Bioethical Issues In Healthcare
advertisement

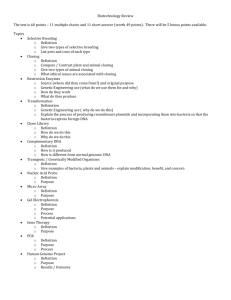
Bioethical Issues In Healthcare DEFINITION BIOETHICS is defined as discipline dealing with the ethical implications of biological research and applications especially in medicine. Bioethical Issues in Health care 1. Bioethical issues related to Beginning of Life – Family planning, Abortion, prenatal testing, sterilization, Artificial insemination, Assisted reproductive technology 2. Bioethical issues concerning Death – Advance Directives, Living wills, Euthanasia, Withdrawing and with holding treatment, Assisted suicide 3. Bioethical concerns related to sustaining Quality of Life – Organ and tissue Transplantation, Genetic engineering, human cloning 1. Bioethical a. b. c. d. e. f. g. issues related Beginning of Life: Family planning, Abortion, Prenatal testing, Sterilization, Surrogate mother Artificial insemination, Assisted reproductive technology to FAMILY PLANNING Refers to the various methods used to control the size of one’s family or to space birth. The religious, beliefs and personal values of individuals usually influence the methods and approaches used FAMILY PLANNING Natural Family Planning It is based on fertility awareness, which revolves around tracking a woman's reproductive cycle to determine the days of the month that she is most likely to conceive and avoiding sex during these times. Does not have the health side effects associated with artificial forms of birth control. Artificial Family Planning involves the use of birth control pills, devices, and sterilization surgeries. Sterilization, while permanent, has the highest rate of effectiveness in pregnancy prevention and can sometimes be reversed. Birth control methods such as condoms and spermicide can be purchased over the counter, and have high rates of effectiveness when used properly. PROBLEMS OF CONSENT AND FAMILY PLANNING In legal term the age of consent is the age at which one is capable of giving deliberate and voluntary agreement. The age of consent is established state by state and varies from 14 to age 18 and may different for males &females Emancipated minor : is an individual legally under the age of majority ,who are financially independed ,married or in the military ,may give consent for medical treatment Mature minor :is generally applied to individual In their mid to late teens who are considered mature enough to understand the treatment being recommended and provide informed consent ABORTION Is the termination of pregnancy before the viability of the fetus that is, any time before the end of the sixth month of gestation. Fetal Rights Fetal Rights are the legal or ethical rights of fetuses. The term is used most often in the context of the abortion debate, as the basis for an argument in support of the pro-life stance. Legislative measures sometimes seek to establish the right to life of the fetus from the moment of fertilization. Such laws regard the fetus as a person whose legal status is on par with that of any other member of the species homo sapiens Abortion: Its Bio-ethical Issues The two most obvious ways the issue has been framed is as a debate between those who are pro-life and those who are prochoice. Pro-life: They stance the frame of the issue as a refusal to “justify the deliberate killing of an innocent human being”. Pro –choice: They insist that those who would force a woman to bear her child are in no way acting morally. Instead, pro-lifers are perpetuating abusive patriarchal structures in which women are denied a right to be their own decision-makers about what they want to do with their body. Both of these positions often center the debate on the status of the fetus: is it a full-fledged person with all the rights and dignity we accord to other fully grown persons. PRENATAL TESTING Sonography, Amniocentesis and CVS: to detect genetic abnormalities. Ethical concern: Govt. may make amniocentesis n abortion of all defective fetuses mandatory. Couples may be stressed as carrying defective gene. ASSISTED REPRODUCTIVE TECHNOLOGY (ART) The IVF technology is a boon to childless couples. A procedure in which a fine catheter (tube) is inserted through the cervix (the natural opening of the uterus) into the uterus (the womb) to deposit a sperm sample from the husband or from a donor. The purpose of this procedure is to achieve fertilization and pregnancy. Initially this technique was pioneered by Prof. Robert Winston during 1970s which was later applied by P. Steptoe and R. Edwards for the production of first test tube baby. The first IVF baby - Louse Joy Brown, who was born on July 25, 1978. Artificial Insemination AIH (artificial insemination by husband) AID (artificial insemination by donor) AIH is also known as AID is also called homologous insemination. A procedure in which a fine catheter (tube) is inserted through the cervix (the natural opening of the uterus) into the uterus (the womb) to deposit a sperm sample from the woman's mate directly into the uterus. heterologous insemination. A procedure in which a fine catheter (tube) is inserted through the cervix (the natural opening of the uterus) into the uterus (the womb) to deposit a sperm sample from a donor other than the woman's mate directly into the uterus. Ethical concerns Woman may have multiple births as several fertilized ova are returned to uterus to ensure that at least one will survive. At times this lead to abortion leading to financial and emotional costs. What to be done with fertilized ova that are not returned to the uterus? Donate, freeze (how long) or thrown away (abortion)? SURROGATE MOTHERS She is the one who agrees to bear a child conceived through artificial insemination / IVF and relinquish the baby at birth to others for rearing. A formal, contractual relationship is usually established between the surrogate & the contracting family. ETHICAL CONCERNS What happens if the child is born with an anomaly and family refuses to take the child? What if the surrogate becomes attached to the child & refuses to give up custody? What happens if the parents divorce before the child is born & wish to nullify the contract? What will happen to the child? 2. Bioethical issues concerning Death – a. Futile treatments b. Advance Directives, c. Living wills, d. Euthanasia, e. Withdrawing and with holding treatment, f. Assisted suicide PLANNING FOR END OF LIFE ISSUES FUTILE TREATMENTS (medications, devices / therapy): are those that are evaluated by the healthcare team, family or both as being nonbeneficial or harmful to the patient in as much as they cannot cure or reverse the underlying disease. For e.g. terminally ill cancer patient. ADVANCE DIRECTIVES & LIVING WILL ADVANCE DIRECTIVES are legal documents that indicate the wishes of an individual with regard to end of life issues & LIVING WILL allows individuals to identify what measures to include in care if they become terminally ill. Ethical concern: they are not clear, specific, misunderstood, signing for power of attorney for healthcare. EUTHANASIA: the act or method of causing death painlessly so as to end suffering. CLASSIFICATION POSITIVE / ACTIVE EUTHANASIA: •It occurs in a situation in which the physician prescribes, supplies or administers an agent that results in death. •Medications given for the comfort of the dying patient may be ethically justifiable even if they hasten death to some extent. NEGATIVE / PASSIVE EUTHANASIA: •It refers to a situation in which no extraordinary measures are undertaken to sustain life. •This concept has resulted in (no codes” also called as do not resuscitate order (DNR) in hospital.; WITHDRAWING AND WITHHOLDING TREATMENT: This has been described mainly in situations related to technical interventions (ventilator, hemo-dialysis). Can also be applied by extension to chemotherapy, artificial hydration to prolong life beyond expectation, to delay death. ASSISTED SUICIDE: involves helping another end his or her life. Role of the nurse should be directed toward reversing the despair and pain experienced in the last stages of life, and in fulfilling the obligation to provide competent, comprehensive & compassionate end of life care (ANA, 1994). 3. Bioethical concerns related to sustaining Quality of Life – a. Organ and tissue Transplantation, b. Genetic engineering, c. Human cloning Organ and tissue Transplantation Organ transplantation is the process by which an entire organ is removed & replaced by a corresponding part. Donor can be living or recently deceased. Genetic Engineering Genetic Engineering, also called genetic modification, is the human manipulation of an organism's genetic material in a way that does not occur under natural conditions. Genetic engineering works because there is one language of life: genes Genetic engineering examples: Genetic engineering has created a goat with spider genes that creates "silk" in its milk. Insertion of human genes into sheep so that they secrete alpha-1 antitrypsin in their milk - a useful substance in treating some cases of lung disease. Human Cloning Human Cloning is a type of genetic engineering, but is not the same as true genetic manipulation. In human cloning, the aim is to duplicate the genes of an existing person so that an identical set is inside a human egg. The result is intended to be a cloned twin, perhaps of a dead child. Genetic engineering in its fullest form would result in the child produced having unique genes - as a result of laboratory interference, and therefore the child will not be an identikit twin Cloning Ethical Debate Argument against Human Cloning: Human Cloning Constitutes Unethical Experimentation That human cloning threatens identity and individuality. That human cloning turns procreation into manufacture. That human cloning means dictatorship over children and the perversion of parenthood. Scientific Debate: Human Cloning could save many lives The Quality of Humans could be improved To develop new organs for transplantation in humans. This could decrease the time a patient waits for a transplant