Urinary system
advertisement
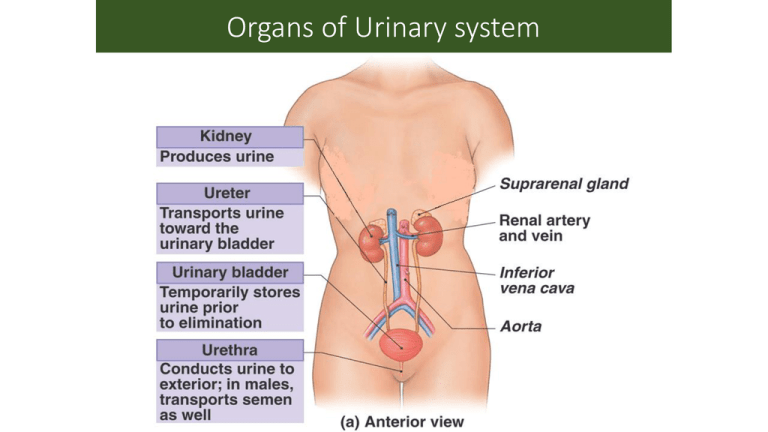
Organs of Urinary system Kidney function • Filter 200 liters of blood daily, allowing toxins, metabolic wastes, and excess ions to leave the body in urine • Regulate volume and chemical makeup of the blood • Maintain the proper balance between water and salts, and acids and bases • Gluconeogenesis during prolonged fasting • Production of rennin to help regulate blood pressure and erythropoietin to stimulate RBC production • Activation of vitamin D Other Urinary system organs function • Urinary bladder – Hollow Muscular Organ provides a temporary storage reservoir for urine • Paired ureters – transport urine from the kidneys to the bladder • Urethra – transports urine from the bladder out of the body Location & External Anatomy of kidney Lumbar vertebrae and rib cage partially protect Kidney location and External Anatomy • The bean-shaped kidneys • The right kidney is lower than the left because it is crowded by the liver • The lateral surface is convex and the medial surface is concave, with a vertical cleft called the renal hilus leading to the renal sinus • Ureters, renal blood vessels, lymphatics, and nerves enter and exit at the hilus External Anatomy of the Kidney The covering of kidney consists of three layers. The inner layer, the renal capsule, The middle layer, the adipose capsule, and the outer, renal fascia. • CT coverings • renal fascia: anchors kidneys to abdominal wall • adipose capsule: cushions kidney • renal capsule: encloses kidney like cellophane wrap Kidney location and External Anatomy Internal Anatomy • A frontal section shows three distinct regions • Cortex – the light colored, granular superficial region • Medulla – exhibits cone-shaped medullary (renal) pyramids Internal Anatomy In a typical adult kidney, the renal medulla is subdivided into 8 to 15 distinct conical or triangular structures known as renal pyramids. Blood vessels, nerves, and the ureter connect to the kidney at a prominent medial indentation known as the hilum Internal Anatomy Internal Anatomy Internal Anatomy • Renal pelvis – flat, funnel-shaped tube lateral to the hilus within the renal sinus • The renal pelvis: • Collect urine draining from papillae • Empty urine into the pelvis • Urine flows through the pelvis and ureters to the bladder Internal Anatomy Internal Anatomy Internal Anatomy Blood Supply Blood Supply • Approximately one-fourth (1200 ml) of systemic cardiac output flows through the kidneys each minute • Arterial flow into and venous flow out of the kidneys follow similar paths • The nerve supply is via the renal plexus Blood Supply correct sequence starting from the renal artery The Nephron • Nephrons are the structural and functional units that form urine, consisting of: • Glomerulus – a tuft of capillaries associated with a renal tubule • Glomerular (Bowman’s) capsule – blind, cup-shaped end of a renal tubule that completely surrounds the glomerulus • Kidney has over 1 million nephrons The Nephron Following is the order of parts of nephron through which the fluids moves from filtration membrane. 1. Renal corpuscle (the initial blood-filtering component of a nephron. It consists of two structures: a glomerulus and a Bowman's capsule) 2. Proximal tubule 3. Loop of henle 4. Distal tubule 5. Collecting duct Capillary Beds of the Nephron • Blood pressure in the glomerulus is high because: • Arterioles are high-resistance vessels • Afferent arterioles have larger diameters than efferent arterioles • Fluids and solutes (primarily glucose and amino acids) are forced out of the blood throughout the entire length of the glomerulus Two Types of Nephron • 1. Cortical nephrons – 85% of nephrons; located in the cortex • 2. Juxtamedullary nephrons: • • • • Are located at the cortex-medulla junction Have loops of Henle that deeply invade the medulla Have extensive thin segments Are involved in the production of concentrated urine Functions of different parts of the Nephron Proximal convoluted tubule : Active transport of sodium; water follows passively Descending limb of the nephron loop: passively permeable to water Ascending limb of the nephron loop: Active transport of sodium; impermeable to water Collecting duct : passively permeable to water under ADH stimulation. Mechanisms of Urine Formation 1. Glomerular filtration refers to the movement of fluid and solutes from the glomerular capillaries into Bowman’s space. 2. Tubular secretion refers to the secretion of solutes from the peritubular capillaries into the nephron. 3. Tubular reabsorption refers to the movement of materials from the filtrate in the nephron into the peritubular capillaries. Mechanisms of Urine Formation Hormonal Control of Kidney Function • ADH • Renin • Is an enzyme hormon • Secreted by posterior produced by kidneys, pituitary causes production of • Regulates water reabsorption angiotensin II that raises blood pressure at the distal convoluted tubule Aldosterone • Atrial natriuretic • Produced in adrenal cortex hormone • Affects Na+ and Cl- transport • Produced by heart when blood pressure increases in nephron and collecting • Inhibits ADH production ducts • Reduces ability of kidney • promotes sodium retention to concentrate urine and potassium loss from the blood across: the wall of the wall of the distal convoluted tubule?