Hand-Hygiene Education in Pre-Clinical Medical and Nursing Students.ppt
advertisement

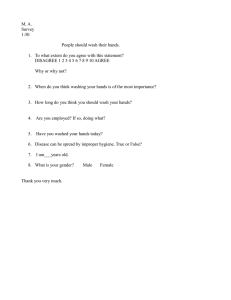
Hand-washing is a primary component of disease prevention. Several studies (Sharek et al., 2002, Lam et al., 2004, Won et al., 2004) have shown that increasing hand-washing compliance rates result in decreased rate of communicable disease in hospital settings. However, compliance with hand-washing protocols has been reported in the literature as poor with high rates of contamination (Cohen et al., 2003, Brown et al., 1996). To improve compliance it is important to understand how people think about hand-hygiene and the first step is to identify the strengths and weaknesses of their education. Infection control education varies widely between schools, years and programs of study (Danchaivijitr et al., 2005). As such, the purpose of this study is to identify the knowledge and beliefs on the subject of hand-hygiene of an interdisciplinary group of students. The specific areas of soap/water washing, alcohol hand sanitizer and glove use will be focused on. Materials and Methods Sample: Two groups were sent an email describing the project (Queen’s Medicine, 2008 and Queen’s Nursing, 2009). In 2006/07 academic year both received hand hygiene education and then began the clinical phase of training. Responses were received from 39 of 79 Nursing 2009 students and 58 of 101 Medicine 2008 students. Hand-Hygiene Education in Pre-Clinical Medical and Nursing Students Regan Giesinger (Medicine ‘08), Robyn Duffus (Nursing ‘09) QUIPPED Program, Queen’s University, Kingston ON Results 97 respondents completed the survey. Of these 2 (1 Medicine, 1 Nursing) did not answer any questions and they were removed from further analysis. Of those who did answer 38 (40%) were from Nursing 2009 and 57 (60%) were from Medicine 2008. This represents 49% and 54% response rate from Nursing and Medicine respectively. The results were divided into 3 categories based on the subject matter of the question as follows: Soap and Water The choice of how much soap was needed for adequate wash was answered similarly by both groups: 50.5% of respondents chose enough to ‘get a lather’ and 31.6% chose ‘hands coated’ as the endpoint with no statistical difference between classes. Figure 1: Duration of wash 70 60 50 Medicine Nursing 40 % 30 20 10 0 10 Questionnaire: A survey was generated by the researchers and then submitted to Dr. R. Zoutman of the Infectious Diseases Department at Kingston General Hospital for review. Questions were designed to test the knowledge and beliefs of participants in the areas of soap/water wash, alcohol sanitizer and glove use. Administration: The survey was administered via email using the Survey Monkey tool. Participants were sent a request to complete the survey the day following handhygiene education and non-responders were sent a follow up email 7 days later. The survey was closed before formal clinical rotations began. An introduction outlined the purpose of the questionnaire, confidentiality, and contact information for the researchers and the Research Ethics Board. Consent was obtained before the survey was completed. Responses were recorded with a unique ID and kept confidential. At the completion of the study responses were purged from the database. Data analysis: Results were collected and analyzed with the assistance of Wilma Hopman, the Kingston General Hospital Statistician. Acknowledgments We would like to thank the Queens Inter-professional Patient Centered Education Directive (QUIPPED) for funding this project. Thank you to Dr. R. Zoutman for his input on the questionnaire and to Wilma Hopman for her invaluable assistance with the statistical analysis of the results. 15 30 seconds Alcohol Figure 2: How does alcohol compare to soap/water at cleaning hands? As seen in Fig. 2, Nursing tended 70 to choose alcohol as better more 60 Medicine frequently than Medicine. The 50 Nursing 40 difference is significant (p=0.01). % 30 Overall, >80% believe that As can be seen in Fig.1, both 20 alcohol is at least as good as groups tended to choose longer 10 soap and water for hand hygiene. 0 hand wash, and were both split Better Same Worse Don't know between 15s and 30s. Though there was a trend for nursing to The overwhelming majority of respondents believe that choose 30s over 15s, there was alcohol is acceptable for emergency use (84%), not acceptable when hands are visibly soiled (94%) and a good no statistical significance. alternative to soap and water (94%). With no statistically significant differences between groups. Glove Use When asked if gloves were necessary for routine contact with skin, the medicine group said they were not necessary significantly more often (p=0.033). Both groups chose that gloves protected both health care worker and patient >90% of the time. Figure 3: Gloves can be used alone as adequate hygiene. 100 80 Medicine Nursing 60 % 40 20 0 Discussion Hand hygiene is taught to both groups however, the timing and intensity of education is variable and neither class received evidence based education on the subject. The Medicine students received 1 practical lab on glove use one year before clinical placement followed by a demonstration of how to wash hands in the week before clerkship begins. Nursing students had a lecture on hand hygiene in year one followed by a practical lab and seminar day including orientation to hand hygiene protocols of the various Kingston hospitals just before clinical placements began. Despite these slight differences, the two groups were largely similar in their responses. Agree The results of gloves as a sole hand hygiene method can be seen in Figure 3. Again, there is no statistical significance, however, there is a trend for the nursing group to disagree. Disagree References Brown J, Froese-Fretz A, Luckey D, Todd J.(1996) High rate of hand contamination and low rate of hand washing before infant contact in a neonatal intensive care unit. Pediatr Infect Dis J.10:908-10 Cohen B, Saiman L, Cimiotti J, Larson E. (2003) Factors associated with hand hygiene practices in two neonatal intensive care units. Pediatr Infect Dis J. 22(6):494-9. Overall, neither group had a strong tendency towards one answer in any of the questions about soap and water washing. The responses tended to be spread out over all options with larger numbers choosing more conservative answers. For example, only 3.2% of respondents chose 10s (the shortest option) as the correct one for duration of wash and with that choice eliminated, the other options were split approximately evenly. Similarly, few students chose the arbitrary ‘pump 3 times’ as the endpoint for how much soap was needed but the other two choices ‘get a lather’ and ‘hands coated’ received approximately similar number of responses. This may indicate that there is no clear message on this subject being passed on to students. Danchaivijitr S, Chakpaiwong S, Jaturatramrong U, Wachiraporntip A, Cherdrungsi R, and Sripalakij S. (2005) Program on nosocomial infection in the curricula of medicine, dentistry, nursing and medical technology in Thailand. J Med Assoc Thai. 88 Suppl 10:S150-4. Alcohol hand sanitizer has become a large part of the hand hygiene protocol of many health care institutions. It is now considered an acceptable substitute for soap/water in most situations and there is evidence that alcohol is equal to traditional surgical scrub techniques (Gupta et al., 2007). However, in this study population, 17% of students believed that alcohol was inferior to soap and water washing and only 50% of students chose alcohol as the superior method. Additionally, nursing students had a significant edge over medicine students in choosing correctly in this area (p=0.01). The lack of significant differences in other questions about alcohol use may reflect the fact that though students do not know whether alcohol or soap and water is better, they do recognize that either one is better than no hand wash. Gupta C, Czubatyj AM. Briski LE. Malani AK. (2007) Comparison of two alcohol-based surgical scrub solutions with an iodine-based scrub brush for presurgical antiseptic effectiveness in a community hospital. Journal of Hospital Infection. 65(1):65-71 The use of gloves without proper hand wash is a significant area of difficulty in Kingston General Hospital (Giesinger et al., 2005). It is encouraging that most students know that gloves protect both health care worker and patient, however, in this study 32% of people believed that gloves are acceptable as a sole method of hand hygiene. This represents a large group of new health care workers who have not learned that gloves are not a substitute, but an adjuvant to hand washing despite education to that effect. In general, the responses to this survey suggest that there is no clear message being sent to new health care workers on the acceptable use of various hand hygiene methods. However, though nursing students did tend to do better in general, it was only in the use of alcohol hand sanitizer that there was a clear difference between the two groups. Both groups of students and hand hygiene compliance in general would likely benefit from clear, practical and easily remembered education before entering clinical placements. Giesinger R, Nova N. and Flavin M. (2006) Hand hygiene compliance in the Neonatal ICU. Presented: Health Sciences Research Trainees Meeting, Queen’s University. Lam B, Lee J, Lau Y. Hand Hygiene Practices in a Neonatal Intensive Care Unit: A multimodal intervention and impact on nosocomial infection.Pediatrics.2004 Nov;114(5):565-71. Sharek JP, Benitz WE, Abel NJ, Freeburn MJ, Mayer ML, Bergman DA. Effect of an evidence-based hand washing policy on hand washing rates and false-positive coagulase negative staphylococcus blood and cerebrospinal fluid culture rates in a level III NICU. J Perinatol. 2002 Mar;22(2):137-43. Won SP, Chou HC, Hsieh WS, Chen CY, Huang SM, Tsou KI, Tsao PN. (2004) Handwashing program for the prevention of nosocomial infections in a neonatal intensive care unit. Infect Control Hosp Epidemiol. 25(9):742-6.