The NOIIS with rating instructions
advertisement
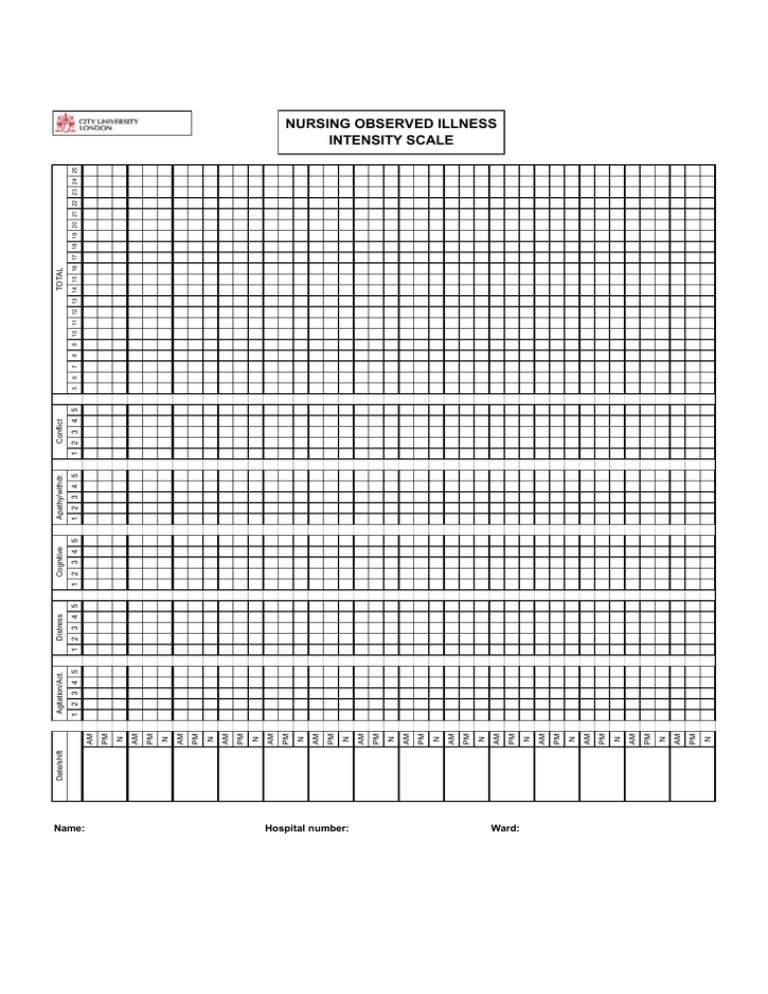
Date/shift Name: Hospital number: Ward: N PM AM N PM AM N PM AM N PM AM N PM AM N PM AM N PM AM N PM AM N PM AM N PM AM N PM AM N PM AM N PM AM N PM AM Distress 1 2 3 4 5 Agitation/Act. 1 2 3 4 5 Cognitive 1 2 3 4 5 Apathy/withdr. 1 2 3 4 5 Conflict 1 2 3 4 5 5 6 7 8 9 TOTAL 10 11 12 13 14 15 16 17 18 19 20 21 22 23 24 25 NURSING OBSERVED ILLNESS INTENSITY SCALE Please enter the score for the shift by placing a dot in the box: If you make a mistake, please cross through the dot: then enter the correct score: Agitation and activity Apathy and withdrawal Calm and relaxed all the time, no excessive movement or activity 1 Out in the day room or other public ward areas, interacting with others at a normal level and engaging in ward activities 1 Signs of restlessness from time to time (e.g. fidgeting, swinging or arms and legs, frowning, increased facial expressiveness occasional gesticulations) 2 Present in the main public ward areas, but does not initiate social interaction or activities 2 Brief episodes of pacing, of gross body movement or activity, with other signs of restlessness at other times, possibly with increased talking 3 Although present in the main ward areas, does not converse with others except in monosyllables, and passively avoids social interaction unless specifically required or encouraged 3 Extended signs of restlessness, overactivity, agitation, tension or irritability, unable to concentrate, unable to keep still or remain seated half of the time 4 Spends half the time isolating self around bed space or other areas where chances for interaction are minimised. When approached gives only brief responses. 4 Patient agitated or overactive for nearly the whole time, constantly on the go, unable to keep still, and/or tense, irritable and hyper responsive to noises or to the actions of others, and/or interfering with others 5 Isolates self at every opportunity, avoids interaction with others, spends virtually the whole time keeping solitary, and/or is close to mute 5 Psychological Distress Conflict (score the highest that applies) 1 Patient is fully compliant with ward rules and accepts all treatment and engages in therapeutic activities 1 Some discomfort due to infrequent worries, pessimism, suspicion, fear about present and/or future, or other unpleasant emotions 2 Patient fails to comply with ward rules (e.g. re smoking), and/or refuses to see workers, and/or to engage in activities, and/or wash, and/or get up and out of bed when asked, or refuses to go to bed, and/or is abusive 2 Apprehensive, suspicious, unhappy, irritable or dysphoric for most of the day but without impairment in functioning 3 Patient refuses to accept treatment (e.g. medication), or is suspected (or known) to have consumed illegal drugs or alcohol 3 Some areas of daily functioning are disturbed by anxiety, guilt, helplessness, depression, suspicion, irritability; cries or expresses distress in other ways 4 Patient attempts to or succeeds in absconding 4 Many areas of daily functioning are disrupted by constant worries, irritability, guilt, inappropriate affect, paranoia, distress, sadness, helplessness or other dysphoria 5 Patient is aggressive to objects or others, or attempts or succeeds to harm self or others 5 Calm and relaxed throughout the shift Cognitive accessibility Speech content and behaviour normal 1 Patient talks about delusions when specifically asked, or reports hearing voices when asked, or shows some thought disorder during conversation 2 Patient seeks out others to talk about delusional material, or shows obvious signs of experiencing episodes of hallucinations, or conversation is hard to understand due to thought disorder or confusion Patient's conversation dominated by delusional material, or is preoccupied with hallucinations or affected by thought disorder or confusion to the degree that conversation is difficult, but not impossible Patient totally obsessed with delusional material and/or apparently hallucinating nearly constantly, and/or impossible to communicate with at all due to cognitive disorganisation 3 4 5