Labeled Immunoassays 8
advertisement

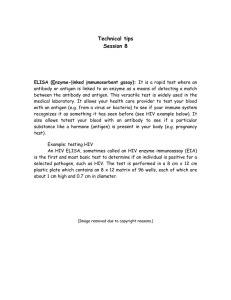
Labeled Immunoassays Part 2 Enzyme Linked Immunosorbent Assay (ELISA) Labeled Immunoassays • The basic underlying principles of indicator labeled immunoassays are the same. • There are differences with respect to the detail of the protocols. • The designation given to each test differs according to the label used to detect the antigen/ antibody complexes. Enzyme Linked Immunosorbent Assay (ELISA) • One of many assays collectively called enzyme immunoassays (EIA). • The enzyme used an indicator molecule. • The enzyme does not provide detection directly. • The action of the enzyme on a substrate that results in a change in the properties of the solution. • The substrate is brokendown by the enzyme to produce chromogenic, fluorogenic or luminescent products. ELISA • Can Be Used To Detect Both Antibody and Antigen • Very Sensitive, ng & pg/mL • Relies on Monoclonal Abs Enzymes used in ELISA • Enzymes used as labels for immunoassay are chosen according to the following criteria: number of substrate molecules converted per molecule of enzyme purity sensitivity ease and speed of detection stability absence of interfering factors in patient samples in addition, availability and cost of enzyme and substrate. Enzymes used in ELISA • The most commonly used enzymes are: horseradish peroxidase (HRP) and alkaline phosphatase (AP). • Each has a high turnover number (rapid conversion of chromogenic substrate to coloured product) resulting in high sensitivity. • An array of chromogenic, fluorogenic and chemiluminescent substrates is available for use with either enzyme. • Other enzymes have been used as well, but they have not gained widespread acceptance because of limited substrate options. – These include beta-galactosidase, acetylcholinesterase and catalase. Enzyme Substrates • A large selection of substrates is available for performing the ELISA with an HRP or AP conjugate. • A common ELISA substrate for HRP: – tetramethylbenzidine (TMB), – TMB yields a blue reaction product that is watersoluble and absorbs light at 450 nm. • The most common ELISA substrate for alkaline phosphatase: – the chromogen p-nitrophenyl phosphate (PNPP) – PNPP yields a yellow reaction product that is watersoluble and absorbs light at 405 nm. Linkage of Enzyme • The enzyme label is linked to antibody or analyte by several means. Glutaraldehyde is often used as a crosslinker to join amino groups of the enzyme and the molecule to be labeled. Maleimide derivatives are also used to attach the enzyme label. Coating of microplate • A key feature of the solid-phase ELISA is that antigens or antibodies can be attached to surfaces easily by passive adsorption. • This process is commonly called coating. • Most proteins adsorb to plastic surfaces, probably as a result of hydrophobic interactions between nonpolar protein substructures and the plastic matrix. • Since most of proteins' hydrophilic residues are at the outside and most of the hydrophobic residues orientated towards the inside. • Partial denaturation of some proteins results in exposure of hydrophobic regions and ensures firmer interaction with the plastic. • This can be achieved by exposing proteins to low pH or mild detergent ELISA Protocol 1- Coating antibody or antigen onto the microplate Dilute the protein to be coated in a buffer such as PBS or Carbonate-Bicarbonate and add 100 μl of this solution per well. Incubate for 18-20 hours at room temperature or 4°C. Block unoccupied sites with a blocking agent (200-300 μl/well) Store plate at 4°C with a desiccant for future use. ELISA Protocol 1- Coat solid phase with •antigen when analysing antibody •antibody when analysing antigen Analyte = antibody Analyte = antigen Incubate, wash ELISA Protocol 2- Blockage of free binding sites Block the unoccupied sites on the surface of the well to reduce the amount of nonspecific binding of proteins A variety of blocking buffers ranging from nonfat milk to highly purified proteins have been used to block unreacted sites. The blocking buffer should improve the sensitivity of the assay by reducing the background interference. An individual blocking buffer will not be compatible with every system; a variety of blockers in both Tris buffered saline (TBS) and phosphate buffered saline (PBS) are available. The proper choice of blocker for a given assay depends on: the antigen itself and on the type of enzyme conjugate to be used. (eg. AP + Blocking Buffer in TBS, PBS interferes with AP) ELISA Protocol 2- Block free binding sites. Incubate. Wash. Analyte = antibody Analyte = antigen ELISA Protocol 3. Add sample. Incubate. Wash Analyte = antibody Analyte = antigen ELISA Protocol 4. Add conjugate. Incubate. Wash. E E Analyte = antibody E E Analyte = antigen 5. Add substrate 6. Incubate, stop, measure colour change ENZYME Colourless OD CONCENTRATION Types of Enzyme Immunoassay A- Heterogenous Enzyme Immunoassay Three main methods: 1. Competitive ELISA 2. Indirect ELISA 3. Sandwich ELISA 1- Competitive ELISA • Enzyme activity is inversely proportional to the concentration of the test substance. • A sensitivity of nanograms (10-9 g)/ml can be achieved. • This method can be used for measurement of small molecules that are relatively pure, • such as insulin • and estrogen. 1- Competitive ELISA COMPETITION ELISA TO DETECT ANTIGENS (antibody-coated plate) 1. Anti-analyte 1- Competitive ELISA Low [analyte] High [analyte] 2. Analyte-E + sample 1. Anti-analyte 1- Competitive ELISA Low [analyte] High [analyte] 3. Wash E E E 2. Analyte-E E E + sample 1. Anti-analyte E E 1- Competitive ELISA Low [analyte] High [analyte] 4. Substrate 3. Wash 2. Analyte-E + sample 1. Analyte 2- Noncompetitive ELISA or Indirect ELISA • Indirect ELISA is more sensitive than the competitive. • Much assays are capable of detecting concentrations of less than 1 pg/ml (10-12 g)/ml. 2- Indirect ELISA • • screening hybridoma supernatants detecting clinically important antibodies - autoantibodies - anti-pathogens - anti-allergens 1. Antigen 2- Indirect ELISA 2. Sample (human) antibody 1. Antigen 2- Indirect ELISA E E 3. Anti-(human) Ig-enzyme 2. Sample (human) antibody 1. Antigen E E E E 2- Indirect ELISA 4. Substrate 3. Anti-(human) Ig-enzyme 2. Sample (human) antibody 1. Antigen E E E 3- Sandwich ELISA • If the antibody is bound to the solid phase, • These assays are called sandwich immunoassays or capture assays • Antigens captured in these assays must have multiple epitopes. 3- Sandwich ELISA eg. hormones drugs tumour antigens cytokines 1. Anti-analyte 3- Sandwich ELISA 2. Sample 1. Anti-analyte 3- Sandwich ELISA E 3. Anti-analyte-enzyme 2. Sample 1. Anti-analyte E 3- Sandwich ELISA 3. Or: anti-analyte-biotin followed by streptavidin-enzyme 2. Sample 1. Anti-analyte E S E-S B S-E E S E-S B S-E ANTIBODY SANDWICH ELISA TO DETECT ANTIGENS 4. Substrate 3. Or: anti-analyte-biotin followed by streptavidin-enzyme 2. Sample 1. Anti-analyte Membrane based cassette assays • This type of ELISA is rapid, easy to perform and give reproducible results. • Designated primarily for primary care clinics and home testing • Many of these have been modified for increased sensitivity and can be made semiquantitative for use in a clinical laboratory by reading the color reaction with a densitometer. Membrane based cassette assays(Dipsticks) Apply sample solution, upon application of sample biochemicals dissolve Positive: no antigen Immobilised Antibody area Control area Negative: antigen present • Immunochromatography • Biochemical components are separated across an absorbent membrane into discrete distinct regions. QUALITATIVE TEST Control Monoclonal Ab labeled with enzyme Immoblized Ab + substrate support Sample pad B- Homogenous Enzyme Immunoassay • Homogeneous methods have been generally applied to the measurement of small analytes such as abused and therapeutic drugs. • Since homogeneous methods do not require the separation of the bound Ab-Ag* from the free Ag*, they are generally much easier and faster to perform. • Homogenous methods are generally less sensitive than heterogeneous assays. • They are based on the principle of change in enzyme activity as specific antigen-antibody combination occurs. • Enzymatic activity can be altered by steric exclusion of the substrate, or there may be changes in the conformation structure of the enzyme. • Enzymes of this type include lysozyme, amaylase, trypsin and others. 1- Enzyme-multiplied immunoassay • It is based on the principle of change in enzyme activity as specific antigen-antibody combination occurs. Reagent antigen is labeled with an enzyme tag. When antibody binds to specific determinant sites on the antigen, the active site on the enzyme is blocked, resulting in a measurable loss of activity. • Free analyte (antigen) competes with enzyme-labeled analyte for a limited number of antibody-binding sites, so this is a competitive assay. Enzyme activity is directly in proportion to the concentration of patient antigen or hapten present in the test solution. A physical separation of bound and free analyte is thus not necessary. Advantages & Disadvantages • Advantages of ELISA High sensitivity No need for expensive instruments Reagents are inexpensive and have a long shelf time No disposal problems, or health hazard of radiation • Disadvantages of ELISA Some specimens may contain natural inhibitors Size of enzyme may be a limiting factor in the design of some assays Nonspecific binding and sensitivity of enzymes to temperature Toxoplasma gondii • Toxoplasma gondii is a small intracellular parasite, whose life cycle has a sexual and an asexual phase. • Sexual development is restricted to the intestinal cells of (probably exclusively) cats; the oocysts formed are excreted and due to their resistant cell walls they may be infectious under advantageous circumstances for at least 1 year. • Animals and man are intermediate hosts for the asexual proliferation of T. gondii: the ingested parasites will proliferate explosively within the host cells lysing them eventually. • They disseminate throughout the body via circulation and lymphatic system and may infect any cell type. Cysts are virtually impossible to be killed in the intermediate host. Toxoplasma gondii • Most T. gondii infections are asymptomatic or present with a transient • febrile illness, often with lymphadenopathy. • Primary infections acquired during pregnancy can cause • • • • • stillbirth or congenital abnormalities, including blindness, encephalomyelitis, impaired brain functions and convulsions in the newborn. • Infections can also be more severe in individuals who are infected with HIV or who are otherwise immunocompromised. • Toxoplasmosis can be treated with antibiotics but early detection of the disease is crucial for effective therapy. Test Principle • Microtiter wells are coated with antigens. • This constitutes the solid phase. • Patient's sample is added to the wells and any antibodies specific for the antigen present will bind to the solid phase. • After removal of unbound material, anti-human IgG or IgM conjugated to an enzyme (alkaline phosphatase) is allowed to react with the immune complex. • After removal of excess conjugate by washing, an appropriate substrate (paranitrophenylphosphate) is added, with which the conjugated enzyme reacts producing a coloured derivative of the substrate. • The colour intensity is proportional to the level of specific antibody bound and can be quantified photometrically. Test procedure • Place the required number of cavities in the frame and prepare a protocol sheet. • Prepare the diluted washing solution • Wash microplate strips once with working washing solution. Remove remaining liquid by tapping on absorbent paper • Dilute test sera by adding 10 µl of sample to 1 ml of diluent • Calibrators 0, 6, 60 and 240 IU/ml are diluted in the same manner • Add each 200 μl of diluted sample or calibrators into the appropriate wells – well A1 0 IU/ml – well B1 6 IU/ml – well C1 60 IU/ml – well D1 240 IU/ml – well E1, F1, G1, etc.. 200 µl of diluted sample Test procedure • • • Sample incubation for 60 minutes (+/- 5 min) at 37°C (+/- 1°C). Prepare working conjugate 15 minutes before the end of first incubation period After incubation wash all wells with washing solution (by automated washer or manually): • • • • • aspirate or shake out the incubation solution fill each well with 300 μl washing solution aspirate or shake out the washing buffer repeat the washing procedure 2 times (altogether 3 times!) dry by tapping the microtest plate on a paper towel Test procedure • Addition of conjugate • • • • Add 200 μl of working-conjugate to the appropriate well Conjugate incubation for 60 minutes (+/- 1 min) * at 37°C (+/- 1°C) After incubation wash all wells 4 times with washing solution (see above) Addition of substrate • • Add 200 μl substrate solution to each well Substrate incubation for 30 minutes (+/- 1 min) * at 37°C (+/- 1°C) in the dark Test procedure • Stopping of the reaction • • Add 100 μl stopping solution to each well, shake microtest plate gently to mix. Read optical density • Read OD within 30 minutes at 450 nm against substrate blank Results • The presence and quantity of IgG antibodies to T. gondii in the test sample is determined by comparing the optical density (OD) of the test sample to a standard range. • For validation of the test the following criteria must be met: • OD values – OD R3 ≤ 0.200 – OD R4c ≥ 1.000 • Ratio: – OD R4a / OD R3 ≥ 2 Results • After drawing the curve from the concentration of standards on the x-axis with absorbance of standards on the y-axis, find the value corresponding to the OD reading of the test sample on the y-axis and draw a horizontal line to the standard curve. At the point of intersection with the standard curve draw a vertical line to the x-axis. Read the concentration in IU/ml at the point of intersection with the x-axis. • Interpretation of results • Negative result: titer < 6 IU/ml • Positive result: > 9 IU/ml