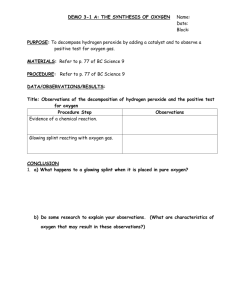
Chapter 37 Orthopedic Trauma 37-1
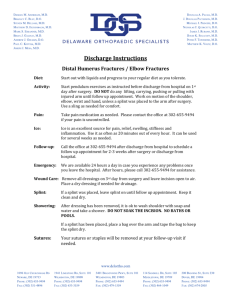
advertisement

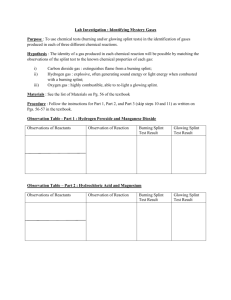
Chapter 37 Orthopedic Trauma Copyright (c) The McGraw-Hill Companies, Inc. Permission required for reproduction or display. 37-1 Objectives 37-2 Musculoskeletal System • Gives the body its shape • Provides a rigid framework that supports and protects internal organs • Provides for body movement • Maintains posture • Helps stabilize joints • Produces body heat 37-3 Skeletal System • Gives the body shape, support, and form • Works with muscles to provide for body movement • Stores minerals, such as calcium and phosphorus • Produces red blood cells • Protects vital internal organs 37-4 Axial Skeleton Skull Vertebral column Appendicular Skeleton (shown in blue) Shoulder girdle Sternum Pelvic girdle Ribs Limb bones 37-5 Skull • Cranial bones – Protect the brain • Upper jaw (maxilla) • Lower jaw (mandible) • Facial bones • Cheek (zygomatic) bones 37-6 Vertebral (Spinal) Column • Cervical – 7 vertebrae • Thoracic – 12 vertebrae • Lumbar – 5 vertebrae • Sacrum – 5 vertebrae (fused) • Coccyx – 3-4 vertebrae (fused) 37-7 Chest (Thorax) 37-8 Upper Extremities 37-9 Lower Extremities 37-10 Joints • Place where two bones come together • Some bone ends are covered with cartilage – Cartilage cushions bones • Held together by ligaments 37-11 Ball-and-Socket Joints • Allow movement in all directions 37-12 Hinge Joints • Allow only flexion and extension 37-13 Muscular System • Gives body shape • Protects internal organs • Provides body movement • Maintains posture • Helps stabilize joints • Produces body heat 37-14 Skeletal Muscles • • • • Move bones to which they are attached Produce heat Help maintain posture House a rich supply of blood vessels and nerves • Must receive a signal from a nerve in order to contract 37-15 Skeletal Muscles Three main parts: 1. Origin: Stationary attachment of muscle to bone 2. Insertion: Movable attachment to a bone 3. Body: Main part of the muscle 37-16 Musculoskeletal Injuries 37-17 Mechanism of Injury (a) Direct force injury (b) Indirect force injury (c) Twisting force injury 37-18 Types of Musculoskeletal Injuries 37-19 Open and Closed Injuries • Open injury – Skin surface is broken – Can result in serious blood loss – Increased risk of contamination and infection • Closed injury – Skin surface is not broken 37-20 Growth (Epiphyseal) Plate 37-21 Fractures 37-22 Open Femur Fracture 37-23 Dislocation Dislocation of the right hip joint. (a) Anterior view. (b) Frontal section. 37-24 Knee Dislocation 37-25 Sprain • Stretching or tearing of a ligament • Pain and bruising usually present • May be mild, moderate, or severe 37-26 Strain • Twisting, pulling, or tearing of a muscle • Signs and symptoms – Pain with movement – Little or no swelling – Limited ability to bear weight – Tender to the touch – Possible bruising 37-27 Patient Assessment • Scene safety • Assess the mechanism of injury • Put on appropriate personal protective equipment • Perform a primary survey 37-28 Patient Assessment • Quickly determine if the patient’s injury is life or limb-threatening. • Classes of patients with musculoskeletal trauma: 1. Patients with life/ limb-threatening injuries or conditions, including life/ limbthreatening musculoskeletal trauma 37-29 Patient Assessment 2. Patients with other life/ limb-threatening injuries and only simple musculoskeletal trauma 3. Patients with life/ limb-threatening musculoskeletal trauma and no other life/ limb-threatening injuries 4. Patients with only isolated, non-life/ limbthreatening injuries 37-30 Patient Assessment • Treat all life-threatening conditions first • Then address limb-threatening injuries. • If signs of shock are present or if internal bleeding is suspected, treat for shock. • Provide care for non-life/limb threatening injuries as time permits. 37-31 Patient Assessment • The 6 P’s of musculoskeletal assessment: 1. Pain or tenderness (on palpation, movement) 2. Pallor 3. Paresthesia (pins and needles sensation) 4. Pulses (present, diminished, absent) 5. Paralysis (inability to move) 6. Pressure (swelling/edema) 37-32 Emergency Care • Secondary survey – DCAP-BTLS – PMS • Vital signs, medical history 37-33 Emergency Care – Put on appropriate PPE – Keep on-scene time to a minimum – Spinal precautions, if appropriate – Establish and maintain an open airway – Give oxygen 37-34 Emergency Care • Apply a cold pack to the injured area • Dress open wounds • Splint bone or joint injuries – Support joints above and below the injured bone – Support bones above and below the injured joint 37-35 Emergency Care of Sprains and Strains • Rest • Ice • Elevation 37-36 Splinting 37-37 Splinting • Splint – Device used to limit movement of a body part to reduce pain and further injury 37-38 Reasons for Splinting • To limit the motion of bone fragments, bone ends, or dislocated joints • To lessen damage to muscles, nerves, or blood vessels • To help prevent a closed injury from becoming an open injury • To lessen the restriction of blood flow caused by bone ends or dislocations compressing blood vessels • To reduce bleeding • To reduce pain • To reduce the risk of paralysis caused by a damaged spine 37-39 Hazards of Improper Splinting • Compression of nerves, tissues, and blood vessels • Transport delay • Reduced distal circulation from a splint that is too tight • Aggravation of the musculoskeletal injury • Causing or worsening tissue, nerve, vessel, or muscle damage 37-40 Principles of Splinting • Take standard precautions and wear appropriate PPE • Remove or cut away clothing to expose the injury • Remove jewelry from the injured area • Assess pulses, movement, and sensation distal to the injury before and after splinting • Cover open wounds with a sterile dressing 37-41 Principles of Splinting • Pad a rigid or a semi-rigid splint • Splint the area above and below the injury – Splint joints above and below the injured bone – Splint bones above and below the injured joint 37-42 Position of Function 37-43 Principles of Splinting • Pad the hollow areas (voids) between the splint and the extremity • Do not intentionally replace protruding bones • Avoid excessive movement of the injured area • Avoid placing ties or straps directly over the injury • Splint the injury before moving the patient unless the patient is in danger or lifethreatening conditions exist 37-44 Principles of Splinting • When in doubt about whether or not a musculoskeletal injury is present, splint • If the patient shows signs of shock: – Align the patient in the anatomical position on a long backboard – Treat for shock – Transport 37-45 Types of Splints 37-46 Rigid Splints 37-47 Semi-Rigid Splints 37-48 Soft Splints 37-49 Traction Splints 37-50 Pneumatic Splints 37-51 Warning Signs that a Splint Is Too Tight • • • • • • Fingers or toes become cold to the touch Fingers or toes begin to turn pale or blue Inability to move fingers or toes Increased pain Increased swelling below the splint Patient complains of: – Numbness or tingling – Burning or stinging 37-52 Upper Extremity Injuries 37-53 Shoulder Injuries • Shoulder injury typically involves three bones: – Collarbone (clavicle) – Shoulder blade (scapula) – Upper arm bone (humerus) • Patient usually holds arm in a position of comfort – Immobilize the injury in this position • Sling and swathe usually used for this injury 37-54 Immobilization of a Shoulder Injury 37-55 Immobilization of a Shoulder Injury 37-56 Immobilization of a Shoulder Injury 37-57 Immobilization of a Shoulder Injury 37-58 Immobilization of a Shoulder Injury 37-59 Immobilization of the Humerus 37-60 Immobilization of the Elbow 37-61 Immobilization of the Forearm or Wrist 37-62 Immobilization of the Hand 37-63 Immobilization of the Fingers 37-64 Lower Extremity Injuries 37-65 Immobilization of the Pelvis or Hip 37-66 Immobilization of the Hip 37-67 Immobilization of the Femur 37-68 Immobilization of the Femur • Traction splint – Applying traction: • Stabilizes bone ends • Reduces pain • Reduces the likelihood of a closed fracture becoming an open one • Reduces further soft-tissue damage 37-69 Application of the SEFRS Adaptor 37-70 Application of the SEFRS Adaptor 37-71 Application of the SEFRS Adaptor 37-72 Application of the SEFRS Adaptor 37-73 Application of the SEFRS Adaptor 37-74 Application of the SEFRS Adaptor 37-75 Application of the SEFRS Adaptor 37-76 Application of the SEFRS Adaptor 37-77 Application of the SEFRS Adaptor 37-78 Application of the SEFRS Adaptor 37-79 Applying the Sager SX Unipolar Traction Splint 37-80 Applying the Sager SX Unipolar Traction Splint 37-81 Applying the Sager SX Unipolar Traction Splint 37-82 Applying the Sager SX Unipolar Traction Splint 37-83 Applying the Sager SX Unipolar Traction Splint 37-84 Applying the Sager SX Unipolar Traction Splint 37-85 Applying the Sager SX Unipolar Traction Splint 37-86 Applying the Sager SX Unipolar Traction Splint 37-87 Applying the Sager SX Unipolar Traction Splint 37-88 Applying the Sager SX Unipolar Traction Splint 37-89 Applying the Sager SX Unipolar Traction Splint 37-90 Applying a Bipolar Traction Splint 37-91 Applying a Bipolar Traction Splint 37-92 Applying a Bipolar Traction Splint 37-93 Applying a Bipolar Traction Splint 37-94 Applying a Bipolar Traction Splint 37-95 Applying a Bipolar Traction Splint 37-96 Applying a Bipolar Traction Splint 37-97 Applying a Bipolar Traction Splint 37-98 Applying a Bipolar Traction Splint 37-99 Immobilization of the Knee 37-100 Immobilization of the Knee 37-101 Immobilization of the Lower Leg 37-102 Immobilization of the Ankle or Foot 37-103 Questions? 37-104