Lecture 3-214.ppt
advertisement

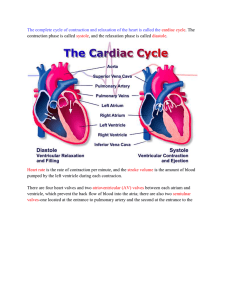
Cardiovascular System Heart Introduction of Cardiovascular Sytem 1. 2. 3. Consists of; Blood Heart Blood Vessels Location of Heart Heart lies between the lungs in the mediastinum. Location of Heart Two-thirds of its mass is to the left of the midline Location of Heart Precordium – The area of the chest anterior to the heart Location of Heart Lies between the vertebral column and the sternum Structure and Function of Heart 1. 2. Pericardium Layers of the Heart Wall Pericardium The heart is enclosed and held in place by the pericardium Pericardium 1. 2. Consists of; Fibrous pericardium (outer) Serous pericardium (inner) Pericardium Fibrous pericardium – anchors the heart in the mediastinum Pericardium 1. 2. Serous pericardium composed of; Parietal layer Visceral layer Pericardium Pericardial cavity – a space between the parietal and visceral layers filled with pericardial fluid Layer of the Heart 1. 2. 3. Epicardium Myocardium Endocardium Epicardium Consists of the visceral layer of pericardium and connective tissue (adipose) Myocardium Composed of cardiac muscle Myocardium The cells are branched, involuntary, and have one nucleus Myocardium The cells are connected by intercalated discs, which have gap junctions that allow ions to flow in between cells during depolarization Endocardium Lines the chambers and covers the connective tissue in the heart valves Endocardium It consists of endothelium Chambers of the Heart 1. 2. 3. 4. Right Atrium Right Ventricle Left Atrium Left Ventricle Chambers of the Heart On the surface of the heart are auricles and sulci Chambers of the Heart Auricles – small pouches on the anterior surface of each atrium Chambers of the Heart Sulci – Are grooves that contain coronary arteries and fat and separate the chambers Right Atrium 1. 2. 3. The right atrium receives systemic venous blood from; Superior Vena Cava Inferior Vena Cava Coronary sinus Right Atrium The atrium receives blood low in O2 and high in CO2 Right Atrium Interatrial septum - separates the right and left atria Right Atrium Fossa ovalis – an oval depression in the interatrial septum; it is a remnant of the foramen ovale Right Atrium Tricuspid Valve – Blood passes from the right atrium into the right ventricle through here Right Ventricle Forms most of the anterior surface of the heart Right Ventricle Pulmonary semilunar valve - Blood passes from the right ventricle to the pulmonary trunk via this valve Left Atrium Receives pulmonary venous blood from the pulmonary veins which is rich in oxygen and low in CO2 Left Atrium Mitral Valve – Blood passes from the left atrium to the left ventricle via this valve Left Ventricle Thickest and strongest chamber Left Ventricle Forms the apex of the heart Left Ventricle Blood passes from the left ventricle through the aortic valve into the aorta Left Ventricle During fetal life the ductus arteriosus shunts blood from the pulmonary trunk into the aorta Left Ventricle At birth the ductus arteriosus closes and becomes the ligamentum arteriosum Left Ventricle The left ventricle is separted from the right ventricle by the interventricular septum Myocardial Thickness and Function The atria walls are thin because they only pump blood to the nearby ventricles Myocardial Thickness and Function The ventricle wall are thicker because they pump blood greater distances Myocardial Thickness and Function The right ventricle walls are thinner than the left because they pump blood to the nearby lungs Myocardial Thickness and Function The left ventricle walls are thicker because they pump blood through the body Function of Heart Valves Valves open and close in response to pressure changes as the heart contracts and relaxes Myocardial Thickness and Function 1. 2. Two types of valves; Atrioventricular Valves Semilunar Atrioventricular Valves 1. 2. Tricuspid (right side) Mitral or bicuspid (left side) Atrioventricular Valves AV valves prevent blood flow from the ventricles back into the atria Atrioventricular Valves Back flow is prevented by the contraction of papillary muscles and tightening the chordae tendinae Semilunar Valves SL valves allow ejection of blood from the heart into the pulmonary arteries and aorta Semilunar Valves Prevent back flow into the ventricles Circulation of Blood 1. 2. 3. Systemic Pulmonary Coronary Systemic Circulation The left side of the heart pumps oxygenated blood from the left ventricle into the ascending aorta. Systemic Circulation The coronary arteries arise off of the ascending aorta Pulmonary Circulation The right side of the heart receives deoxygenated blood from the body. Pulmonary Circulation The right side of the heart pumps blood from the right ventricle and sends it into the lungs via the pulmonary artery Circulation of Blood Right atrium receives blood from the superior and inferior vena cava Circulation of Blood The Left atrium receives blood from the pulmonary veins Coronary Circulation It delivers oxygenated blood and nutrients to and removes CO2 and wastes from the myocardium Coronary Circulation The left and right coronary arteries branch from the ascending aorta and carry oxygenated blood Coronary Circulation 1. 2. Left coronary artery branches into the; Left anterior descending artery Circumflex artery Coronary Circulation 1. 2. Right coronary artery branches into; Marginal artery Posterior descending artery Coronary Circulation Deoxygenated blood returns to the right atrium through the coronary sinus Histology of Cardiac Muscle In comparison to skeletal muscle fibers, cardiac muscle fibers are involuntary, shorter in length, larger in diameter, and squarish rather than circular in transverse section. Histology of Cardiac Muscle They also exhibit branching Histology of Cardiac Muscle Have same arrangement of actin and myosin, and the same bands, zones, and Z discs as skeletal muscles Cardiac Conduction System There is an atrial and ventricular network Cardiac Conduction System Fibers within the networks are connected by intercalated discs Cardiac Conduction System The intercalated discs allow the fibers to work together so that each network serves as a functional unit Cardiac Conduction System Cardiac muscle cells are autorhythmic cells because they are self-excitable. Cardiac Conduction System They repeatedly generate spontaneous action potentials that then trigger heart contraction Cardiac Conduction System 1. 2. 3. 4. 5. The components of this system are; Sinoatrial node (SA) Atrioventricular node (AV) Bundle of His Right and Left Bundle branches Purkinje fibers Cardiac Conduction System SA node is the pacemaker Cardiac Conduction System From the SA node, a cardiac action potential travels throughout the atrial muscle and down to the AV node Cardiac Conduction System At the AV node the impulse is delayed (about 0.1sec) Cardiac Conduction System This gives the atria time to completely contract before ventricular contraction begins Cardiac Conduction System It then passes through the Bundle of His, Right and Left Bundle Branches, and the Purkinje fibers, resulting in ventricular contraction Cardiac Cycle 1. 2. Consists of; Systole (contraction) and Diastole (relaxation) of both atria Systole and Diastole of both ventricles Atrial Diastole The atria are relaxed Atrial Diastole They receive blood from three veins Atrial Diastole The A-V valves are open, allowing for 70% of ventricular filling. The ventricles are therefore also in diastole. Atrial Systole The SA node then fires; after this electrical event, atrial systole begins (a mechanical event) Atrial Systole Atrial contraction accounts for 30% of ventricular filling Ventricular Systole Shortly after the beginning of ventricular depolarization, ventricular systole begins Ventricular Systole The ventricles contract. The ventricular pressure becomes higher than atrial pressures, causing the AV valves to close. Ventricular Systole The SL valves open when the ventricular pressure becomes higher than aortic (pulmonary arterial) pressure. Ventricular Systole Then blood is ejected into the aorta and pulmonary trunk. Ventricular Diastole Begins when the ventricles relax Ventricular Diastole Ventricular pressures drop below arterial pressures, causing the SL valves to close Ventricular Diastole The ventricular pressures continue to drop below atrial pressures, causing the AV valves to open Auscultation Listening to sounds within the body with a stethoscope Auscultation The first heart sound (lubb) is created by the closing of the AV valves soon after ventricular systole begins Auscultation The second heart sound (dupp) represents the closing of the SL valves close to the end of the ventricular systole. Cardiac Output The volume of blood ejected from the left ventricle (or the right ventricle) into the aorta (or pulmonary trunk) each minute. Cardiac Output Cardiac Output = Stroke volume X Heart Rate Cardiac Output Stroke volume – the volume of blood ejected by the ventricle with each contraction Cardiac Output Stroke Volume = End Diastolic Volume (130ml) – End Systolic Volume (60ml) Cardiac Output Heart Rate – number of beats per minute Regulation of Heart Rate Sympathetics impulses increase heart rate and force of contraction Regulation of Heart Rate Parasympathetic impulses decrease heart rate Tachycardia Heart Rate over 100 beats/min Bradycardia Heart Rate below 60 beats/min Fibrillation Prolonged tachycardia Exercise And The Heart Sustained exercise increases oxygen demand in muscles Exercise And The Heart Resting cardiac output 5.25 Liters/minute Exercise And The Heart In sedentary people CO may go up to 22 liters/minute Exercise And The Heart In trained athletes CO may go up to 40 liters/minute Exercise And The Heart Sedentary people increase their CO during exercise by an increase in HR and SV Exercise And The Heart Sedentary people Increase in HR more dramatic Stroke volume only goes up by 10-35% Exercise And The Heart For a given activity, sedentary people’s maximum HR will be higher than in a trained athlete Exercise And The Heart Trained athletes increase their CO during exercise by an increase in HR and SV Exercise And The Heart Trained Athletes Increase in SV more dramatic than HR Their SV goes up to 60% Exercise And The Heart Athletes have larger stroke volumes due to longer filling time Electrocardiogram (ECG or EKG) Records the electrical currents of the body generated by the heart Electrocardiogram (ECG or EKG) P= depolarization of the atria Electrocardiogram (ECG or EKG) QRS= depolarization of the ventricles (repolarization of atria, but don’t see) Electrocardiogram (ECG or EKG) T= ventricles repolarization Electrocardiogram (ECG or EKG) PR interval= between beginning of atrial depolarization and ventrical depolarization Electrocardiogram (ECG or EKG) ST segment= ventricle contraction Electrocardiogram (ECG or EKG) QT interval = ventricle depolarization through ventricle repolarization