oxygen transport
advertisement

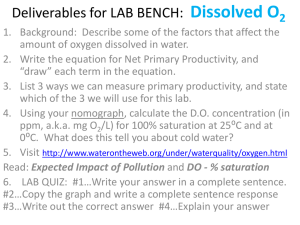
LECTURE 20 Oxygen Transport by Blood By Dr. Khaled Khalil Assistant Professor of Human Physiology At the end of this session, the student should be able to: Describe the forms in which oxygen is transported in the blood. Define oxygen partial pressure (tension), oxygen content, oxygen capacity and percent hemoglobin saturation. Illustrate and describe oxyhemoglobin dissociation curve. Describe factors affecting shape of oxyhemoglobin dissociation curve (shift to right and shift to left). Describe the diffusion of oxygen from capillary blood to tissues and different factors affecting it. GUYTON & HALL Textbook of Medical Physiology, 12th edition, page: 495-502. O2 is present in the blood in two forms: I. Physical solution: 1- Each 100 ml of arterial blood contains 0.3 ml of O2 dissolved physically in plasma. 2- Each 100 ml of venous blood contains 0.13 ml of O2 dissolved physically in plasma. II. Chemical combination: More than 98% of the O2 is bound to hemoglobin of the red blood cells. I. Physical solution: Although it is small amount but it has the following significance: It determines the rate and direction of oxygen flow. As O2 diffuses from high pressure to low pressure, physically dissolved O2 acts as a pathway for the supply of O2 to and from hemoglobin. When the blood reaches the tissues, it is this small amount that is first transported to the cells and then, it is replaced rapidly by more oxygen liberated from Hb. Hemoglobin - It is an oxygen carrying pigment. 2) Heme 1) Globin - a protein composed of four -Four pigment polypeptide chains. containing a single ferrous ion in - There are many types of the center of each molecule. polypeptide chains according Each ferrous ion can combine to their amino acid sequence. with e.g., -chain, β-chain, γ-chain, Therefore, One Hb molecule can and δ-chain. combine with 4 molecules of O2. one molecule molecules of O2. - According to the type of polypeptide chains forming the globin portion, Hb can be classified into: Hb A (formed of 2 + 2 β chains): it represent 98% of Hb in adults. Hb A2 (formed of 2 + 2 δ chains): it represents 2% of Hb in adults. Hb F (formed of 2 + 2 γ chains): it represents the main Hb in fetus. Binding of Oxygen to Hb is characterized by: The reaction is reversible and rapid. The reaction is oxygenation not oxidation. i.e., the iron in the heme remains in the reduced form “Fe++ or ferrous iron”. The combination of Hb and O2 occurs in steps and each step accelerates the next one. i.e. Hb + O2 HbO2 (25 % saturation) HbO2 + O2 HbO4 (50 % saturation) HbO4 + O2 HBO6 (75 % saturation) HbO6 + O2 HBO8 (100 % saturation) Oxygen content of the blood: -It is amount of O2 present in chemical combination with Hb in 100 ml of blood. Oxygen capacity of the blood: - It is the amount of oxygen present in chemical combination with Hb in 100 ml of blood when it is fully saturated. - In normal subjects, Hb content is about 15 gm % and each gram of Hb can combine with 1.33 ml O2. - O2 capacity = 15 x 1.33 = 19.95 ml (about 20 ml O2 / 100 ml.) - Oxygen capacity depends upon Hb content. So, It is decreased in anaemia. Percentage (%) saturation of hemoglobin with oxygen: - This equals = O2 content / O2 capacity x 100 - Under normal condition, the Hb of systemic arterial blood is only 97% saturated with O2 (not fully saturated). - This is due to addition of venous blood from bronchial and coronary veins to the arterial blood which is called physiological shunt. Coefficient of O2 utilization: - Definition: It is the % of the blood that gives its oxygen as its passes through the tissue capillaries. It equals = O2 content in arterial blood – O2 content in venous blood O2 content in arterial blood - The total quantity of oxygen bound with Hb in normal arterial blood is approximately 19.5 ml/100 ml blood. On passing through tissue capillaries, this amount is reduced to about 14.5 ml /100 ml blood. Thus, during rest about 5 ml of O2 is utilized by the tissues by each 100 ml of blood. The normal value for utilization coefficient is approximately 25%. -In muscular exercise, It is increased to 75%. O2 Dissociation Curve It is the curve which study the factors that affect the % saturation of Hb with O2 in relation to O2 tension of the blood. How to obtain the curve? - Blood samples are placed in special vessels known as tonometer used for blood equilibration with gases at body temperature, and each is exposed to a certain O2 tension. - The O2 content in each tonometer is determined. - O2 content is divided by the O2 capacity to get the % saturation. - % saturation is plotted against the O2 tension. Shape of the curve: - The oxygen dissociation curve has a Characteristic sigmoid or S shape. - This is because the combination of O2 with the haem groups of the Hb occurs in steps as the affinity of haem to O2 is increased after the haem group is oxygenated. Physiological significance of the curve: The curve has 3 parts: 1) Upper flat part (plateau). 2) Middle curved part (slope). 3) Lower vertical part (steep). 1) The At upper flat mmHg.), % Hb saturation 60 mmHg., causes decrease of % Hb part is 100%. (note that inside saturation from 100% to 90% (i.e., only (plateau): the body, % saturation 10%). O2 tension (100 So, decrease O2 tension from 100 to will be 97% only due the The functional significance of the flat physiological shunt). At O2 tension part of the curve is that the arterial O2 (80 saturation does not change much until mmHg), % Hb saturation PO2 has decreased to about 60 mmHg. is 93 %. At O2 This enables persons living at high tension (60 altitudes or with lung disease to get mmHg), % Hb saturation enough O2 from this blood. is 90%. 2) This Middle that: At O2 tension (40 mmHg, causes decrease of % Hb saturation curved mm Hg), the % Hb from 100% to 70% (i.e., 30% decrease of % part saturation is 70%. (slope): part shows So, decrease O2 tension from 100 to 40 O2 saturation which are given to the tissues during rest). This satisfies the tissues needs during rest & maintains an oxygen reserve in the blood for emergency condition. Lower This part shows that: This enables peripheral tissues to vertical part With further decrease of withdraw large amount of oxygen for (steep): O2 tension (below 40 only a small drop in capillary PO2 as mmHg), there is marked occurring in muscular exercise. decrease in the % Hb saturation (i.e., more O2 supply to the tissues). Factors affecting O2 dissociation curve: A number of factors can influence the affinity of HB to oxygen. These factors may cause shift of the curve either to right or to left. Shift to right: Hb gives more O2 to tissues even under high O2 tension. Shift to left: Hb gives less O2 to the tissue even under low O2 tension. Factors that shift the curve to Factors that shift the curve to right: left: 1) Increased H+ concentration. 1) Decreased H+ concentration. 2) Increased Partial pressure of 2) Decreased partial pressure of CO2. CO2. 3) Increased temperature. 3) Decreased temperature. 4) Increased 2,3 DPG Function. 4) Decreased 2,3 DPG function. 5) Carbon monoxide poisoning. 2,3diphosphoglycerate (2,3 DPG) It is a chemical substance produced by the mature RBCs to increase the release of O2 from Hb. Formation: Mature RBCs lack mitochondria. Therefore, they obtain energy through the anaerobic glycolysis. During the course of glycolysis, 1,3 DPG is formed where it can be converted to 2,3 DPG by a side reaction using 1,3 DPG mutase enzyme. Function: 2,3 DPG combine with β-chain of Hb causing release of O2 to the tissue. 2,3 DPG is increased in : 2,3 DPG is decreased in: 1) All conditions of hypoxia 1) Fetal hemoglobin. as in: High altitudes. 2) Muscular exercise. 3) Certain hormones such as: testosterone. 2) Stored blood.