محاضرة المسكنات في الولادة
advertisement

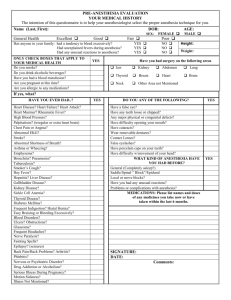
Obstetric Analgesia and Anesthesia Dr. Rayan G. Albarakati, MBBS, SB-OB Assistant Professor OB/GYN Head Of Obsterics & Gynecology Al Majmaah university The goal ? 1. Effective pain relief for the mother during the course of labor and delivery 2. That is safe for her and her baby 3. That has minimal adverse effects on the progress & outcome of labor. * Maternal mortality due to anesthesia has decreased to less than 1 in 500,000 mothers. Analgesia and Anesthesia • Analgesia: the relief of pain without loss of consciousness. • Anesthesia: Total or partial loss of sensation, especially tactile sensibility, induced by an anesthetic. Pain pathways of parturition: • T10 to L1 supply innervation to the uterus. • L1 to S4 supply pain pathways to the vagina and deep pelvic structures. • S2 to S4 supply nerve fibers to the pudendal nerve. Pain Path ways In Labor ADVERSE EFFECTS OF LABOR PAIN A) Maternal hyperventilation: B) Hyperventilation-hypoventilation: during contractions causes respiratory alkalosis that results in : The cyclical nature of contraction pain may cause this syndrome whereby the mother blows off so much carbon dioxide during a contraction that she hypoventilates between contractions and become mildly hypoxemic between contractions. (1) a shift of the oxyhemoglobin dissociation curve to the left. (2) increased affinity of maternal hemoglobin for oxygen. (3) decreased oxygen offloading to the fetus. The cyclical nature of contraction pain may cause a hyperventilation-hypoventilation syndrome whereby the mother blows off so much carbon dioxide during a contraction that she C) labor pain results in increased levels of circulating catecholamines: The α-adrenergic effects of the catecholamines may reduce uterine blood flow, whereas the β 2 -adrenergic effects may impair uterine contractility. OPTIONS FOR LABOR PAIN RELIEF A) Pharmacologic treatment options B) Nonpharmacologic methods • • • • • • • • • Parenteral narcotics Regional analgesia (epidural, spinal, combined spinal-epidural, paracervical, caudal, and pudendal nerve blocks) Inhalational analgesia • • Education and psychoprophylaxis Emotional support Back massage Hydrotherapy Biofeedback Transcutaneous electrical nerve stimulation Acupuncture Hypnosis (hypnobirthing). Parenteral narcotics • have very limited efficacy for the relief of labor pain. • They work best in the early first stage when the pain is primarily visceral and less intense. • All opioids readily cross the placental barrier and may cause neonatal respiratory depression depending on the dose and timing relative to delivery. • They may also cause decreased fetal heart rate variability and impair neonatal breastfeeding. • Fentanyl and nalbuphine have the shortest neonatal half-lives of the commonly used parenteral narcotics. Neuraxial analgesia • • • • • • • • The most effective form of labor pain relief. Lumbar epidural analgesia is the most common form of neuraxial analgesia used to treat labor pain Its use has been steadily increasing to 60 % nationally. It may be used to provide pain relief for the first and second stages of labor0 by injecting a higher concentration of local anesthetic, the block may be intensified and extended to provide surgical anesthesia for cesarean delivery or postpartum tubal ligation. Anesthetics (bupivacaine, ropivacaine, or lidocaine) Narcotics (fentanyl or sufentanil) . The goal is to avoid motor block to minimize any adverse effects on maternal expulsive efforts in the second stage. Pudendal Nerve Block • anesthetizes somatic afferent nerve fibers entering the spinal cord at sacral segments S2 to S4. • It is usually effective at relieving the perineal pain of the second stage of labor , along with the pain of episiotomy and episiotomy repair. • It does not affect the ongoing pain of uterine contractions. • Main complications: Nerve injury, hematoma, hypersensitivity. Pudendal Nerve Block in a trans-vaginal approach Inhalational anesthesia • Widely used analgesics for labor pain because of their: 1.Availability 2.Simplicity of administration 3.Low cost. 4.Safety • Their analgesic efficacy is limited compared with regional analgesia. • Nitrous oxide in oxygen (Entonox) provides moderate pain relief and is safe for use in labor Unintended Consequences of Regional Anesthesia or Analgesia • Delayed second stage of labor • Fever (0.5°C increased body temperature) • Headache: The risk is about 1% to 2% with spinal anesthesia, while in epidural it is (less than 1%). • Backache** • Hypotension ** The risk for new, chronic back pain in parturients is high (up to 47%) whether or not they have had an epidural Delayed second stage of labor 1. Effects of the release of endogenous oxytocin, prostaglandin F2a hormones responsible for the propagation of labor. 2. Impaired ability to push (unlikely as long as motor block is avoided). 3. Decreased maternal urge to push due to sensory blockade. Fever • • an alteration in the thermoregulatory threshold interference with peripheral thermoreceptor input to the central nervous system • shifting heat calories from the core to the periphery by vasodilation • an imbalance between maternal heat production and loss (decreased hyperventilation, decreased lower body sweating, increased shivering). Postdural puncture headaches • • • • These are self-limited • usually resolving within 5 to 7 days. Cerebrospinal fluid leaks through the hole in the dura, resulting in low intracranial pressure. The hallmark is a severe positional headache —little or no headache supine, sudden onset of severe headache when sitting upright or standing. • The dural hole will heal in about 1 week or can be sealed with an epidural blood patch. Symptomatic treatment includes narcotics, nonsteroidal antiinflammatory drugs, caffeine, sumatriptan, and abdominal binder. Contraindications to Regional Anesthesia Absolute Contraindications • Patient refusal • Coagulopathy • Infection at needle insertion site • Severe hypovolemia with ongoing blood loss Relative Contraindications • Prior back surgery • Certain cardiac lesions, especially aortic stenosis • Increased intracranial pressure ANESTHESIA FOR CESAREAN DELIVERY The type of anesthesia for cesarean delivery is determined by: • Urgency of the surgery. • Presence or absence of a preexisting epidural catheter for labor. • Patient’s medical condition. • Pregnancy-related complications. • Presence of any contraindications to regional anesthesia. ANESTHESIA FOR CESAREAN DELIVERY • For cesarean delivery, regional anesthesia is preferred because the airway is maintained . • General anesthesia carries a 16-fold higher risk of anesthesia-related maternal mortality compared with regional anesthesia . • If no epidural is in place, a spinal block is frequently used. General anesthesia is employed for cesarean delivery in three situations: • Extreme urgency without a preexisting, functional epidural catheter • There is a contraindication to regional anesthesia • Regional anesthesia has failed. Parturients have a higher risk for airway complications than non pregnant patients: 1. An 8 times higher chance of failed intubation 2. 60% increased oxygen consumption 3. Decreased functional residual capacity (FRC) resulting in a lower oxygen store 4. Increased risk for aspiration. The protocol for general anesthesia for cesarean birth includes: 1. Oral administration of nonparticulate antacid (sodium citrate) 2. routine monitoring. 3. Left uterine displacement. 4. Preoxygenation for at least four vital capacity breaths. 5. Rapid sequence induction of anesthesia with cricoid pressure followed by intubation 6. Once the correct position of the endotracheal tube has been confirmed by end-tidal CO 2 and auscultation of the lungs, surgery may begin. THANK YOU