Bacterial infections of GIT
advertisement
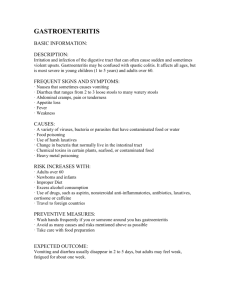
BACTERIAL INFECTIONS OF GIT Assistant Professor Microbiology Syed Yousaf Kazmi College of Medicine, Majmaah University OBJECTIVES 1. Maj Bacteria causing GIT Infections, epidemiology, etiology and pathogenesis 2. Mechanism of transmission, Enlist clinical conditions 3. Discuss laboratory diagnosis INTRODUCTION • Digestive system-maj route of entry of pathogen • Local defenses are strong to keep infection away o Mechanical & Physiological o Immunity (MALT etc) o Microbial Flora • Digestive diseases are usually associated with: o Crowding o Poor hygiene o Contaminated food or water INTRODUCTION • GIT Infections are of two types o Exogenous infection-where org are introduced from outside o Endogenous infection-where infection is associated due to normal flora • Endogenous infections are caused by organisms that are part of the normal flora. o Viridans Streptococcus, Actinomyces isreali • In the right circumstances they can cause: o Dental diseases. o Infections of the bowel, appendix, and liver. o Diverticular abscesses. CLINICAL CONDITIONS 1. GASTROENTERITIS a. Non inflammatory (No WBCs in stool) b. Inflammatory (WBCs in stool) c. Invasive (WBCs, RBCs, Mucus in stool) 3. FOOD POISONING 4. DYSENTERY 5. ENTEROCOLITIS, PSEUDOMEMBRANOUS COLITIS 6. 7. 8. 9. PEPTIC ULCER DISEASE DIVERTICULITIS APPENDICITIS DENTAL CARIES, PERIODONTITIS GASTROENTERITIS • Most infections of GIT are Gastroenteritis • Mainly of two types o Intoxication (Ingestion of toxins) e.g. Staph aureus, Bacillus cereus, Clostridium perfringens o Infections ( Ingestion of bacteria) e.g. Vibrio cholerae, Shigellosis, Campylobacter jejuni • Modes of contamination of food or water • • • • Many microbes are present in healthy animal’s intestinecontaminate during slaughter e.g. Campylobacter spp, Salmonella spp Washing of fruits/ veg with contaminated water Hands of food handler Sewage contamination of drinking water NON INFLAMMATORY GASTROENTERITIS INTOXICATIONSTAPH AUREUS • Gram positive cocci, Catalase & coagulase +ve • Secretes enterotoxin • Food contaminated from boil/ abscess of food handler or from nose during sneeze • Type of food meat, fish, cream filled pastries, egg salad • Incubation Period 1-6hrs • Nausea, vomiting, abdominal cramps, diarrhea • Mnemonic: (Staph starts with S, Shank for vomiting) INTOXICATIONCLOSTRIDIUM PERFRINGENS C. pergringens-Obligate anerobe, Gram +ve spore forming rod Protein rich food-beef, poultry, fish, Survive cooking-germinate & secrete enterotoxin Moderate to severe abdominal cramps, diarrhea Recovery usually in 1-2 days Antimicrobials usually not req Mnemonic C. perf starts with C, C for Commode INTOXICATIONBACILLUS CEREUS • Gram +ve spore forming rod • Spores germinate after reheating of rice/ Chinese food • Vomiting after 2-6 hours • Recovery in 2-3 days • Antimicrobials usually not req INFLAMMATORY GASTROENTERITIS INFECTIONVIBRIO CHOLERAE • Gram –ve curved rod • Contaminated water or raw seafood • Extremely susceptible to acid • 105 -108 org req • Release toxin-enterocytes ↑cAMP-loss of water & electrolytes • Profuse vomiting and diarrhea (rice water stool) • Extreme dehydration • Renal failure, acidosis- death INFECTION-ESCHERICHIA COLI • Gram –ve facultative anaerobe • Normal fecal flora but various serotypes can be pathogenic • Enterotoxigenic E. coli (ETEC) T for Traveller o o o o o Commonest cause of Traveller’s diarrhea Secrete enterotoxins like cholera Eating of raw veg, fruits, drinking unhygienic water Diarrhea, vomiting, abd cramps, fever Diarrhea last for 3-7 days • Enteropathogenic E. coli (EPEC) P for Pediatric o Diarrhea in infant o Associated with poor sanitation INVASIVE GASTROENTERITIS SHIGELLOSIS • Shigella spp are Gram –ve facultative anaerobe, non motile bacillus • Shigella dysenteriae most severe, Shigella sonnei most benign form • Outbreaks in school, daycares, etc. • Consumption of water or food e.g. eggs, veg, dairy products contaminated by food handler, flies, hands • Even 101 to 102 org can initiate infection • Acid resistant- reach colon- secrete toxin and invade epithelium • Blood, mucus, WBCs passed in stool • Severe diarrhea, tenesmus, vomiting, dehydration Stool exam shows WBCs, RBCs, non motile bacilli ENTERO-HEMORRHAGIC E. COLI • EHEC-H for Hemolytic Uremic Syndrome • Dangerous • Undercooked beef, unpasteurized milk, juices, lettuce, • 103 org can initiate infection • Release toxin in high conc in large intestine • Serotype O157:H7 secretes toxin- inhibits protein synthesis-cytolysis • Hemorrhagic colitis • Older, young children, weak immunity- HUS • Hemolysis, renal failure, seizure, coma, etc SALMONELLOSIS • Salmonella typhi causative agent of typhoid fever • Salmonella enterica serotype Enteritidis and serotype Typhimurium • Salmonella typhi source is humans, Salmonella enterica spp source is poultry chicken & turkeys • Transmitted through food handlers • IP 6-48 hours, nausea, diarrhea, abdominal pain, fever • Colonic ulceration • Infection lasts 3-7 days • Septicemia rare CAMPYLOBACTER JEJUNI • Gram negative motile curved bacillus • Normal gut flora of chicken, turkey, dairy cattle • Contaminated raw food, water, eggs, poultry • Fecal-oral route • IP 2-7 days – small /large intestine invasion • Ulceration of mucosa • Symptoms variable- mild to severe dysentery • Association with GB Syndrome weeks later (Markus Babbel liverpool) LAB DIAGNOSIS OF INFECTIVE GASTROENTERITIS • Clinical history • Appropriate Samples • Vomitus • Stool • Left over food • Blood • Microbiological Testing • Microscopy (Direct and after Gram staining) • Culture & Sensitivity of Stool, vomitus, left over food or blood • Blood complete picture • Toxin detection in stool or vomitus, food Cl. Perfringens in stool LAB DIAGNOSIS Campylobacter jejuni in stool Vibrio cholerae colonies on TCBS Toxin detection kit C. difficile PEPTIC ULCERHELICOBACTER PYLORI • • • • • • • • • Peptic ulcer –smoking, alcohol, diet, stress etc. Association of peptic ulcer with infectious etiology in 1982 Australians Dr. Barry J Marshall & J Robbin Warren believed that infection is responsible Microaerophilic Gram –ve curved rod, urease producer Person to person via food or water In stomach, attaches to stomach surfacesecrete urease- produces ammonia Locally pH ↑, neutralize acid, mucus cells destroyed Ulcer develop 2% of ulcer patients develop cancer Gastric ulcer HELICOBACTER PYLORI LAB DIAGNOSIS • Urea breath Test o Urea breath test- use radioactive C labeled urea o Patient drinks the sol- urea broken down by urease of H. pylori- CO2 released radiolabeled detected by special equipment • Serological tests like ELISA • Culture of gastric biopsy • Rapid urease test of gastric biopsy