Male reproductive system practical Dr: Salah Ahmed

Male reproductive system practical
Dr: Salah Ahmed
Atrophied testis secondary to cryptorchidism
Cryptorchidism:- failure of testicular descent into the scrotum
- complications: 1-testicular atrophy 2- sterility
3- malignant transformation
Testicular atrophy:- may be associated with :
1- orchitis , especially mumps orchitis
2- trauma
3- cryptorchidism
4- Klinefelter`s syndrome
5- chronic debilitating disease
6- old age
7- hormonal excess or deficiency ( liver cirrhosis, estrogen therapy, hypothalamus or pituitary disorders )
8- radiation and chemotherapy
Normal testicular atrophy
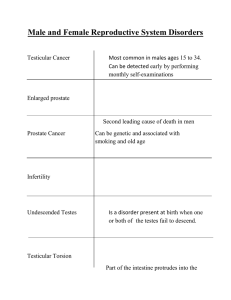
Testicular tumors:
- 95% of testicular tumors arise from germ cells, and always are malignant
- sex cord/stromal tumors are uncommon, usually benign
- originate from intratubular germ cell neoplasia
1- Seminomas: 1- classic seminomas: most common
2- spermatocytic seminoma: common in older age than classic, not originate from ITGCN, mets are rare
- the cells express hCG
Seminoma
:- soft usually gray-white tumors
(nests of large cells with distinct borders, clear cytoplasm and round nuclei with prominent nucleoli, separated by fibrous septa with lymphocytic infiltration)
•
•
•
- ill-defined mass
- composed of large and primitive looking cells, with basophilic cytoplasm, indistinct cell borders, and large nuclei with prominent nucleoli in solid sheets, glandular pattern and irregular papillae
2- Embryonal carcinomas:
- rare tumor (2 – 3%)
- majority of cases are mixed
microcystic tissue and a papillary structure resembling a developing glomerulus. hyaline droplets of α-fetoprotein is present
• 3- Yolk sac tumors (endodermal sinus tumors):
3- Yolk sac tumors (endodermal sinus tumors):
Common in children under 3 years , cells express α-fetoprotein
- mixed with embryonal carcinoma
Composed of small cells intermingled with large eosinophilic cells with multiple nuclei
4- Testicular choriocarcinomas:
- it is a rare tumor
- highly malignant tumor
5- Testicular teratomas:
- Morphology: - tumors form firm masses that on cut surface often contain cysts
- three variants of teratoma: a) Mature teratoma: contains fully differentiated tissues b) Immature teratoma: contains immature elements (fetal tissue) c) Teratoma with somatic-type malignancies: characterized by the development of frank malignancy (squamous cell carcinoma or adenocarcinoma
Mature teratoma
Testicular teratomas contain mature cells from endodermal, mesodermal, and ectodermal lines.
Pictured here are four different fields from the same tumor containing (A) neural (ectodermal),
(B) glandular (endodermal), (C) cartilaginous (mesodermal), and (D) squamous epithelial elements
• Benign prostatic hyperplasia (nodular hyperplasia) :
- BPH is not a premalignant condition
- is the most frequent cause of urinary tract obstruction
- it is common in older men
- Pathogenesis :
- dihydrotestosterone (DHT) a metabolite of testosterone is the mediator of prostatic growth
- DHT is synthesized by the action of enzyme 5- alpha- reductase
- BPH may also be caused by age-related increase in estrogen, which promotes expression of receptors for DHT
Morphology :
- both glands and stroma proliferate
- the prostate appears nodular
- the nodules arise commonly in transitional zone
- hyperplasia begins in transitional zone then going peripherally
BPH
enlarged in size with nodularity, hyperplastic glands with corpora amylacia
• Prostatic adenocarcinoma :
- more common in blacks than in white
- the common age at diagnosis is 72 years old ( older men )
- Pathogenesis :
- remains unknown but clinical and epidemiological data suggest that advancing age, race, hormonal influence, genetic factors and environmental factors (diet) all contribute
- Morphology :
- almost all carcinomas originate in the peripheral zone
- grossly usually yellow in colour .
- It is solid not nodular as in BPH
- either well (glandular), moderate (glands+ sheets), poorly
(sheets of malignant cells) differentiated
Metastasis occurs by :
1- direct local invasion (seminal vesicles, base of bladder, rectum)
2- hematogenous to bone (lumbar spine, proximal femur, pelvis) and viscera
3- lymphatic to obturator, perivesical, iliac, perisacral and para -aortic nodes.
- prostatic carcinoma associated with increase in prostate specific antigen (PSA) : used to diagnose prostate cancer, and distinguish it from BPH.
- also characterized by increased serum prostatic acid phosphatase when tumour penetrates the capsule into adjacent tissues.
- bony metastasis associated with increase in serum alkaline phosphatase
* Prostate-specific antigen (PSA) ( gamma-seminoprotein or kallikrein-3)
- is a glycoprotein enzyme
- is secreted by the epithelial cells of the prostate gland
- is produced for the ejaculate, where it liquefies semen and allows sperm to swim
- PSA is present in small quantities in the serum of men with healthy prostates, but is often elevated in the presence of prostate cancer or other prostate disorders
High power : back to back arrangement of the malignant glands and cells with prominent nuclei.