nervous regulation
advertisement

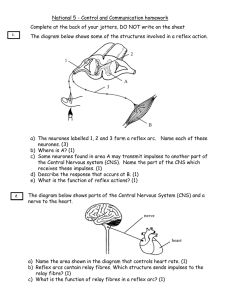
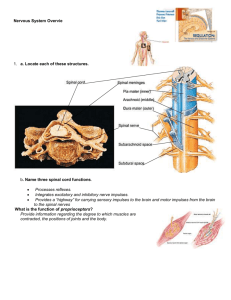
Lecture 44 Nervous Regulation of Circulation By Dr. Khaled Ibrahim Khalil By the end of this session, the student should be able to: o Describe the physiological anatomy of autonomic supply to the heart and blood vessels. o Discuss the nervous control of circulatory functions especially heart rate. o Describe the role of vasomotor center in regulation of circulatory functions. o Describe the various factors affecting activity of vasomotor center. Guyton & Hall Textbook of Physiology - 12th ed. P. 201204. Sympathetic Parasympathetic Anatomy Origin: CAC & VCC in medulla CIC in the medulla oblongata oblongata Relay: Parts supplied: In the upper 3 cervical In terminal ganglia In the ganglia heart. The whole heart All the heart except the ventricles Autonomic Receptor Cardiac muscle β1 adrenergic receptors Muscarinic (M2) receptors Coronary vessels β2 & α1 adrenergic receptors Muscarinic (M3) receptors Functions Rhythmicity: ↑H.R. ↓H.R. a) of atria ↑(may initiate extrasystoles) ↓(may stop an attack of P.T) b) of ventricles ↑(may initiate extrasystoles) no effect Excitability: Conductivity: ↑due to ↓A-V nodal delay ----> ↓P-R interval in ECG. ↓due to ↑A-V nodal delay. So, it may produce various degrees of heart block. Contractility a) of atria Increased Decreased b) of ventricles Increased No effect Metabolism Increased Decreased O2 consumption increased Decreased Coronary blood flow increased (see later) Decreased (see later) Nervous Regulation of HR The cardiac centers (CIC & CAC) controlling the heart rate are influenced by impulses from other nerve centers in the brain and by afferent impulses from the body. A- Impulses from higher centers: 1- The cerebral cortex: It is the highest center affecting HR directly or indirectly through the hypothalamus (as in emotions) in the following conditions: a- Conditioned reflex: - It is the change in HR in the response to visual, smell, hearing stimuli or even thinking about something. - HR may ↑ or ↓ according to the nature of the stimulus. - These stimuli stimulate certain areas in the frontal lobe of the cerebral cortex. - Conditioned reflex is not a true reflex, e.g. if a source of light is shown to a dog and then the dog's skin is pricked, the painful stimulus leads to marked ↑ in HR. With repetition of the experiment application of light alone without painful stimulus ----> marked ↑ HR. b- Voluntarily: Some people can ↑ or ↓ HR voluntarily as in practitioner of yoga. c- Emotions: - Most emotions (mild) e.g. fear, anger, sexual excitation…etc -----> ↑ HR. - Sudden shocking news (sever) ------> ↓ HR. 2- The hypothalamus: The hypothalamus is the higher center of the autonomic nervous system. a- Stimulation of anterior hypothalamic nuclei, which control parasympathetic activities -----> ↓ HR due to stimulation of CIC. (as in quite sleep). b- Stimulation of posterior hypothalamic nuclei, which control sympathetic activities -----> ↑ HR due to stimulation of CAC. (as just before starting a race or examination). B- Afferent impulses affecting the medullary cardiac centers: 1- Afferent impulses from the circulatory system: It is the most important impulses that regulate HR as it represents (-ve feedback mechanism) by which several circulatory functions are regulated as arterial blood pressure & circulatory volume. Impulses from the right side of the heart Impulses from the left side of the heart Bainbridge reflex Marey's law Bainbridge reflex: -Increased cardiac filling i.e. right atrial pressure, leads to reflex acceleration of the heart. Stimulus: ↑ right atrial pressure (RAP) as in ↑ed venous return or infusion of blood or saline. Receptors: atrial baroreceptorsThey are volume mechanoreceptors present in the wall of right atrium at its junction with superior vena cava & inferior vena cava. Afferent: vagal fibers. Center: - - CIC & ++ CAC. Efferent: Sympathetic fibers. Response: ++ SAN -----> ↑ HR. Significance: ↑ HR ------> ↑ COP This helps pumping of excess venous return to the arterial side and prevents stagnation of blood in veins i.e. (diastasis). Marey's law - The heart rate is inversely proportional to the arterial blood pressure provided that other factors that affect the heart rate remain constant. i.e., ↑ ABP -----> ↓ HR & vice versa Stimulus: ↑ arterial blood pressure (ABP). Receptors: arterial baroreceptors.In the wall of carotid sinus & aortic arch. Afferent: sinus nerve (branch of IX) & aortic nerve (branch of X). They are called "depressor nerves" because they resist rise in ABP. Center: + + CIC & - - CAC. Efferent: vagus nerve. Response: - - SAN -----> ↓ HR. Significance:↓ ed HR antagonizes the elevation of ABP & helps to restore it to its normal level. Carotid sinus syndrome Definition: This is a pathological condition in which the carotid sinus is abnormally hypersensitive. Manifestations: In patients with this syndrome, a slight pressure on the carotid sinus (e.g. during shaving or by tight collar) stimulates the baroreceptors in the carotid sinus ----> reflex ↑ vagal tone to the heart & ↓ sympathetic vasoconstrictor tone to the blood vessels -----> bradycardia (↓ HR) and hypotension (↓ ABP) ------> cerebral ischemia and momentarily loss of consciousness (fainting). Treatment: Denervation of the hypersensitive carotid sinus cure the condition. Clinical significance: Carotid sinus reflex could be used to terminate an attack of paroxysmal atrial tachycardia but not of ventricular origin, as the vagus does not supply the ventricles. 2- Afferent impulses form the body other than the circulatory system: Stimulation of the central end of any nerve containing afferent fibers e.g. radial, sciatic or splanchnic may produce ↑ or ↓ HR according to the nature of the stimulus. a- Impulses from skeletal muscles (Alams Smirk reflex): Contraction of voluntary muscles produces reflex increase in heart rate. - This occurs even with moving one finger. - Mechanism: Muscle contraction -----> + + proprioceptors in the muscle and joints ----> afferent somatic sensory nerves -----> + + CAC & - - CIC ----> ↑ HR. - Significance: help to ↑ blood supply to the active muscle. - It is a reflex, so, it is obtained after obstruction of the blood supply, and this proves that it is not due to the metabolites of muscular contraction acting on the cardiac centers or directly on the SAN. b- Impulses from pain receptors: - Mild pain sensation (cutaneous) -----> reflex tachycardia, due to ++ CAC & - CIC. - However, sever pain (visceral) -----> reflex bradycardia. c- Trigger zone reflexes: The carotid sinus, the eye ball, the larynx, the epigastrium and testes are sensitive areas known as trigger zones. A blow on any of these areas can produce reflex severe bradycardia, fainting or even cardiac arrest. THE VASOMOTOR CENTER (VMC) Vasomotor center is formed of: 1- Vasoconstrictor center. 2- Vasodilator center. The vasoconstrictor center (VCC): - located bilaterally in the antrolateral portion of the upper medulla. - It is also called vasopressor area. - Course: Neurons of VCC project descending axons -----> LHCs of all thorathic & upper 3 lumbar (spinal or subsidiary VCC) -----> preganglionic to relay in sympathetic chain or collateral ganglia -----> postganglionic noradrenergic fibers in spinal nerves -----> SMF of blood vessels -----> VC of blood vessels. Mechanism of activity of the VMC: Under normal resting conditions the VMC is exposed to: Pressor effect of normal CO2 tension in the blood causing stimulation of the VMC. Depressor effect of arterial baroreceptors in the aortic arch and carotid sinus by the normal level of ABP causing inhibition of the VMC. Normally, the stimulatory effect of CO2 predominates, leading to continuous discharge from the VCC, producing the VC tone. Vasomotor Tone: Definition: Continuous partial V.C. of arteries & arterioles at rest. Mechanism: Contineous partial activity of VCC (see before). Significance: maintain peripheral resistance & Diastolic ABP. Spinal subsidiary vasomotor centers: - The bilateral horn cells of the thoracolumbar region of the spinal cord - When they are separated from the VCC, they stop transmission of the VC impulses leading to VD and marked drop of arterial blood pressure. b. The vasodilator center (VDC): - It is located bilaterally in the antrolateral portion of the lower half of the medulla. - The fibers from these neurons project upward to the vasoconstrictor center - When it is stimulated it inhibits the vasoconstrictor activity of the VCC, thus causing vasodilatation. - There is no direct connection between the VDC and the vasodilator nerves. Factors affecting the vasomotor center These factors can be classified into nervous and chemical factors I. Nervous factors: 1. Impulses from the higher centers: a. The cerebral cortex: - can either stimulate or inhibit the VMC depending on the site, and the intensity of the stimulus. b. The hypothalamus: - Stimulation of the postrolateral portions of the hypothalamus -----> excitation ------> V.C. & ↑ABP. -Stimulation of the anterior part ------> inhibition --------> VD & ABP. 2. Afferent impulses from the circulatory system: a. From the arterial baroreceptors: Stimulation aortic of the arch carotid and sinus receptors increased by level of ABP, send depressor impulses vasomotor to the center, producing VD and drop at ABP. b. From the chemoreceptors: Stimulated by O2 lack, CO2 excess or increased H+ concentration in the blood. When stimulated they send pressor impulses to the VMC, causing vasoconstriction with consequent rise of ABP. c. From the atrial baroreceptors: A fall of the right atrial pressure e.g. during hemorrhage, sends pressor impulses to the VMC. Stimulation of the VMC leads to arteriolar constriction, which result in elevation of ABP towards normal level. 3. Afferent impulses from other parts of the body: 1) Cutaneous pain: mild ------> ++ VMC , sever ------> -- VMC 2) Sever visceral pain or afferent fibers from the trigger zones -VMC. 3) Afferent impulses from the Propiroceptors of skeletal muscles during exercise ++ VMC. 4) Loven's reflex: Stimulation of the afferent nerve of an organ produces local vasodilatation in the active organ but generalized vasoconstriction due to stimulation of the VMC. 5) Cold pressor test: If a normal person drips his hand in a cold water (4oC), ABP rises by 10-20 mmHg, due to stimulation of the VMC