Lecture Week 1
advertisement

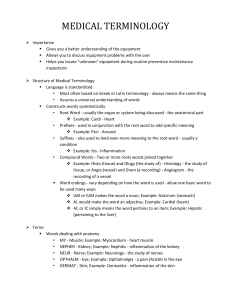
Learning Objectives: 1. Define pathology and scope of human pathology. 2. Describe the definition and classification of Inflammation. 3. Know the causes of inflammation 4. Understand the process of inflammations 5. Comprehend the etiopathogeneses of granulomatous inflammations 6. Contrast the differences between acute and chronic inflammations Definition: Pathology is defined as the structural and functional changes in the body caused by disease or trauma. Diseases are the deviations from normal. The Scope of Human Pathology • Pathology deals with recognition of diseases, their causes (aetiology), and their progression. • Pathologists study structural changes (gross, or microscopic), etiology and mechanisms of diseases (pathogenesis) • Most diseases can be placed in one of these categories: 1. Inflammatory 2. Neoplastic 3. Degenerative conditions 4. Developmental conditions Inflammation Inflammation: Local defense and protective response against cell injury or irritation or Local vascular and cellular reaction, against an irritant. Irritating or injurious agents (Irritant) Living: • Bacteria, • Fungi, • Virus, • Parasite • or their toxins Non-Living: • Chemical • Physical • Mechanical Inflammation is designated by adding the suffix (itis) to the end of the name of the inflamed organ or tissue. Types of inflammation 1) Acute inflammation 3) Chronic inflammation 2) Sub acute inflammation: rarely occur. 1. Acute inflammation Macroscopic signs: classical 5 cardinal symptoms (Celsus 1st c. B.C., Virchow 19th c. A.D.) 1. calor - heat 2. rubor - redness 3. tumor - swelling 4. dolor – pain & Tenderness 5. functio laesa - loss (or impairment) of function Microscopic signs: Inflammatory response 1. Local vascular change 2. Formation of inflammatory exudate Inflammatory response: (microscopic signs) First: Local vascular changes: 1. Initial temporary vasoconstriction for few seconds. 2. Active vasodilatation of arterioles and capillaries (by chemical mediators: Histamine) and passive dilatation of venules. Increase in capillary permeability (fluid exudate to the extravascular tissue) thus concentration of blood cells, slowing of blood flow (stasis) 3. Pavmentation: the margination of leukocytes. Normal Inflammation Second: Formation of inflammatory exudates: • Immigration or infiltration of the various leukocytes, fluid and plasma proteins outside the blood vessels into the surrounding tissue without injury of the blood vessels. • Leukocytes seem to leave the smallest blood vessels by inserting pseudopodia into the interendothelial junctions and sliding through the wall by amoeboid movement. • This is also due to the increased capillary permeability caused by the high osmotic pressure of the surroundings. • The early stages are marked by the predominance of polymorphs especially neutrophils migration, particularly when the inflammation is caused by pyogenic cocci, later on monocytes infiltration occurs. ****In some cases RBCs may also pass (Diapedesis) Function of inflammatory exudates 1-Dilute the invading microorganism and its toxins. 2-Bring antibodies through the plasma to the inflamed area. 3-Bring leukocytes that engulf the invading microorganisms. 4-Bring fibrinogen through the plasma, which is converted, to fibrin mesh, helping in trapping the microorganism and localize the infection. Blood stem cell Cells of inflammatory response 1) Polymorphonuclear leukocytes: are basophils, neutrophils and eosinophils; lobed nucleus and grainy cytoplasm (granulocyte). Microphages (small eaters) 2) Monocytes or histocytes: macrophages. (big eaters) 3) Lymphocytes: leukocyte of fundamental importance; they determine the specificity of the immune response to infectious microorganisms and other foreign substances. 4) Plasma cells: A type of immune cell that makes large amounts of a specific antibody, developed from activated B cells (Derived from lymphocytes originate in the bone marrow). It is a type of WBCs and also called plasmacyte. Neutrophil Lymphocyte Eosinophil Plasma cell Basophil Monocyte Name Neutrophil Eosinophil Basophil Monocyte Lymphocyte Microphage Acidophile Basophil Macrophage = >Polymorphs Histocytes and < RBCs Plasmacyte Shape Pale pink to blue, Minimal granulation. Red with eosin, Coarse granulation. Blue with eosin, Coarse granulation 1.5 to 2 times larger, Abundant fine granulation Agranular: non-granulated, Large round nucleus Basophilic, Encentric nucleus % of WBCs 60-70% 1-2% (50% in allergy) 1% 4-6% 30% Found in tissue only Functi on Phagositic 1st defense Unknown but could neutralize histamine, serotonin and other kinins Unknown but contain histamine &heparin Phagocytic 2nd defense element engulf bacteria, dead cells, debris & dead neutrophils (pus cells) Antibodies production Late stage of the inflammation Primary source of specific Antibodies Monocytes Plasma cell Plasma Plasmacell cell Phagocytosis • Process by which Phagocytic cell (microphages and macrophages) engulf and kill foreign particles (bacteria) Two main types of phagocytes: 1- Motile phagocytes found in the blood stream and migrate to the inflamed area (microphages) 2- Histocytes (macrophages) of the reticuloendothelial system (RES) which remove bacteria that escapes from the inflamed area. Normal cell Phagocytosis Phagocytosis Steps of Phagocytosis 1. Recognition 2. Ingestion- pseudopods engulf microbe through endocytosis 3. Vacuole Formation- vacuole contains microbe 4. Digestion- vacuole merges with enzymes to destroy microbes 5. Exocytosis- microbial debris is released It occurs in two subsequent stages 1. Ingestion of the m.o. 2. Intracellular killing of the m.o. (digestion): • Increased glycolysis and the PH drop to 4 -4.5 • As a result, the proteolytic enzymes, phagocytin, lysozyme and other hydrolytic enzymes (lipase, esterase, nuclease … etc.) are released and digest the ingested microorganism. Some species of bacteria e.g. tuberculosis are not killed within the phagocyte and even multiply within it. Methods of Intracellular killing of the m.o. (digestion) I. Oxygen-dependent intracellular killing: Production of a superoxide. Use of the enzyme myeloperoxidase from neutrophil granules II. Oxygen-independent intracellular: 1. electrically charged proteins 2. lysozymes 3. lactoferrins 4. proteases and hydrolytic enzymes Ingestion stage Chemotaxis • Positive directional response to chemical stimuli (chemotactic subs) • The migration of leukocytes (by amoeboid movement) toward the injurious agent and the injured cells due to chemical stimuli (chemotactic subs). Chemotactic subs: Exogenous (Specific): Polysaccharide secreted by m.o. Endogenous (General): Reaction product of the antigen-antibody reaction . Chemotaxis Types of acute inflammation (based on type of exudates) 1- Catarrhal inflammation: 2- Serous inflammation: 3- Fibrinous inflammation: 4- Membranous inflammation: 5- Hemorrhagic inflammation: 6- Gangrenous inflammation: 7- Allergic inflammation: 8- Suppurative or purulent inflammation: Name Occur in Characterized by Exudates rich in mucous Catarrhal Mild inflammation in mucous membrane of respiratory or alimentary tracts e.g. common cold and catarrhal appendicitis Serous Mild inflammation in serous surface such as pleural cavity, joint cavity where no damage in endothelium ex. Tuberculosis pleurisy and Common blisters Extensive watery low protein exudates Fibrinous Outpouring of exudates with high protein and less Exudates rich in fibrinogen volume ex. in lobar pneumonia due to Streptococcus pneumonia & pericardium inflammation Fibrinous inflammation in which network of fibrin entangling inflammatory cells and bacteria forms Membranous pseudo-membrane. Example: Diphtheria , Bacillary dysentery. Yellowish grey pseudo membrane rich in fibrin , polymorphs & necrotic tissues In blood vessels e.g. in plague Exudates rich RBCs Acute appendicitis Necrotic tissues resulting from thrombi or emboli Allergic Result to Ag – Ab reaction Hypersensitivity Presence of edema & increase in vascularity. Suppurative Caused by pyogenic bacteria and is characterized by pus formation Example: Abscess. Large amount of Pus & Purulent exudates produced Hemorrhagic Gangrenous Lobar Pneumonia due to Streptococcus pneumonia is associated with massive fibrinous exudates in the lung alveoli. 3. Fibrinous type: 4. Membranous type Pseudomembranous inflammation in diphtheria showing network of fibrin entangling inflammatory cells. Bacteria forming pseudo-membrane (left). 5. Suppurative or purulent Pyemic abscess in myocardium. Abscess containing necrotic cell debris, colonies of bacteria, and large number of neutrophils, many of them degenerate. Myocardium is on the right. Suppurative or purulent inflammation Pus: thick fluid containing viable and necrotic polymorph and necrotic tissue 1. Localized: ex. Abscess: Abscess is the localized collection of pus, commonly seen solid block of tissue - Example: dermis, liver, kidney, brain etc. Pus consists of partly or completely liquefied dead tissue mixed with dead or dying neutrophils and living or dead bacteria, formed of 3 zones 1. Small abscess is called boil or furuncle 2. Large one carbuncle 3. Fistula 2. Diffused: Spreading of pus to adjacent areas e.g. cellulites occurring in subcutaneous tissue . Usually caused by streptococci. Abscess: Fate of acute inflammation 1- Resolution: exudates are reabsorbed and tissue becomes normal again. 2- Healing: by repair and regeneration. 3- Spread: through lymphatics or blood stream. 4- Chronicity Chronic inflammation: (granulomatous) • Results from increased resistance of the causative agent to phagocytosis or the body defense mechanism is depressed. • Shows lower vascular and exudative response • The inflammatory cells are mainly macrophages, plasma cells, giant cells, lymphocytes, fibroblasts. • Occurs in the form of granuloma. • Chronic inflammation usually occur with granulomatous infections; e.g. leprosy, tuberculosis and fungal infections. Thanks