Chapter 11 Emergency Medications 11-1
advertisement

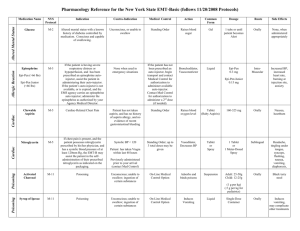
Chapter 11 Emergency Medications Copyright (c) The McGraw-Hill Companies, Inc. Permission required for reproduction or display. 11-1 Objectives 11-2 Administered Medications 11-3 Administered Medications • • • • Activated charcoal Aspirin Oral glucose Oxygen 11-4 Activated Charcoal 11-5 Activated Charcoal • Generic name – activated charcoal • Trade names – Liqui-Char, Actidose, InstaChar, SuperChar, and others • Activated charcoal can only bind a drug that is not yet absorbed from the gastrointestinal tract 11-6 Activated Charcoal Action • Acts as an adsorbent • Binds with many (but not all chemicals) • Slows down or blocks absorption of the chemical 11-7 Activated Charcoal Indications • Some ingested poisons 11-8 Activated Charcoal Contraindications • Patient has an altered mental status • Patient is unable to swallow • Medical direction does not give authorization • Patient has ingested acids or alkalis 11-9 Activated Charcoal Adverse Effects • Abdominal cramping • Constipation • Black stools • Nausea, vomiting 11-10 Activated Charcoal Dosage • Dosage – 1 gram of activated charcoal per kilogram of body weight – Usual adult dose: 25 to 50 grams – Usual infant/child dose: 12.5 to 25 grams 11-11 Activated Charcoal • Before giving activated charcoal, you must determine if your patient can follow directions and swallow safely. • Activated charcoal looks like tar, stains any material with which it comes in contact, and doesn’t taste good. – Be prepared for the patient to spit out the medication. 11-12 Giving Activated Charcoal 11-13 Giving Activated Charcoal 11-14 Giving Activated Charcoal 11-15 Giving Activated Charcoal 11-16 Aspirin 11-17 Aspirin • Generic name – Acetylsalicylic acid • Trade names – Bayer, Ecotrin, Empirin, and others • Nonnarcotic pain reliever • Fever reducer • Anti-inflammatory medication 11-18 Aspirin Action • Inhibits platelet clumping, thus interfering with blood clotting 11-19 Aspirin Indications • Chest pain or other signs/symptoms suspected to be of cardiac origin – (Unless hypersensitive to aspirin) • If ordered by medical direction, aspirin should be given as soon as possible after the patient’s onset of chest discomfort. 11-20 Aspirin Contraindications • Known allergy or sensitivity to aspirin • Bleeding ulcer or bleeding disorders • Children and adolescents 11-21 Aspirin Adverse Effects • • • • • Rapid pulse Flushing Wheezing Nausea, vomiting Gastrointestinal bleeding • Diarrhea • Heartburn • Loss of appetite • Ringing in the ears (tinnitus) • Rash • Hives • Bruising 11-22 Aspirin Dosage • Adult – Two to four 81-mg tablets (baby aspirin), chewed and swallowed 11-23 Aspirin Special Considerations • Use with caution in a patient who has any of the following: – Asthma – Nasal polyps – Nasal allergies 11-24 Aspirin Administration • Open the container • Pour the correct number into the inside cap of the container • Transfer the tablets by pouring them into the patient’s hand – Do not to contaminate the inside cap of the container • Carefully recap the container 11-25 Oral Glucose 11-26 Oral Glucose Action • When administered, oral glucose increases the amount of sugar available for use as energy by the body. 11-27 Oral Glucose Indications • Patients with an altered mental status who have a known history of diabetes controlled by medication and can swallow 11-28 • • • • Oral Glucose Contraindications Medical direction does not give permission Unresponsive Unable to swallow Known allergy to the glucose preparation 11-29 Oral Glucose Adverse Effects • Nausea • May be aspirated by the patient without a gag reflex 11-30 Oral Glucose Dosage • One tube 11-31 Oral Glucose Special Considerations • Ensure signs and symptoms of altered mental status with a known history of diabetes • Make sure the patient is responsive, can swallow, and can protect his airway • Obtain order from medical direction • Use appropriate personal protective equipment • Practice the six rights of drug administration 11-32 Giving Oral Glucose 11-33 Giving Oral Glucose 11-34 Giving Oral Glucose 11-35 Giving Oral Glucose 11-36 Oxygen 11-37 Oxygen Action • Giving oxygen increases the amount available in the bloodstream for use by the body’s cells 11-38 Oxygen Indications • Cardiac or respiratory arrest • Suspected low oxygen levels from any • Any suspected cardiopulmonary emergency, especially complaints of shortness of breath or chest pain 11-39 Oxygen Adverse Effects • May reduce the respiratory drive in some patients with chronic obstructive pulmonary disease • Drying of the mucous membranes 11-40 Oxygen Dose • Nasal cannula – 1 to 6 L/min • Nonrebreather mask – 15 L/min • Cardiac or respiratory arrest: positive-pressure ventilation with 100% oxygen 11-41 Assisted Medications 11-42 Assisted Medications • An EMT can assist a patient in taking the following physician-prescribed medications when authorized by medical direction: – Epinephrine auto-injector – Inhaled bronchodilators – Nitroglycerin 11-43 Epinephrine 11-44 Epinephrine • Generic name – epinephrine • Trade name – Adrenalin 11-45 Epinephrine Actions • Relaxes the bronchial passages of the airway • Constricts blood vessels 11-46 Epinephrine Indications • All of the following criteria must be met: – Patient shows signs and symptoms of a severe allergic reaction – Epinephrine is prescribed for patient or EMS system authorizes you to carry it – Medical direction authorizes use for the patient 11-47 Epinephrine Contraindications • There are no contraindications when an epinephrine auto-injector is used in a life-threatening situation 11-48 Epinephrine Adverse Effects • Rapid heart rate • Anxiety • Excitability • Nausea, vomiting • Chest pain or discomfort • Headache • Dizziness 11-49 Epinephrine Dosage • Adult – One adult auto-injector (0.3 mg) • Infant and child – One infant/child auto-injector (0.15 mg) 11-50 Epinephrine Special Considerations • Use appropriate personal protective equipment • Practice the six rights of medication administration. • Use a pulse oximeter • Give oxygen by nonrebreather mask • Assess lung sounds 11-51 Epinephrine Special Considerations 11-52 Epinephrine Auto-Injector Procedure 11-53 Epinephrine Auto-Injector Procedure 11-54 Epinephrine Auto-Injector Procedure 11-55 Epinephrine Auto-Injector Procedure 11-56 Epinephrine Auto-Injector Procedure 11-57 Epinephrine Auto-Injector Procedure 11-58 Inhaled Bronchodilators 11-59 Prescribed Metered-dose Inhaler 11-60 Inhaled Bronchodilators Action • Generic (trade) names – albuterol (Proventil, Ventolin) – isoetharine (Bronkosol) – metaproterenol (Alupent, Metaprel) • Dilate bronchioles, reducing airway resistance 11-61 Inhaled Bronchodilators Indications • An EMT can assist a patient in taking a prescribed inhaler if all of the following criteria are met: – Patient has signs and symptoms of a respiratory emergency – Patient has a physician prescribed handheld inhaler – No contraindications to giving the medication – Specific authorization by medical direction 11-62 Inhaled Bronchodilators Contraindications • The patient is unable to use the device. • The inhaler is not prescribed for the patient. • Permission is not received from medical direction. • The patient has already met the maximum prescribed dose before your arrival. 11-63 Inhaled Bronchodilators Adverse Effects • Increased heart rate • Nausea • Shaking or tremors • Headache • Restlessness • Dizziness • Nervousness 11-64 Inhaled Bronchodilators Dosage • Number of inhalations based on medical direction’s order or physician’s order based upon consultation with the patient 11-65 Inhaled Bronchodilators Special Considerations • Use appropriate personal protective equipment. • Practice the six rights of medication administration. • Assist the patient in finding his MDI if it is not readily available. • Assess lung sounds • Reassess vital signs and patient’s degree of breathing difficulty. 11-66 Inhaled Bronchodilators 11-67 Inhaled Bronchodilators 11-68 Inhaled Bronchodilators 11-69 Inhaled Bronchodilators 11-70 Inhaled Bronchodilators 11-71 Inhaled Bronchodilators 11-72 Nitroglycerin 11-73 Nitroglycerin • Generic name – nitroglycerin • Trade names – Nitrostat, Nitrobid, Nitrolingual, Nitroglycerin Spray • Action – Relaxes (dilates) the smooth muscle of blood vessel walls – Decreases the workload of the heart 11-74 Nitroglycerin Indications • An EMT can assist a patient in taking nitroglycerin if all of the following criteria are met: – Patient has signs and symptoms of chest discomfort suspected to be of cardiac origin – Patient has physician prescribed sublingual tablets or spray – No contraindications – Specific authorization by medical direction 11-75 Nitroglycerin Contraindications • • • • • • • • Medical direction does not give permission Medication is not prescribed for the patient Patient has taken maximum prescribed dose Blood pressure below 100 mm Hg systolic Heart rate <50 beats/min or >100 beats/min Head injury (recent) or stroke (recent) Infants and children Erectile dysfunction drug within last 24-48 hours 11-76 Nitroglycerin Adverse Effects • Hypotension • Headache • Tachycardia • Palpitations • Bradycardia • Fainting 11-77 Nitroglycerin Dosage • One tablet or one spray under the tongue • Dose may be repeated in 3 to 5 minutes (maximum of three doses) if: – Patient experiences no relief, – Patient’s systolic blood pressure remains above 100 mm Hg systolic – Patient’s heart rate remains between 50 and 100 beats/minute – No other contraindications – Medical direction okays another dose 11-78 Nitroglycerin Special Considerations • Recheck the patient’s vital signs within two minutes. • Reassess the patient’s degree of discomfort. 11-79 Assisting with Prescribed Nitroglycerin 11-80 Assisting with Prescribed Nitroglycerin 11-81 Assisting with Prescribed Nitroglycerin 11-82 Assisting with Prescribed Nitroglycerin 11-83 Assisting with Prescribed Nitroglycerin 11-84 Assisting with Prescribed Nitroglycerin 11-85 Assisting with Prescribed Nitroglycerin 11-86 Assisting with Prescribed Nitroglycerin 11-87 Special Situations 11-88 Nerve Agents • Chemical weapons • Interrupt nerve signals causing a loss of consciousness within seconds and death within minutes of exposure 11-89 Antidote • An antidote is a substance that neutralizes a poison. • Nerve agent antidotes 11-90 Signs/Symptoms of Nerve Agent Exposure Mild – Tearing – Unexplained runny nose 11-91 Signs / Symptoms Moderate – Drooling – Excessive sweating – Nausea and/or vomiting – Abdominal cramps – Diarrhea – Tightness in chest – Muscle twitching at site of exposure – Pinpoint pupils resulting in blurred vision – Difficulty breathing, shortness of breath, wheezing 11-92 Signs / Symptoms Severe • Strange or confused behavior • Severe difficulty breathing or severe secretions from the airway • Muscle twitching, jerking, staggering • Drowsiness • General weakness • Headache • Involuntary urination • Involuntary defecation • Seizures • Apnea • Unconsciousness 11-93 Nerve Agent Antidotes • Atropine sulfate • Pralidoxime chloride • Packaged in auto-injectors – Mark I™ kits 11-94 Nerve Agent Antidotes • Mark I™ kit – Contains two separate auto-injectors • One for atropine • One for pralidoxime chloride 11-95 Nerve Agent Antidotes • DuoDote™ – Approved by the FDA in 2007 – Prefilled auto-injector – Delivers atropine and pralidoxime chloride in one intramuscular injection 11-96 Atropine Action • Reverses some effects of nerve agent poisoning – Increases heart rate – Relaxes bronchioles – Dries secretions – Decreases gastric motility – Dilates pupils 11-97 Atropine Indications • An EMT can self-administer or administer an atropine auto-injector to a peer if all of the following criteria are met: – The EMT or a peer has signs and symptoms consistent with nerve agent exposure. – The EMT has specific authorization by medical direction. 11-98 Atropine Contraindications • None – in the face of life-threatening poisoning by chemical nerve agents 11-99 Atropine Adverse Effects • Pain at site of injection • Dryness of the mouth • Blurred vision • Confusion • Headache • Dizziness • • • • Tachycardia Palpitations Flushing Urinary hesitance or retention • Constipation • Nausea, vomiting 11-100 Atropine Dosage • Adult – One auto-injector, which contains about 2 mg of atropine in 0.7 mL 11-101 Atropine Special Considerations • More than one dose may be necessary 11-102 Pralidoxime Chloride Action • Generic name: pralidoxime chloride • Trade name: 2-PAM Chloride • Action – Reverses some effects of nerve agent poisoning • Muscle twitching • Difficulty breathing 11-103 Pralidoxime Chloride Indications • An EMT can self-administer or administer a 2-PAM auto-injector to a peer if all of the following criteria are met: – The EMT or a peer has signs and symptoms consistent with nerve agent exposure. – The EMT has specific authorization by medical direction. 11-104 Pralidoxime Chloride Contraindications • None in the face of life-threatening poisoning by chemical nerve agents 11-105 Pralidoxime Chloride Adverse Effects • • • • • • Pain at injection site Tachycardia Hypertension Muscle weakness Nausea Blurred or double vision • Dizziness • Loss of coordination • Headache • Drowsiness 11-106 Pralidoxime Chloride Dosage • Dosage (adult) – One auto-injector contains 600 mg pralidoxime chloride in 2 mL 11-107 Pralidoxime Chloride Special Considerations • Three kits used for severe symptoms 11-108 Diazepam (Valium) • Used to control seizures following severe exposure to nerve agents (and similar toxins) • May be carried in a single auto-injector – Convulsant Antidote for Nerve Agent (CANA) 11-109 Diazepam (Valium) Action / Indications • Action – Relaxes skeletal muscle and controls seizures • Indications – Seizures that persist after three Mark I (or DuoDote) kits have been given and the EMT has specific authorization by medical direction 11-110 Diazepam (Valium) Contraindications • Hypersensitivity to any component of the product 11-111 Diazepam (Valium) Adverse Effects • • • • • Pain at injection site Dizziness Drowsiness Confusion Respiratory depression 11-112 Diazepam (Valium) Dosage • One auto-injector contains 10 mg of diazepam 11-113 Diazepam (Valium) Special Considerations • Relatively short-acting drug – Seizure activity may recur • Onset of action is about 15 to 30 minutes • Monitor blood pressure, pulse, and respiratory rate every 5 minutes. 11-114 Questions? 11-115