Neurohormonal Regulation of GI Functions
advertisement

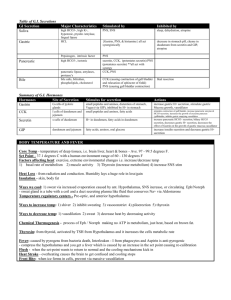
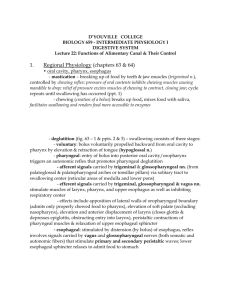
Lecture 5 Neurochemical Regulation of Gastro-Intestinal Functions Dr. Khaled Ibrahim By the end of the session the students should be able to: 1) Describe the physiological anatomy of the enteric nervous system. 2) Enumerate the Differences Between the myenteric and submucosal plexuses. 3) Discuss the autonomic (extrinsic) nervous control of the gastrointestinal activity. 4) List the gastrointestinal hormones classified in the gastrin and secretin hormones. 5) Discuss briefly the actions and regulation of gastrin, secretin and cholecystokinin. A. Text book of Medical Physiology by Guyton and Hall 12th edition, PAGE 755 –757. B. Ganong's review of Medical Physiology 24th edition, Page 468-471 The gastrointestinal system is arranged in the following sequence: Regulation of Gastrointestinal Functions Done by 1. Nervous regulation. 2. Hormonal regulation 1. Nervous Regulation. Carried out through the Autonomic N.S which has: a. Extrinsic component (symp and parasymp innervation of GIT). b. Intrinsic component (called the enteric nervous system (ENS) a) Intrinsic component (Enteric Nervous System) (ENS) Site: lies in the wall of the whole length of the gut. Components: myenteric plexus ( ) ms layers which controls motility. submucosal plexus in submucosa which controls secretory & endocrinal function. Number of neurons: equals to that of spinal cord neurons (i.e. important regulator of GIT) Function: can modulate all GIT function i.e. controls the contractile, secretory & endocrinal function of GIT. It can function independent on CNS. Connection: The ganglia of the ENS: A) Receives afferent impulse from: Symp. and parasymp. fibers. Sensory information from Mechano and chemoreceptors of the gut mucosa. B) Send motor fiber to smooth ms, secretory and endocrine cells. C) Ganglia of 2 plexuses are interconnected by interneurons. b) Extrinsic Innervation 1- Parasympathetic: 2 divisions Cranial Division Origin Sacral Division *Few fibers through VII and IX 2nd, 3rd and 4th sacral segments of spinal cord *Main supply through the vagus (X) (pelvic n.; nerve of defecation) *VII and IX: salivary glands mainly iin the mouth & pharynx. Supply *Vagus: duodenum, esophagus, stomach, Distal half of the colon. S.I & proximal half of large intestine (L.I). Preganglionic synapses with ganglia of ENS. Postganglionic supply sm ms, secretory & endocrine cells. Connection postganglionic are classified into: Cholinergic neuron -----> release acetyl choline. Peptidergic neuron ----> release substance P or vasoactive intestinal peptide (VIP) Function Stimulates all functions of the gut (i.e. motor, secretory….etc). 2- Sympathetic: Origin: from T5-L2 segments of sp. cord. Relay: in celiac and mesenteric ganglia. Connection: - The short preganglionic fibers enter the sympathetic chain. - Many of postganglionic fibers end on postganglionic parasympathetic cholinergic neurons where noradrenaline (NA) released from postgang. symp, inhibits a. choline secretion from postgang. cholinergic n. - Other sympathetic fibers ends directly on the target cells. Preganglionic sympathetic Preganglionic parasympathetic postganglionic sympathetic postganglionic parasympathetic - Function: Stimulation of sympathetic: a) Inhibit all functions of the gut. b) Produce VC of bl. vs - Reflexes Controlling GI functions 1. Short reflexes 2. Long reflexes * Responsible for local * Responsible for higher (integrated) control regulation of GIT i.e. (i.e. control many parts of GIT at same time) control local part of GIT. *Mediated by: ENS i.e. * Mediated by: ANS: All components of the They have centers in CNS. reflexes are located in They regulate GI functions in response to:GIT wall. 1.Impulses from outside gut (visual, olfactory, auditory …..etc 2.Local factors in the gut. 3.Other factors as pain and emotion. II. Hormonal Regulation GIT also has its own endocrine system. Carried out by group of special cells called APUD cells (Amine Precursor Uptake and Decarboxylation) that are located in GIT mucosa. These cells secrete gastrointestinal hormones (GIHs). After secretion, GIHs are absorbed ------> portal circulation ------> liver ------> IVC heart and then back again to digestive system to exert their actions. GIHs secretion is regulated by: 1. Nervous factors: either through: 2. Chemical factors: such as: - E.N.S. - A.N.S. - Blood-borne substances. - Luminal factors i.e. from lumen of the gut e.g. products of digestion, PH.... ------> GIHs are of 2 main families Gastrin family Includes: Secretin family Includes: gastrin hormone Secretin hormone. cholecystokinin h (CCK). vasoactive intestinal polypeptide (VIP). gastric inhibitory polypeptide (GIP). Gastrin Hormone Chemistry: Polypeptide present in several forms: G14 , G17, and G34. All forms have same c-terminal 5 chain a. a which is: The active part of the molecule. Pentagastrin is a synthetic form of the hormone & is formed only of the active part. Metabolism: inactivated in kidneys and small intestine Sources: G cells: in antrum mucosa and duodenal bulb. TG cells: throughout stomach and small intestine. Gastrin is also present in pituitary gland, hypothalamus and M.O Actions (Physiological Function) Of Gastrin: gastrin stimulates: 1- Secretion of HCl and pepsin from gastric glands. There is -ve feedback relation ( ) degree of acidity & gastrin secretion. “i.e. excess acid will inhibit gastrin secretion and vice versa". This represents protective mechanism against harmful effect of strong acid on gastric mucosa. 2- Motility of the stomach. 3- Growth of the mucosa of the stomach, small and large intestines. Control of gastrin Secretion: Stimulator Inhibitor Vagal stimulation but the ch. transmitter is not acetyl choline (i.e. couldn’t be blocked by 1. Nervous Factors atropine), it is a gastrin releasing polypeptide ------- (GRP) similar to "bombesin". 2. Luminal Factors 1. Distention of the stomach by food. acidity ( PH) of gastric contents 2. acidity ( PH) of gastric contents. (-ve feedback mechanism) 3. amino acids in gastric contents. 3. Bl-borne Factors .-------- Secretin, GIP & Somatostatin Cholecystokinin (CCK) In the past, 2 types of hormones were believed: One ++ contractility of gallbladder -----> so called "CCK". The other ++ exocrine secretion of pancreas rich in enzymes -----> so called “pancreozymine”. Now, It is known that a single hormone secreted by mucosa of upper S.I and has both activities -----> so called Cholecystokinin- Pancreazymin (CCK-PZ) or commonly CCK Chemistry: CCK is present in several forms CCK8, CCK12, CCK33, CCK39 & CCK58. All forms have same c-terminal 5 chain a. a. as gastrin. Source: It is secreted from I cells in upper S.I (duodenum & jejunum), plus the distal ileum and colon. It is also found in CC & may be involved in regulation of food intake, anxiety and analgesia. Action (physiological function) of CCK: CCK stimulates: Contraction of gallbladder & relaxation of sphincter of Oddi. Exocrine secretion of the pancreas rich in enzymes. It augments action of secretin h. on HCO3 secretion. Trophic effect on gall bladder and pancreas. Inhibits gastric emptying ----> help fat digestion and absorption as it needs more time. Control of Secretion: CCK is stimulated by:- Fatty acids in the duodenum. Products of protein digestion in the duodenum. There is +ve feedback ( ) CCK secretion and its i.e. conc. of F.A and products of protein digestion -----> ++ secretion of CCK and vice versa. stimulus Secretin Hormone Chemistry: It is a polypeptide contains 27 a. a. The whole molecule is needed for activity. Source: From S cells in mucosal glands of upper S.I. These cells are stimulated by: - Products of protein digestion. - Acidity of the fluid passing from stomach to the upper S.I There is +ve feed back ( ) secretin secretion and degree of acidity i.e. acidity secretin h. ------> release of Action of secretin: It stimulates pancreatic exocrine secretion w is large in volume, watery and rich in bicarbonate. This bicarbonate causes: 1) Neutralization of acidity -------> inhibits secretin secretion 2) Provides alkaline medium needed for action of pancreatic enzymes. The action of secretin on pancreas is mediated via cAMP. Nicotine (in cigarette) inhibits secretin secretion. SO, In heavy smokers, there is hyperacidity which may -----> peptic ulcer. Glucose –dependent insulinotropic peptide Or Gastric Inhibitory Polypeptide (GIP) Chemistry Source Stimulus for secretion Polypeptide (43 a. a.) Polypeptide K cells in mucosa of duodenum & jejunum. Found in: GIT, brain, autonomic nerves and blood. Glucose , fatty acids and amino acids presence of fats in the jejunum 1.Inhibits gastric acid secretion. Action Vasoactive Intestinal Polypeptide (VIP) 2.Stimulates insulin secretion (some types of DM is due to hyposecretion of GIP). many 1.Inhibits gastric acid secretion & motility. 2.Stimulates secretion of water & electrolytes form intestine