evaluation of cp
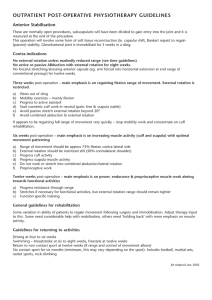
advertisement

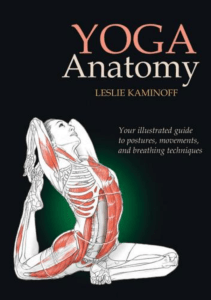
Nivedita.P.Kashyap Discover the functional abilities and strengths of the child Determine the primary and secondary impairements Discover the desired functional and participation outcomes of the child/family 1. - - Data collection Date of birth Date of assessment Chronological age Reason for referral Relevant medical history Overview of function Family and environmental characteristics Assistive technology /adaptive equipement - - Morphology Functional skills and capacity for change Gross motor control Communications Fine motor control Social skills/behaviour Observation of posture and movement Individual system review related to function Neuromuscular Musculoskeletal Sensory Respiration Cvs Perceptual /cognitive Areas of concern - System impairements - Ineffective posture and movement - Functional limitations - Barriers to participation Plan of care - Anticipated goals and expected outcomes - Frequency and duration of intervention - Stratergies of intervention - Role of family,medical team and educational professionals Team worker in assessment of C.P 1- pediatrition 2- neurologist therapist 4- Occupational Therapist 5- Social Worker 7- Dentist 8-speech therapist 3- physical 6- Nutritionist History is a key component in evaluating the child as it provides valuable information for diagnosis the timing of achievement of developmental milestones and the presence of associated impairments help to decide a functional prognosis. Family History: Consanguinity Medical history: Anti epileptic drugs, muscle relaxant Observing the child’s movements is the initial and most crucial part of the examination. The principal rule is “Observe before you touch”. If the child is young, apprehensive or tearful, let him or her stay on the mother’s lap while you watch and talk to the mother As the child adapts to the environment, slowly place him on the mat and watch him moving around. If the child cries a lot and does not cooperate, continue let him in mother’s lap.. - In addition to the gross observational assessment the therapist should examine individual aspects of motor function as part of overall evaluation of the child. The foll list of positions provides guidelines by which to assess functional antigravity control Supine Prone Side-lying Sitting-short sit,long sit,side sit, ring sit Quadruped Kneeling,half kneeling walking - - - When assessing postural control look out for the following Does the child have a variety of ways to transition between postures or only steriotypic choices? Does the child actively push into the supporting surface with the pelvis or extremities? Is the child able to repeat movements or tasks and make small changes in his or her motor performances? Tone is used to describe how a muscle or group of muscles feel when the joints of the body part are moved through a particular range. Slight resistance or amount of tension that you feel when move muscle. The child must be calm for assessment of muscle tone The head should be placed in the neutral position because turning or flexion can trigger tonic neck reflexes and interfere with muscle tone. “Spasticity” is the resistance felt while moving the joint through a passive range of motion. The “modified Ashworth or Tardieu scales” are utilized to grade spasticity. Methods of assessment: 1- passive movement 2- Shaking to distal part in all direction 3- Postural fixation(sudden release of limb) Factors affecting evaluation of muscle tone; 1-laughing 2- excitement 3- Surface 4light 5- Sleeping 6- head position Reflexes The persistence of primitive reflexes and the absence of advanced postural reactions should be evaluated. The presence of primitive reflexes beyond 6 months of age is a sign of poor prognosis. This examination reveals contractures and deformities that interfere with mobility. The examination is performed in a comfortable room with adequate space and props to attract the child’s attention Range of motion: ROM test must be done in a slow and smooth manner. Sudden stretch of the muscle increases spasticity, creating the false impression of a fixed joint contracture. Evaluation of spine Mobility of spine in all planes for correct alignment. Smooth symmetric movement of the spine. See for passive spinal flexion, spinal extension, lateral flexion and rotation Thoracic movement Examination of the respiratory excursion of the thorax is a critical portion of motor assessment for the child with cerebral palsy. Respiratory function should be assessed with the child in various functional positions Evaluation of shoulder girdle and upper extremity - Tightness and limitation of shoulder girdle - Tightness of pectoralis major - Dynamic scapular stability - Passive flexion,abduction and external rotation of shoulder - Extension of elbow, supination of forearm - Extension of wrist and fingers 1. 2. 3. Flex wrist Gradually extend Palpate contracted / spastic tendon ( FCU or FCR ) Foot propagation angle Femoral rotation int. / extr. Rotation Tibial rotation Foot – Thigh Angle - - An early immature normal gait is characterised by Uneven step length Excessive flexion of hip and knee during swing phase Immobility of pelvis without pelvic tilting or rotation Abduction and external rotation of hips throughout swing phase Base of support that is wider than the lateral dimensions of the trunk Pronation of foot Foot flat Hyperextension of knee throughout stance phase UE in high,medium,low guard position. - - - Spastic diplegic Limited mobility in lumbar spine,pelvis, and hip joints Limited asymmetrical pelvic tilt/rotation Hips stay flexed during stance and full extension of hip is never achieved Excessive adduction and internal rotation of hip In severe cases medial aspect of knee approximate. Feet may be in valgus outside the lateral dimensions of the trunk/close together in narrow base of support in PF with heels off of the floor. Speed of walking is reduced. - Hemiplegic gait Asymmetry is the most obvious feature Weight bearing is mostly on unaffected limb Shifting of weight on involved side is limited /incomplete Limbs on involved side are retracted or rotated posteriorly Arm swing occurs only on normal side Involved extremity is held in shoulder hyperextension and elbow flexion - - Athetoid cp Lower extremity is usually lifted high into flexion and placed down in stance into extension with adduction,internal rotation and plantar flexion. Hips stay slightly flexed,lumbar spine is hyperextended and thoracic spine is excessively rounded with capital hyperextension,flexion,and rotation of cervical spine with jaw forward and rotated to one side.