salivary gland disorders

Dr. Rupak Sethuraman
Specific Learning Objective
To identify the complaint with which patient may come to the dental hospital.
To ask relevant question to the patient in order to get a diagnosis.
Advise a reliable treatment to the patient.
FORMAT
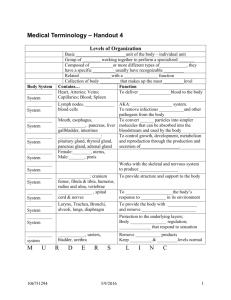
SALIVARY GLAND ANATOMY
Developmental Abnormalities
Accessory Salivary Ducts
Diverticuli
Darier’s Disease
Sialolithiasis (Salivary Stones)
Mucoceles
Inflammatory and Reactive Lesions
Immune Conditions
ANATOMY
STRUCTURE OF SALIVARY GLANDS
The main excretory duct
Smaller striated ducts
Intercalated ducts
Blind microvillus
Terminal end piece
Developmental Abnormalities
Accessory duct
Diverticuli – is a pouch or sac protruding from the wall of a duct
Darier’s Disease
Duct dilation, with periodic stricture affecting the main ducts.
Symptoms of occasional obstructive
sialadenitis have been reported.
Sialolithiasis (Salivary Stones)
Stones are most commonly found in the
, where stones can obstruct .
Associated with chronic infection
( of the glands, dehydration ( ), and/or increased local levels of calcium, but in
) many cases can arise
Pain, when present, usually originates from the floor of the mouth, although in many cases the stones cause only intermittent swelling.
Since chewing promotes release of saliva, symptoms tend to increase during meals.
A palpable lump or visible swelling in the area of the gland is often noted.
Complications include persistent obstruction of the duct, leading to bacterial invasion, overgrowth and infection (sialadenitis).
DIAGNOSIS
Radiographs are helpful to visualize sialoliths; however, poorly calcified stones may not be readily identifiable .
An occlusal radiograph is recommended for submandibular glands.
Stones in the parotid gland can be more difficult to visualize due to the superimposition of other anatomic structures; therefore, requesting proper radiographic views is important.
An Antero Posterior (AP) view of the face is useful for visualization of a parotid stone.
An occlusal film placed intraorally adjacent to the duct may also help.
Computed Tomography (CT) images may be used for the detection of sialoliths and have a 10-fold greater sensitivity than plain-film radiography for detecting calcifications.
A relatively new technique for visualizing and subsequently removing sialoliths is sialoendoscopy, where a small (<1 mm diameter) probe attached to a specially designed endoscopic unit can explore primary and secondary ductal systems.
The endoscopic unit also has a surgical tip that can obtain soft tissue biopsies and help remove calcified materials using a minimally invasive technique under local anesthesia.
TREATMENT
During the acute phase, therapy is primarily supportive.
Standard care includes analgesics, hydration, antibiotics, and antipyretics, as necessary.
In pronounced exacerbations, surgical intervention for drainage or removal of the stone may be required.
Stones at or near the orifice of the duct can often be removed transorally by milking the gland, but deeper stones require removal with surgery or sialoendoscopy.
After the acute phase has subsided, surgery can be performed.
Location within the duct determines the type of surgery planned.
For example, stones located in the intraglandular portion of the duct require complete removal of the gland.
Alternatively, if the stone can be removed from the duct without damaging the body of the gland, nearly complete salivary recovery can occur.
Lithotripsy and sialoendoscopy can be helpful as noninvasive or minimally invasive treatments for sialoliths.
Ultrasonography will detect stones (diameter >2 mm) and extracorporeal lithotripsy will fragment the stone, although repeat lithotripsy procedures may be needed.
Lithotripsy has been reported to be more effective for parotid versus submandibular calculi (57% vs 33%), with a 68% success rate after 10 years.
Clinical Presentation –
History – patient complains of accidental biting of the lower lip 2 days back. Patient has severe pain after biting which increases when patient touches his lower lip by tongue or hand. Later pain gradually reduces by itself.
Sign – there is presence of swelling in the lower lip which is red in color and has a laceration wound in between. It is tender on palpation.
Symptom - there is pain and discomfort.
Patient is unable to have his regular hot food.
Clinical Appearance – is seen in lower lip at the level of occlusion of the teeth. Has bite mark with laceration. It is bluish red in color, slightly compressible, fluctuant in nature.
MUCOCELE
“Mucocele” is a clinical term that describes swelling caused by the accummulation of saliva at the site of a traumatized or obstructed minor salivary gland duct.
Mucoceles are classified as
Extravasation type and
Retention type
ETIOLOGY
Extravasation Type - Trauma to a minor salivary gland excretory duct. Laceration of the duct results in the pooling of saliva in the adjacent submucosal tissue and consequent swelling.
Retention Type – caused by obstruction of a minor salivary gland duct by calculus or possibly by the contraction of scar tissue.
TREATMENT –
Symptomatic Treatment –
Avoid biting on the swelling again.
Avoid having hot food from the same side.
Apply ice for 30sec and then leave it for 2minutes then can apply again.
Medical Treatment –
Apply vaseline to avoid super infection.
Apply anesthetic gel like mucopain ointment – diclofenac; meftal gel.
Gel should be applied before the effect of the gel is reduced to avoid pain.
Definitive treatment –
Surgical excision followed by suture placement.
Case – 2
Same case with a modification in history and size of the swelling is reduced.
History – patient complains of swelling in the lower lip present since last 3months or more.
Patient had pain as it started due to biting but has gradually reduced.
Now patient has discomfort while speech and mastication.
Clinical Examination – swelling is pale in color, has well defined borders, no sign of bleeding or discharge. Is seen at the line of occlusion.
Palpation – swelling is soft to firm in consistency, moderately compressible, patient complains of dull pain on pressing with force.
FIBROMA
•
•
•
The initiating injury regardless of type inflammation granulation tissue
Fibrous inflammatory hyperplasias may occur as either pedunculated or sessile
Clinically it appears as asymptomatic smoothly contoured pale appearance .
It is soft, spongy and blanches on pressure.
Treatment – surgical excision.
RANULA
A ranula is an extravasation cyst arising from the sublingual gland.
Typically ranula is associated with cervical prolongation.
It might be an embryonic remnant.
C/F - The classic ranula presents as a blue domed, translucent swelling in the floor of the mouth, resembling the “belly of a frog.”
A rare case of an extensive plunging ranula: Discussion of imaging, diagnosis, and management Shelley
M, Yeung K, Bowley N, Sneddon K,
Sussex W, Oral Surg Oral
Med Oral Pathol Oral Radiol Endod
2002;93:743-6
DEEP/PLUNGING RANULA
A plunging ranula manifests itself as a swelling in the neck.
Swelling shows no change at meal times.
Most of the time swelling is not seen intraorally as the collection is below mylohyoid.
Palpation – Bidigital palpation
Aspiration – reveals numerous macrophages, higher levels of salivary amylase and protein contents compared with serum but no epithelial cells
Contrast medium guided plain radiography
MRI & CT
Complications – it may burst due to repeated trauma or recurrence
Management – surgical excision.
Inflammatory and Reactive
Lesions
NECROTIZING SIALOMETAPLASIA
Benign self-limiting reactive inflammatory disorder
Has a rapid onset.
Lesions occur predominantly on the palate but can be seen on buccal pad of fat.
Lesions initially present as a tender erythematous nodule.
Once the mucosa breaks down, a deep ulceration with a yellowish base forms.
Even big lesions have moderate degree of dull pain.
Seen usually after a dental treatment like filling, scaling etc.
Diagnosis requires an adequate biopsy specimen and histopathologic diagnosis from a pathologist with expertise in oral lesions.
In addition to the specimen, a complete clinical history should be provided to the pathologist to aid in distinguishing this lesion from squamous cell carcinoma.
Treatment –
Self-limiting
Lasts approximately 6 weeks, and heals by secondary intention.
ALLERGIC SIALADENITIS
Usually related to sudden use of drugs.
Involves more than one salivary gland.
Characterized by itching or discomfort in the gland region and history reveals change in food habits or use of particular drug.
Treatment –
It corrects once the medication is stopped.
Drugs which have salivary gland enlargement as a potential side effect include
phenobarbital,
phenothiazine,
ethambutol,
sulfisoxazole,
Iodine compounds, isoproterenol, and
heavy metals.
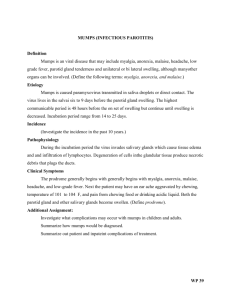
Case – 3
Patients complains of sudden onset of unilateral or bilateral salivary gland enlargement
The involved gland is painful, indurated, and tender to palpation, overlying skin may be erythematous.
A purulent discharge may be expressed from the duct orifice.
Patient has fever . On opening the mouth he has bad odor, poor oral hygiene.
History – of reduced salivary flow since last 10 years.
Investigations –
Ultrasonography
Culture of purulent exudate.
Bacterial Sialadenitis
TREATMENT
If a purulent discharge is present, empiric administration of a penicillinase- resistant antistaphylococcal antibiotic is indicated.
Patients should be instructed to “milk” the involved gland several times throughout the day.
Increased hydration, salivary stimulants (sugar-free candies, gums, mints), and improved oral hygiene are required.
With these measures, significant improvement should be observed within 24 to 48 hours. If this does not occur, then incision and drainage should be considered
Immune Conditions –
BENIGN LYMPHOEPITHELIAL LESION
(MIKULICZ’S DISEASE)
The etiology has been speculated to be autoimmune, viral, or genetic factors
Commonly affects middle aged women.
Has unilateral or bilateral salivary gland swelling due to a benign lymphoid infiltration.
Reduced salivary flow and pain in the swelled gland.
Treatment - Palliative
DIFFERENTIAL DIAGNOSIS
Sjogren’s syndrome
Lymphoma
Sarcoidosis
Other diseases associated with salivary gland enlargement
Diagnosis – Based on biopsy
SJOGREN’S SYNDROME (PRIMARY
AND SECONDARY)
Is a chronic autoimmune disease characterized by symptoms of –
Oral and ocular dryness; lymphocytic infiltration and destruction of the exocrine glands.
The salivary and lacrimal glands are primarily affected, but other exocrine tissues like the thyroid, lungs, and kidney may also be affected.
Post menopausal women are affected most commonly.
CLINICAL FEATURES –
Due to oral dryness –
1.
2.
Frequent sipping of water, unable to speak due to dryness and great difficulty to have food due to lack of salivation.
Patients often have dry cracked lips and angular cheilitis.
3.
4.
5.
6.
Intraorally, the mucosa is pale and dry, saliva that is present tends to be thick and ropy.
Mucocutaneous candidal infections are common in this patient population
Increased dental caries and erosion of the enamel structure.
Have chronic salivary gland enlargement
DIAGNOSIS –
The strictest criteria include
1. Objective measurement of decreased salivary and lacrimal gland function.
2. Positive autoimmune serologies
3.
Minor salivary gland biopsy specimen that demonstrates focal mononuclear cell infiltration in a periductal pattern.
TREATMENT OF XEROSTOMIA
Preventive Therapy –
Salivary stimulation –
Fluoride application
Use of smell of favourite food
Pit and fissure sealants
Use of salt or sour taste at the
Antifungal application may tip of tongue be needed due to oral
Medicinal Treatment – dryness
1.
Bromhexine (mucolytic)
Symptomatic –
2.
Anetholetrithione
Use of chewing gums
(mucolytic)
Advising frequent sipping of
3.
Pilocarpine hydrochloride – water most preferred acts by
Avoiding anxiety and parasympathomimetic drug.
depression by giving anti
4.
Cevimeline HCl.
depressive drugs
Medicinal Treatment –
Thank You
Any Questions ?