Management of Orofacial Pain
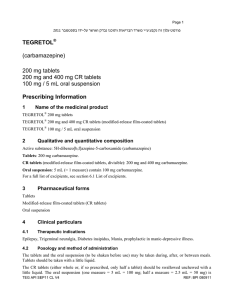
advertisement

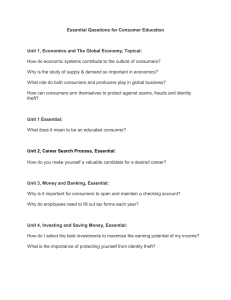
Dr. Rupak Sethuraman SPECIFIC LEARNING OBJECTIVES Various management techniques of orofacial pain Management of common orofacial pain disorders VARIOUS TREATMENT MODALITIES 1. Cognitive behavioral therapy- attempts to alter patterns of negative thoughts and to bring about more healthy and adaptive thoughts, emotions, and actions. 2. Relaxation therapy- More significant in reducing the distress associated with pain. 3. Drug therapy- Four categories of drugs are widely used: Non steroidal anti inflammatory drugs (NSAIDs) Opioid analgesics Adjuvants such as anti convulsants Topical medications Management of trigeminal neuralgia (TN) Initial therapy for TN should consist of trials of drugs that are effective in eliminating the painful attacks. Anticonvulsant drugs are most frequently used and are most effective. Carbamazepine is the most commonly used drug and is an effective therapy for greater than 85% of newly diagnosed cases of TN. The drug is administered in slowly increasing doses until pain relief has been achieved. Skin reactions, including generalized multiforme, are serious side effects. erythema Patients receiving carbamazepine must have periodic hematologic laboratory evaluations because serious life threatening blood disorders may occur . Patients who do not respond to carbamazepine alone may obtain relief from baclofen or by combining carbamazepine with baclofen. Oxcarbamazepine is the 10-ketoanalogue of carbamazepine with a similar mode of action. Its principal advantage over carbamazepine is less liver toxicity and less risk of blood disorders. Other drugs that are effective for some patients include gabapentin, phenytoin, lamotrigine, baclofen, topiramate, and pimozide. Since TN may have temporary or permanent spontaneous remissions, drug therapy should be slowly withdrawn if a patient remains pain free for 3 months. Management of post herpetic neuralgia (PHN) Prevention of PHN is now possible, and use of a varicella-zoster vaccine for patients over 60 years of age significantly reduces the incidence of herpes zoster and the sequelae of PHN. For patients who develop herpes zoster, use of antiviral drugs early in the course of the disease reduces the risk of PHN. For patients who develop PHN, the method of treatment chosen should depend on the severity of the symptoms and the general medical status of the patient. Treatment includes topical therapy, drug therapy, and surgery. Topical therapy includes the use of topical anesthetic agents, such as lidocaine, or analgesics, particularly capsaicin. Capsaicin, an extract of hot chilli peppers that depletes the neurotransmitter substance P when used topically, has been shown to be helpful in reducing the pain of PHN, but the side effect of a burning sensation at the site of application limits its usefulness for many patients. The use of Tricyclic Anti Depressants (TCAs) such as amitriptyline, nortriptyline, doxepin, and desipramine is a well-established method of reducing the chronic burning pain that is characteristic of PHN. Management of Burning Mouth Syndrome (BMS) Once the diagnosis of BMS has been made by eliminating the possibility of detectable lesions or underlying medical disorders, the patient should be reassured of the benign nature of the symptoms. Counseling the patient in regard to the nature of BMS is helpful in management, particularly because many patients will have had multiple clinical evaluations without an explanation for the symptoms. Counseling and reassurance may be adequate management for individuals with mild burning sensations, but patients with symptoms that are more severe often require drug therapy. The drug therapies that have been found to be the most helpful are low doses of TCAs, such as amitriptyline and doxepin, or clonazepam (a benzodiazepine derivative). It should be explained to the patient that these drugs are being used not to manage psychiatric illness but for their analgesic effect. On the other hand, application of topical clonazepam was effective in reducing pain intensity; moreover, in another study, the positive effect was carried over up to 6 months following 2 weeks of treatment. A 2-month course of 600 mg daily of alpha-lipoic acid has been shown to reduce BMS pain, and systemic capsaicin (0.25% capsule 3 times per day for 30 days) demonstrated some positive effects on BMS pain intensity. Any Questions?? Thank you