas Pancreatic lipase digest fats Pancreas Ribonuclease and deoxyribonuclease digest nucleic acids Pancreas These enzymes are secreted as inactive precursors Pancreas Trypsinogen is activated by duodenal enterokinase, producing kinase Pancreas Trypsin then activates the other precursor enzymes Pancreas CCK from the duodenum stimulates the pancreas to secrete digestive enzymes and ejection of bile into the duodenum via contraction of the gall bladder Pancreas Secretin stimulates the pancreas to secrete bicarbonate Liver and Gallbladder Heaviest gland in the body Liver and Gallbladder Second largest organ in the body Liver and Gallbladder The liver is divisible into left and right lobes, separated by the falciform ligament Liver and Gallbladder The gallbladder is a sac located in a depression on the posterior surface of the liver Liver and Gallbladder The right and left hepatic duct combine to form the common hepatic duct which binds with the cystic duct to form the common bile duct Liver and Gallbladder Functions of the gall bladder are to store and concentrate bile until it is needed by the small intestine to help digest fats Liver and Gallbladder The muscularis of the gallbladder ejects bile into the cystic duct Liver and Gallbladder The liver receives a double supply of blood from the hepatic artery and the hepatic portal vein. Liver and Gallbladder The hepatic portal vein receives venous blood from the intestines. Liver and Gallbladder All blood leaves the liver the liver via the hepatic veins to the inferior vena cava. Liver and Gallbladder Hepatocytes produce bile that is stored in the gallbladder Liver and Gallbladder Bile contains bilirubin, cholesterol, and bile acids Liver and Gallbladder Bile emulsifies triglycerides Functions of the Liver Carbohydrate, lipid, and protein metabolism Functions of the Liver Removal of drugs and hormones from the blood Functions of the Liver Excretion of bilirubin Functions of the Liver Synthesis of bile salts Functions of the Liver Storage of vitamins and minerals Functions of the Liver Phagocytosis Functions of the Liver Activation of vitamin D Small Intestine Extends from the pyloric sphincter to the ileocecal sphincter Small Intestine 1. 2. 3. Divided into Duodenum Jejunum ileum Small Intestine The mucosa forms fingerlike villi Small Intestine Lacteals – lymphatic capillaries embedded in the villi for fat absorption Small Intestine 1. 2. 3. 4. Mucosal epithelium contains Absorptive cells Goblet cells Enteroendocrine cells Paneth cells Small Intestine The free surface of absorptive cells contains microvilli Small Intestine Crypts of Lieberkuhn – cavities lined by glandular epithelium in the mucosa Small Intestine Duodenal glands – located in the submucosa and secrete an alkaline mucus Small Intestine Peyer’s patches – aggregated lymphatic nodules in the submucosa of the ileum Small Intestine Brush border enzymes break down dipeptides and disaccharides on the surface of microvilli Small Intestine Segmentation – localized contraction in areas containing food Small Intestine Peristalsis – propels the chyme onward through the intestinal tract Chemical digestion in the Small Intestine Pancreatic amylase breaks down starches into maltose Chemical digestion in the Small Intestine Maltase – breaks down maltose to 2 glucoses Chemical digestion in the Small Intestine Lactase – breaks down lactose to glucose and galactose Chemical digestion in the Small Intestine Sucrase – breaks down sucrose to glucose and fructose Chemical digestion in the Small Intestine Glucose, fructose, and galactose are absorbable Chemical digestion in the Small Intestine Maltase, sucrase, and lactase are brush border disaccharidases Chemical digestion in the Small Intestine Trypsin and chymotrypsin break down proteins Chemical digestion in the Small Intestine Brush border enzymes split dipeptides to amino acids Chemical digestion in the Small Intestine Most dipeptides are split into amino acids inside epithelial cells. Chemical digestion in the Small Intestine Bile salts break the globules of triglycerides into droplets Chemical digestion in the Small Intestine Pancreatic lipase hydrolyzes triglycerides into fatty acids and monoglycerides Chemical digestion in the Small Intestine Infants have low levels of pancreatic lipase Chemical digestion in the Small Intestine Infants have lipase mainly derived from chief cells Chemical digestion in the Small Intestine Breast milk also contains lipase Large Intestine Extends from the ileocecal valve to the anus Large Intestine 1. 2. 3. 4. Subdivisions Cecum Colon Rectum Anal canal Large Intestine Appendix – hangs inferior to the cecum Large Intestine 1. 2. 3. 4. Colon divided into Ascending Transverse Descending Sigmoid portions Large Intestine The mucosa has no villi Large Intestine The mucosa has simple columnar epithelium with numerous goblet cells Large Intestine Taeniae colie – Three strips of longitudinal muscles in the muscularis Large Intestine The taeniae coli contract and gather the colon into a series of pouches called haustra Large Intestine The last stages of chemical digestion occur in the large intestine through bacterial action Large Intestine Some vitamins (K and folic acid) are synthesized by bacterial action and absorbed by the large intestine Large Intestine Absorbs water, electrolytes, and some vitamins Large Intestine Feces consist of water, inorganic salts, sloughedoff epithelial cells, bacteria, products of bacterial decomposition, and undigested parts of food Large Intestine An important organ in maintaining the body’s water balance Defecation Elimination of feces Defecation Aided by voluntary contractions of the diaphragm and abdominal muscles Defecation The external anal sphincter can be voluntarily controlled Diarrhea Frequent defecation of liquid feces Diarrhea Caused by increased motility of the intestine and can lead to dehydration and electrolyte imbalances Constipation Refers to infrequent or difficult defecation Constipation Causded by decreased motility of the intestines Constipation May be alleviated by increasing one’s intake of dietary fiber and fluids Hepatitis Inflammation of the liver Hepatitis Caused by viruses, drugs, and chemicals, including alcohol