Encephalitis & meningoencephalitis
advertisement

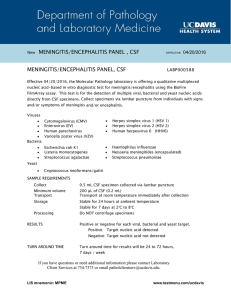
Assist Prof Microbiology Dr. Syed Yousaf Kazmi LEARNING OBJECTIVES 1. List the causes of encephalitis and meningo-encephalitis 2. Discuss pathogenesis of HSV encephalitis, rabies encephalitis and Primary Amoebic meningoencephalitis 3. Explain mechanism of transmission of HSV, rabies and Primary Amoebic meningoencephalitis 4. Discuss laboratory diagnosis of rabies encephalitis and meningo-encephalitis 5. Explain the role of immunization in primary and secondary prevention in rabies encephalitis ENCEPHALITIS & MENINGOENCEPHALITIS-ETIOLOGY FAMILY EXAMPLES DISEASE Herpesvirus Herpes simplex virus 1 &2 Herpes virus encephalitis Enterovirus Enterovirus Viral Encephalitis Retroviruses HIV HIV Dementia Arboviruses West Nile virus, St Louis Encephalitis Rhabdoviridea Rhabdovirus Rabies encephalitis Protozoa Naegleria fowleri, Acanthamoeba Primary amoebic meningo-encephalitis Others Measles, Mumps, Rubella, Polio, Influenza ,VZV Post infectious encephalitis Bacterial causes Syphilis, Mycobacterium, Lyme disease Bacterial encephalitis HERPES SIMPLEX INTRODUCTION HSV 1 & 2 belongs to Herpes virus (DNA Virus) Sexually Transmitted Infection usually HSV1 usually above waist (gingivo-stomatitis, keratitis, encephalitis) while HSV2 below waist(genital herpes) Notorious for Latent Infection Genome in human DNA in sensory ganglion Primary infection & Recurrent illness Herpes labialis very common recurrent disease HERPES SIMPLEX ENCEPHALITIS TRANSMISSION Through saliva, skin blisters, genital sores Active lesions important Asymptomatic virus shredding also common Sexual as well as intimate contact e.g. kissing on skin with herpes lesion Herpes labialis HERPES SIMPLEX ENCEPHALITIS PATHOGENESIS Virus multiplies in skin/ mucous membrane Migrates up the neuron by retrograde axonal flow Becomes latent in sensory nerve ganglion (usually Trigeminal ganglion) Viral DNA in cytoplasm of ganglion during latency HERPES SIMPLEX ENCEPHALITIS Reactivation factors-sunlight, hormonal changes (e.g. menstruation), trauma, stress, and fever Reactivation-viral particles migrate down neuron and produce skin lesions In certain cases, virus enters brain during reactivation period producing encephalitis Primary infection can directly infect brain producing encephalitis HERPES SIMPLEX ENCEPHALITIS HSV encephalitis is very severe illness Diagnosis is aided by past history of HSV infection or active lesion CSF findings are same as viral meningitis except 10–500 RBCs/mm3 PCR for HSV RNA in CSF is positive High mortality rate and severe neurological damage in survivor RABIES Rabies is caused by Enveloped RNA Virus Rhabdoviridea family, Lyssavirus genus Single antigenic type Extremely sensitive to sunlight, uv light, heat, lipid solvents (e.g., ether), alcohol, detergents, soap Sylvatic cycle-foxes, coyotes, wolves, skunks, raccoons, opossums, hyaena, dogs, cats etc. and bats Urban cycle-dogs, cats, monkeys, camel, horses, etc. RABIES-TRANSMISSION All warm blooded animals including humans can be infected Virus is present in saliva of animal with rabies Encephalitis affects limbic system-emotionally unstable- important in transmission of disease Rabid animal bites unprovoked Virus transmitted through wound via saliva Also transmitted by organ transplants e.g. cornea, kidney etc. RABIES-PATHOGENESIS Binds Acetylcholine receptor Multiplies in muscle/ connective tissue locally Enters sensory nerves-moves by axonal transport to the central nervous system Sheltered from immune system Encephalitis –diffuse demyelination and neuron death- Negri bodies Travels down the peripheral nerves to salivary gland, kidney, heart etc. RABIES-PATHOGENESIS Incubation period is variable (2 -16 weeks or >) Bites on face/ head, children, multiple deep wounds short incubation period nonspecific symptoms such as fever, anorexia, and changes in sensation at the bite site confusion, lethargy, and increased salivation develop Hydrophobia-painful spasm of throat muscles Emotional, violent, aggressive, hellucination Death is inevitable once symptoms of rabies develop RABIES-LAB DIAGNOSIS RABIES ANTIGENS OR NUCLEIC ACIDS Immunofluorescence or immunoperoxidase staining Biopsy specimen -skin of the neck at the hairline Impression preparations of brain or cornea tissue Negri bodies in the brain-80% positivity RT-PCR test on brain tissue specimen Negri Body VIRAL ISOLATION tissue is inoculated intra-cerebrally into suckling mice SEROLOGY Serum/ CSF anti-rabies Ab by immunofluorescence ANIMAL OBSERVATION Rabies immunofluorescence test RABIES-PROPHYLAXIS PRE-EXPOSURE PROPHYLAXIS HDCV (Human Diploid Cell Vaccine) Inactivated virus High-risk groups e.g. Veterinarians, Zookeepers, and Travelers to areas of hyper-endemic infection Three doses given on days 0, 7, and 21 or 28 POST EXPOSURE PROPHYLAXIS After person is exposed to virus Thorough cleaning of wound by soap/ detergent/ alcohol/ povidon iodine etc. THIS MAY BE LIFE SAVING ACT RABIES-PROPHYLAXIS HDCV given in Deltoid region, anterolateral thigh but never in gluteal region Intramuscular/ Intradermal routes 0,3,7,21,28 (optional at 90 day) Antibody titers checked for efficacy RABIES IMMUNE GLOBULIN, HUMAN (HRIG) The nature of the biting animal, the availability of the animal for laboratory examination, the existence of rabies in the area, the manner of attack (provoked or unprovoked), severity of the bite 20 IU/kg, half infiltrated around wound and half I/M SHORT MOVIE PRIMARY AMOEBIC MENINGO-ENCEPHALITIS Free living ameoba-Naegleria fowleri, Acanthamoeba Fresh water, lakes, ponds, un-chlorinated swimming pools, other warm water sources Do not require any human/ animal host for completion of life cycle Human infection is accidental Rare but serious disease of meninges and brain Around and more than 90 % fatal even with timely diagnosis and treatment PRIMARY AMOEBIC MENINGO-ENCEPHALITIS TRANSMISSION Swimming, diving, other sports activity in fresh water of ponds, lakes etc. Trophozoites/ flaggellate form in fresh warm water World wide distribution Young immuno-competent individuals Forceful entry of water in nostrils No human to human cases PRIMARY AMOEBIC MENINGO-ENCEPHALITIS PATHOGENESIS Amoeba enters nose and through cribriform plate pass into brain Very thin bone Causes meningo-encephalitis Brain oedema Brain pathology is indistinguishable from other encephalitis/ meningitis PRIMARY AMOEBIC MENINGO-ENCEPHALITIS LABORATORY DIAGNOSIS Clinical suspicion very important CSF findings may be equivocal or similar to other cases of bacterial/ viral meningitis Cells may be Neutrophils and lymphocytes/ monocytes Trophozoites might be read as monocytes by electronic counter Fresh CSF wet film examination will show motile trophozoites/ flagellate form Wet film exam of CSF showing Naegleria SHORT VIDEO