Document 15349747
advertisement

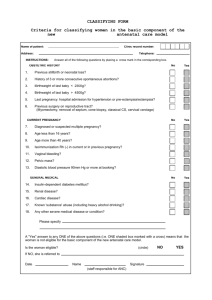
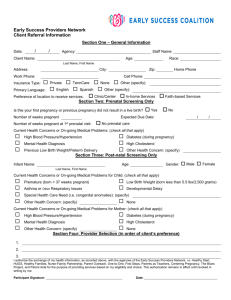
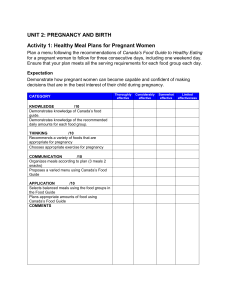
Out lines Objectives of lecture. Introduction about antenatal care. Related definitions MH, MM, IH, IM. Causes of maternal & infant mortality. Methods of reduction of maternal & infant mortality. Definition of antenatal care. Importance &purposes of antenatal care. Factors affecting the ante partum experience. Barriers to qualify of antenatal care. Quality\improvement. Definition of quality of care. Component of quality of prenatal care. Structure: 1. Building 2. Personal. 3. Facilities. 4. Records. Process: 1. General. 2. Specific. Out comes: 1. Results of quality improvement. Component of antenatal care: Initial visit. Subsequent visits. Health education according to level of prevention (Primary, secondary, tertiary). Items of health education: Follow up. Minor discomfort. Immunization. Danger signs. Coitus. Clothes. Traveling. Hygiene. Breast examination & care. Diet Hazards. Preparation for labor. 2 Objectives General Objectives: At the end of this lecture the post graduate student should be able to upgrade a comprehensive knowledge about high quality of antenatal care. Specific Objectives: 1. Define related definition. 2. Discuss causes of maternal & infant mortality. 3. Explain methods for reduction of maternal & infant mortality. 4. Define concept of antenatal care. 5. Identify purposes of antenatal care. 6. Determine barriers to quality of antenatal 7. Discuss component of quality of prenatal care. 8. Apply health education according to levels of prevention. 3 Antenatal Care Introduction: Antenatal cafe is not just physicians for examination & nurses for providing the care but there are other persons have a role in affecting quality reproductive health services which are essential for the reduction of maternal mortality as policy makers, health professionals, social workers, religious leaders There are related definitions we must know: Maternal health: Encompasses the health, of women in the child bearing years including those in pregnancy period those who are pregnant & those who are caring for young children. Maternal mortality rate: Is defining as number of mothers dying per 100,000 live birth in given year. There are two types of MM: Pregnancy associated maternal death. The death of any woman from any cause while she is pregnant or with one calendar year of termination of pregnancy. Pregnancy related maternal death: The death of any woman resulting from complication of the pregnancy itself as "Hypertension disorder of pregnancy, abortion, ante partum& postpartum hemorrhage, amniotic fluid embolism & puerperal sepsis". MM has decreased there are almost 100,000 more maternal deaths annually, now compared to 10 years ago 585,000 must present a challenge to every citizen in society. Infant mortality rate: Is expressed as the number of deaths of children under one year of age per 1.000 live births. There are two types of IM: Neonatal death. The death occurs during first 28 days after birth which are most often attributed to prenatal events& event occurring just afterbirth. Post neonatal death: The death occurs between 28day & 365 day after birth which are dependent on infant's environment including skills, the availability & use of pediatric services. Methods for reduction of MM: 4 Early recognition, improvement & treatment of preeclampsia with preventive care & efficient management of eclampsia. Prophylactic use of cytometrine treatment of "ante - intra – post" partum hemorrhage. Reducing sepsis by primary infection control measures such as following aseptic techniques during all procedures& secondary by introduction of antibiotics. Improved anathesiatic techniques. Advances in knowledge of blood coagulation disorder & its management. Improved standard in maternity services (programmers – prenatal care). High light & screening women at risk & providing intensive care when needed & early detection of high risk cases. Improve social conditions as "nutrition – family planning". Methods for reduction of MM: Improve socio economic status. Improve housing. Improve nutrition. Improve levels of immunization. Improve antenatal& postnatal care. Improve quality of her delivery &the infant environment after birth. Definition of antenatal care: Adequate prenatal care is a comprehensive process in which problems associated with pregnancy is identified & treated additionally (education & support are provided). OR: It is planned examination, observations guidance that includes medical activities & education given to the pregnant women from conception till the time of labor. Importance &purposes of antenatal care: Women are important member in family so the protecting she lives of mother & her out comes during pregnancy is very important to decrease mortality & morbidity rate to obtain good health community. Purposes: Maintenance of maternal fetal health. Recognition of abnormalities & complication at an early stage. Prevention of health hazards to which mother may expose. Woman family education about pregnancy, birth & parenting. To build trust between the family & care providers. Referral to appropriate resources as (threatened abortion, accidental hemorrhage). Factors affecting the ante partum experience: Previous experience with pregnancy. 5 Cultural & personal expectations. Pregnant health & biophysical preparedness for child bearing. Motivation for child bearing. Socioeconomic status. Mother’s age. Accessibility of prenatal care. Level of education. Barriers to quality of antenatal care: Personal barriers: Inadequate finances. Lack of transportation. ; Tendency not to value prenatal care or understand its importance. Failure to realize one is pregnant. Ambivalence or fear of pregnancy. Dislike or fear of the health care provider. System barriers: Negative institutional practices. Limited availability of providers. Lack of child care. Major factors which interfere with participation in prenatal care: Demographic: Age <20, >40. Educational level. Marital status single Financial: Unemployed. Poverty. Inadequate or no health insurance. Health care system: Limit capacity. Cultural insensitivity. Unwelcoming clinic atmosphere. Inconveniencing hours open & limit choice for appointment. Client: Personal cultural views with regard to health care during pregnancy. Knowledge deficit regarding pregnancy, importance of prenatal care& where to go for care. Concurrent stressful life experiences. Fear embarrassment. 6 Attitude toward pregnancy. Quality improvement: Definition of quality of care: It is the optimum level of health care provides for the pregnant woman from the first missed period until delivery. OR: Provide comprehensive components of health care based on the community facilities to reach the optimal health services. Components of high quality health care: Many international agencies & governments are promoting & developing quality assurance in developing countries to improve health care & save the health & welfare of people. Quality assurance: Are the standards which can be formulated for both clinical & no clinical process at the all levels of health care system. Standards may be directed toward structure standards address environment, human, financial & physical resources. Process Standards apply to services provision interaction & collaboration, training management. Outcome standards apply to result again both clinical & non clinical from structure & process improvement. Structure of health care: Physical Setting & building: Should be situated at the center of the community & there is a suitable transportation. Include the main room as delivery room, environment room, laboratory pharmacy, teaching classes & administrative office also W.C. The design should be wide has a good ventilation, electricity, and water. Personal: The personal staff should compose of health team members & administrative members. The health team composed of doctors (obstetrician & gynecologist) pediatrics, dentist& pharmacologist. Nurses high qualified nurse, midwife & diploma nurse. Technician (laboratory & X-ray technician). Sociologist& psychologist. 7 The number of personnel should be suitable for the number of the client & services provided. Every employee should attend for regular training programs & support with continues evaluation for progress of perform not for punishment. Training for emergency situation. Training practically on new machines & apparatus. Facilities & supplies: The health center should have ambulance care for emergency & available transportation. Adequate medical equipment, instrument & supplies. This should be a new technology, up dated & sterile. Fixed budget enough to cover all need. Records: Recording sheet of all clients. Physical examination sheet. Laboratory records. Follow up records. Immunization records. Pharmacacy records. Records for special cases as HT, BP chart/or cases of Preeclampsia, insulin chart for diabetic mother, reports of E.G.G for cardiac mother, amniocentesis chart for cases of polyhydraminos. Process of health care: General process: To provide a high quality antenatal care it is preferable to begin at premarital or preconception period. To detect, correct any health hazards as early as possible. To bring the woman to pregnancy in the best possible health. To attend to preventable factors before pregnancy start for example rubella in occultation. To discuss antenatal diagnosis & management of abnormality. To give advice about the effect of: Preexisting disease on pregnancy & unborn child. The pregnancy on preexisting disease & its progress. To consider the effect of recurrence of events from previous pregnancies. First services at the first antenatal visit: The aim of this visit: To screen & asses the maternal & fetal health condition. To identify the high risk group. To plan the follow up. We can do all of this by using the following elements: 8 History: Demographic history (name, age, address ...). Past history (medical, surgical, obstetric, menstrual), Present history (L.M. P, present complain & need). Comprehensive family history (medical, surgical, obstetric, psychological ...). Psychological & social assessment. Nutritional assessment. Psychological assessment: 1. Self concept: Perception of physical self: Description of current health. Feeling expressed about changing body image & sensation. Measures taken to enhance health during pregnancy this include views about health guidance during pregnancy. Perception of personal self: Reaction to & feelings about pregnancy. Perception of pregnancy & parenting realistic, un realistic. Coping mechanisms used to cope with the demands of pregnancy & parenting effective or ineffective. Culture beliefs regarding pregnancy parenting. Progress in meeting the developmental tasks. Moral, ethical, spiritual, values, beliefs & stander of behavior. Level of knowledge concerning pregnancy: Adaptation. Self assessment & self care measures. Father considers self concept& perceptions meeting of development of tasks, coping mechanisms. 2. Role function: Description of: Current roles. Role responsibility& expectation we define by (self, family, and support system). Role performance as determined by self, family, support system. Present of role conflicts. Potential for role conflicts with the addition of pregnant women role & then the parent role. Awareness of high risk for role conflicts & preparation made. Perception regarding the role of mother. Present knowledge & skills regarding the mother role &measure taken to prepare for the mother role. Interdependence: Family support system: 9 Who are they? Capability of given support? Degree of support offered during pregnancy & after the baby is born? Relationship of expectant mother & father with each other & family & support system. Willing to accept support. Strength to appropriately refuse or limit support. Responses of family & support system to pregnancy, parent, siblings, grand parents, friends & coworkers. Sibling preparation measures. Stability - safety of the home work environment. Financial security. Community agency support required accepted, rejected, availability. Examination: Systemic physical examination (height, weight, heart, lung, abdomen ...). Obstetric examination (abdominal palpation, vaginal examination, examination of the breast. perineal examination). Biochemical evaluation: C. B. C - blood type – RH - antibody screen – urine analysis – serology (VDRL) Pap smear – Chlamydia – gonorrhea - rubella. Identification of high risk group: Characteristic of high risk group: Under 18 year or over 35 year or older at conception. Under or over weight or under l5 or gain over 30 pounds. Short stature 60 inches or less. Lack of money for pregnancy care, housing & environment. RH +ve baby with RH-ve mother. Genetically transferred or predisposed conditions. Drug addiction, alcoholism, DM, hypertension. Parity, multipara, grand Para, previous surgical delivery CS, previous out come premature. Prolonged or precipitate labor. Smoking one or more backs per day. Fear, anxiety & family problems. Services at subsequent visits: There is continuity & follow up of the all types of services provide at first visit. Specific process: Immunization: The women should be vaccinated against poliomyelitis if not already immune, She can vaccinate against diphtheria, tetanus& hepatitis B if she in risk. Other liver virus vaccines should be avoided during pregnancy. 10 Measles, mumps& rubella vaccine should be given 3 months prior to pregnancy. Assessment of fetal well-being: By assessment of fetal heart rate using F.H.R base line is 120 - 160 beat per minute using the following procedures: 1. Non stress test (NST). 2. Fetal movement monitoring. 3. Contraction stress test (CST). Assessment of fetal movement: Fetal activity begins around 18-20 weeks gestation, frequency of fetal movement wide variation average of 10 -12 times in hours. Methods of assessment: Count to ten: The woman should be instructed to do kick counts twice a day, morning & afternoon about I -2 hours after eating lying on her left side& counts the movements of fetus until she reaches a total 10 if fetus does not move with in half hour she should eat or drink something containing sugar& recount, if she does not feel movement during next 2 hours she should contact her physician. Count to fixed time during the day: The woman should instructed to do kick counts begin at 9am & end at 9pm, during this period the woman counts up to 10 movements & place an X at appropriate time on the card. 4. Biophysical profile (BPP). 5. Amniocentesis. 6. Doppler flow Studies. 7. Vibrocoustic stimulation test (VST). Referral services: Referral for the complicated cases of threatened abortion, accidental hemorrhage. Social services: This takes form of support or financial support. Out come of health services: The term out come is sometimes used to describe the results of an interaction between a client & care provider which can be seen to meet the criteria of a health benefit & also the out come can be measured in terms of mortality rates, incidence &prevalence of diseases. Health education according to levels of prevention: According to primary health care elements through assessment of activity of living. Provide appropriate health care about the following: Maintenance safe environment: Assess the house condition if it is stable for delivery & care for mother, her child, also assess basic sanitation. 11 Nutrition (eating & drinking): Assess the quality & quantity of what is eaten & drink. Instruct the pregnant woman how to meet the well balanced diet& riches with essential element as iron, folic acid & calcium. Assess the physical condition: Through out the pregnancy to ensure safe motherhood, good baby physical condition & also provide family planning services. Health education: For preventing health problems& controlling them. Immunization: against most communicable diseased major infection. Prevention & control of disease: local endemic diseases e.g. malaria. Appropriate treatment of common diseases. Prevision of drugs: especially the essential drugs. Communication: Assess the psychological condition as depressions pattern of communication (aggressive or hostile pattern), assess& help her to develop a good communication pattern. Mobilizing, working, planning & sleeping: Every pregnant woman can do exercises as walking, swimming & prenatal exercises. Most of them can work up until term with out complication but should take a rest during works hours, sleeping for 8 hours at night. Eliminating: teach the woman how to avoid constipation& maintain a regular bowel habits. Expressing sexuality: no restriction for normal client & instruct her about the alternative position. Schedule of antenatal visits: I time per month until 32 week - 2 times per month until 3 6 week - 4 times per month from 37 week until delivery. Items of health education: Follow up: Advice the mother to follow up according to the schedule of antenatal care that mentioned before, advise the mother to follow up immediately if any danger sings appears, describe the important of follow up to the mother. Danger signs of pregnancy: Every pregnant woman should be thought as a part of her antenatal care about the following warning sings: Vaginal bleeding including spotting. Persistant abdominal pain. Sever & persistent vomiting. Sudden gush of fluid from vagina. Absence or decrease fetal movement. Sever headache. Edema of hands, face, legs & feet. Fever above 100 F. Dizziness, blurred vision, double vision & spots before eyes. 12 Painful urination. Any woman developing any of the following warning sings should report the nearest clinic with out delay. Hygiene: Avoid hot bath because of fainting, avoid vaginal douche because of changing the vaginal PH & cause infection. Daily complete bath is very necessary. Breast examination & care: Careful examination of the nipples to be sure that it is not retracted or inverted, this will be easily traumatized as the baby can not fix on to the nipples properly, advise the mother to be mentally prepared for breast feeding, the breast should be supported with a well fitting brassiere for prevent or alleviating upper back ache & gives comfortable, advise the pregnant woman to expresses colostrums during the last trimester of pregnancy to prevent congestion. Diet: Daily requirement in pregnancy about 2500 calories. Purpose: 1. Growing fetus. 2. Maintain mother health. 3. Physical strength & vitality in labor. 4. Successful lactation. Activity: Avoid heavy work, house work continued but with exercises & rest. Exercises: Prenatal exercises are very important in pregnancy: Purpose: 1. To develop a good posture. 2. To reduce constipation & insomnia. 3. To alleviate discomvortable, postural back ache& fatigue. 4. To ensure good muscles tone& strength pelvic supports. 5 To develop good breathing habits, ensure good oxygen supply to the fetus. Guide lines for exercises during pregnancy: Maintain adequate fluid intake. Warm up slowly, use stretching exercises but avoid over stretching to prevent injury to ligaments. Avoid jerking or bouncing exercises. Be careful of loose throw rugs that could slip& cause injury. Exercises on regular basis (three times per week). After first trimester, avoid exercises that require supine position. Contraindications: Vaginal bleeding. 13 Sever anemia. History of preterm labor, Extreme over or under weight. Hypertension, heart, lung, thyroid diseases. Coitus: Sexual relations continue throughout normal pregnancy. Contraindications: Rupture of membranes. Preterm labor. Incompetent cervix. Spotting or bleeding. Clothes: It must be comfortable, washable, loose, mood fitting, adjustable & comfortable shoes. Traveling: It must be comfortable, train is safer than traveling by car for car traveling long journey break must taken every two hours air traveling is contraindication after 34 weeks of gestation. Hazards: Occupational hazards: lead, mercury, X ray s& ethylene oxide. Infection: rubella, toxoplasmosis, syphilis....................... Smoking & alcohol: increase risk for bleeding during pregnancy, prematurity, fetal death, mental retardation & congenital anomalies. Drugs: as sedative & analysis, anticoagulant, antithyrodism, hormones& antibiotics. Preparation for labor: Many women expecting a child have a profound desire to learn about pregnancy & birth & want to be as well prepared as possible for this events, many prenatal & child birth program are offer to meet this need in a variety of setting prenatal clinic & hospital. While program length& organization may differ among the various classes offered, all have certain content in common: Pain management & relaxation& breathing techniques that can be used during labor& delivery. Role of support person during labor& delivery. Possibility of high risk birth including CS. Preparation for parenting. Mental preparation: Fear from unknown acts through the cortex& hypothalamus on sympathetic system, tension is produced neither mother nor her uterus can property relax & exhaustion fallows. 14 Fear of labor is universal the most effective antidote is a doctor -client relationship which allows the mother to repose an absolute trust & confidence in her attendants, close personal involvement of the doctor is not always possible in the circumstance of present day obstetric practice, but antenatal instruction has been systematized. Minor Disorders of Pregnancy Minor disorders of pregnancy are not life threatening if treated promptly. They are caused by hormonal, metabolic and postural changes as the body accommodates to pregnancy. Minor Disorders of Pregnancy "First Trimester". Digestive System Morning sickness: Nausea and vomiting occur between 4-6 weeks gestation in about 50-70 percent of expectant mothers. It is not confined to early morning but can occur at any time during the day. Causes: The most likely cause is hormonal influences such as human chorionic gondotrophin, estrogen and progesterone. Emotional factors such as tension Management: Understanding the cause helps in coping. Adequate rest and relaxation will often help to reduce tension and prevent nausea. Eating six small meals a day rather than three large ones is advisable in an attempt to keep some food in the stomach at all times. Solid food may be tolerated better than liquid food, e.g. eating two or three crackers or a piece of dry toast with nothing to drink, immediately on awakening, then lying quietly in bed for 20-30 minutes and thereafter arising and eating a light breakfast. Carbohydrate snacks at bedtime and before rising can prevent hypoglycemia, which cause nausea and vomiting. Food should not have a strong odor, should not be either very hot or very cold, and fried or greasy foods should be avoided. Excessive salivation (ptyalism) It occurs from 8 weeks gestation and may accompany heartburn. Causes: is a pregnancy hormone. Management: Explanation and attentive listening are helpful. Heart burn: It is a burning sensation in the stomach that rises into the throat. Causes: •Progesterone hormone relaxes the cardiac sphincter of the stomach and allows reflux or bubbling back of gastric contents into the esophagus. 15 Management •Avoiding bending over and lying flat can prevent the reflux. •Sleeping with more pillows and lying on the right side can sometimes help. •Small frequent meals take up less room in the reduced stomach space and are digested more easily. •Resting in a semi-reclining position for about half an hour after meals is helpful. •For persistent heartburn, the doctor may prescribe antacids. Taking baking soda in a glass of water is contraindicated because of the possibility of retention of sodium and subsequent edema. Distress: A vague and ill-defined form of discomfort that occurs after eating. It resembles heartburn and makes the woman very uncomfortable. It is more likely to occur in a person who eats rapidly, or does not chew food thoroughly, or eats more at one time than the stomach can comfortably hold. Small amounts of food taken slowly and masticated thoroughly may prevent distress. Pica (Cravings): It is the term used when a mother craves certain foods or unnatural substances such as coal. Cause: is unknown, but may be due to pregnancy hormones and changes in metabolism. The nurse should be aware of this condition and seek medical advice if the substance craved is harmful to the fetus, e.g. lead. Flatulence: It may or may not be associated with heartburn; it is fairly common and rather uncomfortable. Causes: Bacterial action in the intestines, which result in the formation of gas. Hypochlorhydria during pregnancy and decreased motility of the entire gastrointestinal tract retard normal peristalsis and gas sometimes accumulates to a very uncomfortable extent. Management: •The diet should contain adequate amounts of fresh fruits, coarse vegetables, wholegrain breads and cereals and abundant fluids. •A regular time for defecation should be established and action upon the desire for defecation should be prompt. •When trying to have bowel movement, the woman should sit comfortably back on the commode seat with her feet flat on the floor or supported on a low step. •A glass of warm water in the morning before tea or breakfast may activate the gut and help regular bowel movement. •Exercise, especially walking, is also beneficial. •Laxatives and cathartics should be taken only if prescribed by the physician. 16 Irritant cathartics and enemas are to be avoided during pregnancy unless all other treatment has been ineffective. Mineral oil is contraindicated as it is ineffective and inhibits the absorption offalsoluble vitamins. Musculoskeletal System •Many women experience marked fatigue and lassitude early in pregnancy. • This feeling usually disappears by the end of the third month of pregnancy. • Women require many more hours of sleep during this time than they usually do. Genitourinary System • Changes in frequency of micturition. •In the early weeks of pregnancy, it occurs due to the pressure of the growing uterus on the bladder. •The pregnant woman should be reassured that the problem is resolved when the uterus rises into the abdomen after the 12th week. Circulatory System Fainting: In early pregnancy it may be due to the vasodilatation effect of progesterone. Management: The reason should be explained to the pregnant woman. The pregnant woman should avoid long periods of standing. Minor Discomforts of Pregnancy - Third Trimester Respiratory System Dyspnea: Causes: •Upward pressure of the uterus. •Increased sensitivity of the respiratory center to the carbon dioxide content of the blood. •It is aggravated by the mother lying down. Management: •Dyspnea is relieved by sitting up preferably in a straight chair, or being well propped up on pillows while lying down. •Lying on the back with the arms extended above the head and resting on the bed for a few minutes and before sleep at night. •Intercostal breathing may also give some relief. Digestive System Heart bum: Causes: 17 The pressure of the growing uterus on the stomach from about 30-40 weeks gestation. Management: Same as first trimester. Distress: Same as first trimester. Flatulence: Same as first trimester. Constipation: Causes: •The gut is displaced by the growing fetus. •Constipation is sometimes associated with the taking of oral iron. Management: Same as first trimester Musculoskeletal System Backache: Causes: •Backache may be due to muscular fatigue and strain that accompany poor body balance. •It may be due to increased lordosis during pregnancy in an effort to balance the body. •The pregnancy hormones sometimes soften the ligaments to such a degree that some support is needed. Management: •The pregnant woman is reassured that once birth has occurred, the ligaments will return to their pre-pregnant strength. •Exercises: improvement of posture and abdominal support aid in the prevention of backache. Round ligament pain: As the uterus grows, the round ligaments are stretched and cause abdominal pain and tenderness. Management: •Other causes of abdominal pain should be ruled out. •Rest and change of position usually will provide relief. •Cramps in the leg, numbness or tingling may be the result of overstretching of muscles and fascia. •They may be caused by circulatory impairment in the muscles owing to pressure of the large, heavy uterus on the pelvic veins. •A muscular tetany, resulting in leg cramps is sometimes caused by depression of available serum calcium, due to excess phosphorus in the blood. Management to relieve sudden cramps in the calf muscle: •In the sitting position, the woman may be advised to hold the knee straight and stretch the calf muscle by pulling the foot upwards (dorsiflexion). •She stands firmly on the affected leg and strides forward with the other leg. •She raises the foot of the bed about 25 cm. 18 •Application of a hot water bottle or gentle leg movement whilst in a warm bath enhances circulation and removes waste products from the muscle. The doctor may prescribe vitamin B complex and calcium. Fatigue: Tiredness is likely to reappear during the last trimester. Management is the same as first trimester. Genitourinary System Frequency of micturition: In the later weeks, it occurs because the fetal head usually enters the pelvis and reduces the space required by the bladder. The pregnant woman should be reassured that the problem is resolved after delivery. It is increased white, non-irritating vaginal discharge during the latter months of pregnancy. Management: •Douching should be avoided during pregnancy except when specifically ordered by the physician. •In addition to regular bathing, the vulva may be rinsed with warm water after each voiding. •Wearing cotton underwear and thin sanitary napkins usually gives a feeling of cleanliness and comfort. •If the discharge is abnormally profuse, irritating or foul smelling, and distressing by persistent itching and burning, medical investigation is needed for possible pathologic causes. Circulatory System Supine hypotensive syndrome: It may cause dizziness and a faint feeling during the latter part of pregnancy. The inferior vena cava may be compressed by pressure of the heavy pregnant uterus when the mother lies on her back causing decreased venous return to the hart. Management: •An immediate change of position to the left side is important for the mother's comfort. •A folded towel placed under the right hip will usually displace the uterus enough to prevent or relieve symptoms. Varicosities: Although varicose veins are confined to the legs, they may occur in the vulva. Varicose veins in the vulva are very rare and painful. Aching of the legs is a common symptom, even when the veins are not visible. Causes: 19 •Progesterone relaxes the smooth muscles of the veins and results in sluggish circulation. The valves of the dilated veins become inefficient and varicose veins result. •Varicose veins are most likely to develop in pregnant women with a family history or when they must stand for long periods of time or sit with legs dependent. Management: •One preventive measure is to sit down with the feet elevated. •If it is necessary to stand up, moving the legs about is better than standing still. Lying flat on the bed with the legs elevated 45 degrees, resting them on a footstool for 5-10 minutes three to four times a day will help reduce varicose veins and aching of the legs. Exercising the calf muscle by rising on to the toes or making circling movements with the ankles will help venous return Elastic stockings or spiral elastic bandages will give relief and help to prevent the veins from growing larger. They should be put on before getting up in the morning or after resting for few minutes with the leg elevated. Tight bands that interfere with return circulation should be avoided. Engorged veins in the vulva may be relieved by: 1. Lying flat and elevating the hips, or by adopting the elevated Sim's position for a few moments several times a day 2. Applying pressure to the vulva by means of a folded up hand towel, several sanitary pads or a panty girdle. Hemorrhoids: They are varicose veins that protrude from the rectum. They are extremely painful and may itch and bleed. Straining incident to constipation and pressure made by the enlarging uterus may cause them. Management: •Exacerbation of hemorrhoids will be reduced by avoidance of constipation. •Push them back gently into the rectum after lubricating the fingers with petroleum jelly or cold cream. Lying down with the hips elevated on a pillow and application of an ice bag or cold compresses to the anus usually give relief. The physician may prescribe medicated ointments, lotions or suppositories in case of sever condition. Operation is rarely resorted to during pregnancy because there is marked improvement after delivery. Edema: Swelling of the feet is very common during pregnancy and sometimes there is also swelling of the hands. Edema may be confined to the back of the ankles or may extend up to the legs and thighs and may even include the vulva. 20 It is physiological and results from mechanical interference with venous return and other circulatory modifications of pregnancy. Management: Lying down in a lateral position favors venous return from the lower extremities and decreases fluid retention. Sitting with the feet resting on a chair or footstool also will give some relief. For employed woman, elevation of the feet for 10-15 minutes, several times a day may increase her comfort. Dietary salt restriction is not indicated since sodium retention is not an etiologic factor. Sodium intake is necessary to maintain normal maternal and fetal electrolyte balance. The nurse must be keenly aware of the fact that although edema may be of mechanical origin, it is also a sign of toxemia and any swelling should prompt further investigation. Nervous System Carpal tunnel syndrome: It is a feeling of numbness and pins and needles in the fingers and hands in the morning or at any time of the day. It is caused by fluid retention, which creates edema and pressure on the median nerve. Management: Explain to the pregnant woman that this syndrome usually resolves spontaneously following delivery. Wearing a splint at night with the hand resting high on two or three pillows sometimes gives relief. The doctor may prescribe diuretics. Insomnia: 1. Physical reasons include: Difficulty in finding a comfortable position in bed because of a large and cumbersome body. Fetal activity is often vigorous and disturbing. Nocturnal frequency of micturation. 2. Psychological reasons include: The excitement and anticipation of birth may make it hard to relax and "turn off the mind for sleeping. Dreams about labor and the infant may be more frequent and sometimes frightening. Management: A warm drink or warm bath at bedtime or reading some light material in bed. A back rub with a soothing lotion promotes relaxation. Relaxation techniques learned in parenting classes are beneficial now. 21 Lying on the side and using small pillows or rolled towels to support the heavy abdomen and upper leg will usually permit greater muscle relaxation. It is helpful to concentrate on having every part of the body limp and then to make a conscious effort to have each inspiration and expiration exactly the same length and depth. Periods of rest and sleep during the day are important in order to compensate for loss of sleep during the night. Going to bed earlier may give the infant an active period and allow the pregnant woman to sleep at her usual time. Talking through common fears of pregnancy will relieve anxieties. Sensitive listening, explanation and reassurance can be helpful. A lie-in in the morning or a rest in the afternoon will help to prevent tiredness and depression that can occur in the last trimester of pregnancy. Sharing the pregnant woman's feeling can result in a sense of normality and lightness. Encouraging the pregnant woman to think about positive aspects of the infant and having a family may relieve depression due to hormonal changes towards the end of pregnancy. Skin: Itching: The breasts, abdomen and palms of the hands are commonly affected areas, although itching may be generalized to the entire body. Causes: The increased excretory function of the skin may result in the elimination of irritating substances by the skin glands. Stretching of the skin owing to weight gain, the growing uterus, and the fluid that is held in the skin. Generalized itching over the abdomen results from liver response to pregnancy hormones and raised bilurubin levels Management: Explain to the pregnant woman that itching will be reduced after childbirth. Bathing in tepid rather than hot, water and adding sodium bicarbonate (baking soda) to the bath water are soothing measures. Dabbing, rather than rubbing, to dry the skin with a towel will reduce stimulation of the skin and is less likely to produce itching. Lotions and oils are often helpful and rubbing them on the uncomfortable area is a constructive alternative to scratching. Sometimes, changing soaps or reducing the use of soap to a minimum will provide relief. Loose, nonrestrictive clothing is comfortable and not so apt to induce itching. Antihistamines that are prescribed by the doctor will provide limited comfort. 22 References 1. Dale. R., (1999): Fundamentals of obstetric & gynecology, 2nd ed, Lippincott Raven publishers, New York, P 243-246. ****************** 2. Martinal. B., (1998): Obstetric and gynecologic diagnosis & treatments, 7th ed, Lippincott Raven publishers, New York, P l134-1140. ****************** 3. Michael. P., (2001): Medicine Journal, Pregnancy & Postpartum Hemorrhage, August 20, Volume 2, Number 8 ****************** 23