Aneurysms 3rd years
advertisement
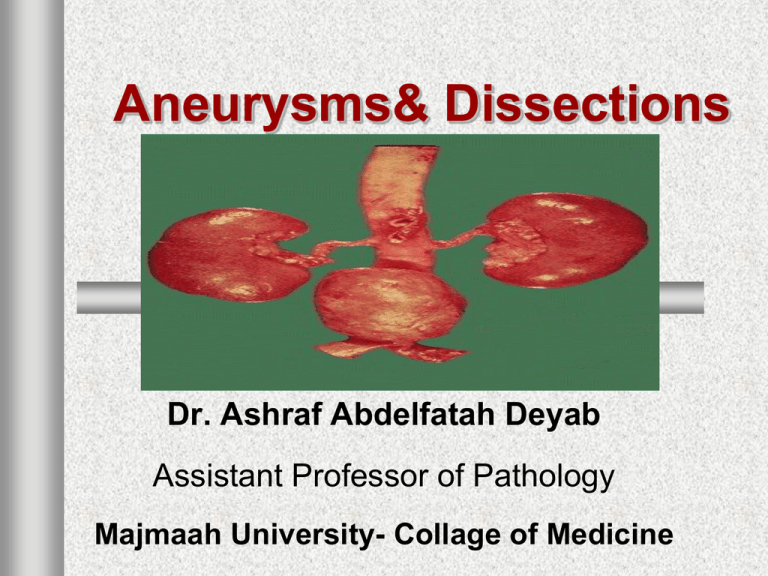
Aneurysms& Dissections Dr. Ashraf Abdelfatah Deyab Assistant Professor of Pathology Majmaah University- Collage of Medicine Aneurysm & Dissection objectives Aneurysms: definition & classification. Pathogenesis, morphology and clinical course of abdominal aortic aneurysm. Pathogenesis, morphology and clinical course of aortic dissection. Robbins Basic Pathology, 8th ed. p. 357 – 362 . Normal vessel- cross section Aneurysms- definition Aneurysm: one of the vascular disorders considered as leading cause of death in all over the world, esp. developed and western societies. Aneurysm: is localized, permanent, abnormal dilatation “blood-filled” of a blood vessel or heart, with extension to all three wall layers (intima, media, and adventitia). Aneurysm-site: small, medium, large BV+HRT. Male : female ratio (5:1)\ Age group > 5th decade Aneurysm classification-1 Different ways and system for classification; I. Based on morphological findings: A) Cylindrical, saccular, fusiform (macroscopic) B) True or False aneurysms (based on microscopic appearance). II. Based on etiological issue- (congenital or acquired causes). III. Based on location: Aneurysms can also be classified by their location(arterial>venous) (brain, aorta, kidneys, leg, ect..) Aneurysms- classified based on morphology-1 1) classified based on shape (of no clinical value) : Fusiform aneurysm (symmetrical spindle-shaped dilatation) Cylindroid or tubular (lengthy dilatation in the form of a cylinder) Saccular aneurysm (sack-like bulging on one side of the artery) Berry aneurysm (small saccular aneurysm the size of a berry) Aneurysms- based on morphological types-2 A true aneurysm is dilatation without tear, due to weakness that involves all 3 layers of the vascular wall (intima, media & adventitia), e.g. Atherosclerotic, syphilitic , and congenital A. , ventricular aneurysms . A false aneurysm, or pseudo-aneurysm, characterized by peri-vascular hematoma\ thrombus, over tear in the intima and media confined next to the vessel, surrounded by fibrous tissue - this enough to seal the leak, or may rupture out of the surrounding tissue. II. False Aneurysms classification •An. varix The following are the types of false aneurysms: (1) Pulsating Haematoma (Simple False Aneurysm) (2) Arterio-venous Fistula- Caused by traumatic injury to an artery, and adjacent vein. The injury results in either Aneurysmal varix, Varicose aneurysm •Simple false A. •Varicose A Aneurysm classification-based on etiology 1) Atherosclerosis& HTN: as result of persistant mechanical force>> lead to wall weakness& degeneration , (90%)occur in the abdominal aorta; Capillary micro-neurysm (HTN, DM& smoking): Brain& retina. 2) Infections& Mycotic aneurysm: bacterial sepsis& IE, sites: Brain, abdomen ,neck ,leg &arm. a) Syphilitic Aortitis (third stage) occur in the ascending& arch of aorta, which is due to obliterative endarteritis of the vasa vasorum b) Mycosis in immune-deficient patients Aneurysm classification-based on etiology 3) Congenital weakness of the media: Causes congenital cerebral aneurysms. Berry A. occurs in the circle of Willis; rupture of one arteries and lead to subarachnoid - hemorrhages 4) Trauma: Causes false aneurysms. 5) Immunologically mediated aneurysms (e.g., in polyarteritis nodosa). 6) Copper Deficiency. Rare cases of aneurysms= lead to a decreased activity of the lysyl oxidase enzyme, affecting elastin fibers. Aneurysm pathogenesis Aneurysms- Pathogenesis-1 Arteries are dynamically remodeling tissues. weakening of vessel walls due to inherited defects in connective tissues, is important in the common, sporadic forms. The intrinsic quality of the vascular wall connective tissue is poor, e.g. in Marfan syndrome, due to defective synthesis of scaffolding protein fibrillin which lead– weakening of elastic fibers. Cystic medial degeneration- cross-section of aortic media from a patient with Marfan syndrome showing marked elastic fragmentation (A), comparison to normal media (A) Aneurysm – Pathogenesis-2 The balance of collagen degradation and synthesis is altered by local inflammatory infiltrates and the destructive proteolytic enzymes they produce, such as in atherosclerosis. The vascular wall is weakened through loss of smooth muscle cells or the inappropriate synthesis of non-collagenous or non-elastic ECM, e.g. thickening of the intima+ medial ischemia of aorta in (atherosclerotic&HTN) Aneurysm morphology Aneurysms –Morphology-1 The intimal surface of the aneurysm shows severe atherosclerosis with destruction of the media. The aneurysm –contains poorly organized mural thrombus. The aneurysm can affect the renal and superior or inferior mesenteric arteries, either by producing direct pressure or by narrowing or occluding vessel ostia with mural thrombi. Aneurysms –Morphology-2 Tow general variants: Chronic Inflammation: dense periaortic fibrosis, abundant lymphoplasmacytic inflammation with many macrophages and often giant cells. Infection – bacterial infection with suppuration - destroys the media, lead to rapid dilation and rupture. Aneurysm clinical features Aneurysms-Clinical features-1 Pressure symptoms& signs: Impingement on an adjacent structure, e.g., compression of a ureter or erosion of vertebrae.. Rupture into the peritoneal cavity or retroperitoneal tissues with massive, potentially fatal hemorrhage Obstruction of a branch vessel resulting in ischemic injury of downstream tissues, iliac (leg), renal (kidney), mesenteric (GIT), or vertebral (spinal cord) arteries Aneurysms-Clinical features-2 Thrombo-embolism from Atheroma or mural thrombus. Presentation as an abdominal mass (often palpably pulsating) that simulates a tumor Complications of Aneurysms: (1) Pressure atrophy on the surroundings. (2) Spontaneous rupture - hemorrhagic shock will dominate the clinical picture: Acute risk to cerebral function (intra-craniazl&, subarachanoid)+ Acute pericardial tamponade (3) Thrombosis with ischaemic effects. 4) Emboli to distal vessels. 5) Dissection, serious complications predominantly occur in the region from the aortic valve through the arch with no underlying atherosclerosis Aneurysm & Dissection objectives Aneurysms: definition & classification. Pathogenesis, morphology and clinical course of abdominal aortic aneurysm. Pathogenesis, morphology and clinical course of aortic dissection. Robbins Basic Pathology, 8th ed. p. 357 – 362 . Aneurysm & Dissection objectives Aneurysms: definition & classification. Pathogenesis, morphology and clinical course of abdominal aortic aneurysm. Pathogenesis, morphology and clinical course of aortic dissection. Robbins Basic Pathology, 8th ed. p. 357 – 362 . Abdominal aortic Aneurysm AAA AAA- introduction AAA is localized abnormal ballooning dilatation of AA exceeding normal diameter- outer aortic diameter >3 cm (normal 2 cm). associated with atherosclerosis majority of cases occurs infra-renal, a few para-renal and supra-renal. Occur frequently in men and in smokers Most commonly in elderly over 60 yrs. CLASSIFED based on size& symptoms(> 5.5cm- Surgery ) AAA pathogenesis Atherosclerotic plaque in the intima compresses the underlying media and compromises nutrient and waste diffusion from the vascular lumen into the arterial wall. The media therefore undergoes degeneration and necrosis that results in arterial wall weakness and consequent thinning. The degradation of tunica media by means of proteolytic process& exposure of ECM>>> lead to elimination of elastin Reduced perfusion& nutrition of vasa vasorum in the AA (compared to thoracic A.)- damage of the AAA morphology Usually below renal& above bifurcation. Saccular or fusiform, up to 15 cm diameter up to 25 cm in length. Intimal surface showed severe complicated atherosclerosis with thinning of the underlying. laminated, poorly organized mural thrombus Renal, superior or inferior mesenteric arteries: AA producing direct pressure or by narrowing or occluding vessel ostia with mural thrombi Rupture as main complications AAA morphology-VARIANTS AAA-two variants: 1) Inflammatory Aortic Aneurysm: dense periaortic fibrosis containing abundant lymphoplasmacytic inflammation with many macrophages and often giant cells (uncertain cause) 2) Mycotic Aortic Aneurysm: infected by the lodging of circulating microorganisms in the wall, particularly in bacteremia from a primary Salmonella gastroenteritis- destroys the media-thinning. AAA clinical features They tend to cause no symptoms. Pressure symptoms and signs: pain, erosion of vertebra and ureter& legs pain (blood flow). Obstruction of vessel branch+ pulsating mass. The major complication of AA is rupture, into the abdominal cavity, and can lead to shock& death within minutes. Embolization+ Fistula formation Mortality of rupture repair in the hospital is 60% to 90%. Aneurysm & Dissection objectives Aneurysms: definition & classification. Pathogenesis, morphology and clinical course of abdominal aortic aneurysm. Pathogenesis, morphology and clinical course of aortic dissection. Robbins Basic Pathology, 8th ed. p. 357 – 362 . Abdominal aortic Dissection Aortic dissection-introduction Aortic dissection is medical emergency, previously called dissecting “aortic” aneurysm, associated with (HTN, AA, Marfan’s syndrome) Dissecting aneurysm occurs when blood splays apart the laminar planes of the media to form a blood-filled channel, under high forceful pressure with obvious perforation of the intima, (intra-mural hematoma). The word dissecting mean hematoma dissecting between the intima and the media or the media and the adventitia or through the layers of the media. Dissecting aneurysm : may or may not associate with dilatation.(not similar to athersclerotic& syphilitic aneurysms) Aortic dissection- Risk group (1)Adult aged 40 to 60, with antecedent HTN (> 90% of cases of dissection. (2) Younger patients with systemic or localized abnormalities of connective tissue affecting the aorta (e.g., Marfan syndrome). 3) Iatrogenic causes, after cardiac cathetrization. 4) Rare –of unknown etiology– after pregnancy. Key note: Dissection is unusual in the presence of atherosclerosis or syphilis, because of the medial scarring, fibrosis - inhibits propagation of the dissection. Aortic dissection- causes Hypertension- major risk factor. Connective tissue diseases Chest trauma. Vasculitis (rare). Aortic dissection- pathogenesis 1) Pressure-related mechanical injury: Aortas of hypertensive pt. have medial hypertrophy of the vasa vasorum with degenerative changes with loss of smooth muscle of Aortic media. ( (due to diminished flow through the Vasa Vasorum). 2) Inherited (congenital) or acquired connective tissue causing abnormal vascular ECM(e.g., Marfan syndrome, Ehlers-Danlos syndrome, vitamin C deficiency, copper metabolic defects). 3) Large groups of A. dissection remain unknown, a few with disruption of penetrating vessels of the vasa vasorum can give rise to an intramural hematoma without an intimal tear. Aortic dissection- morphology 1) Site: common portion (The ascending aorta), usually within 10 cm of the aortic valve. 2) cystic medial degeneration: most frequent preexisting histologically is. and is characterised by mucoid degeneration and elastic fibres fragmentation 3) Intimal tear with typically transverse or oblique and 1 to 5 cm in length, with sharp, jagged edges, not going retrograde towards the heart. 4) No significant inflammation. 5) Hematomas “Thrombus”, the dissecting hematoma reenters the lumen of the aorta through a second distal intimal tear, creating a new vascular channel “double-barreled aorta” = false channel, which with time endothelialized (become chronic dissection ) Histologic view of the dissection demonstrating an aortic intramural hematoma Aorta dissecting Aneurysm clinical features Aortic Dissection- clinical feature The nature of complications depend on site. (most serious complications: dissections of the aorta from the aortic valve to the arch). Symptoms sudden onset of pain, begin in the anterior chest, radiating to the back, moving downward as the dissection progresses; confused as MI. The common cause of death is rupture outward into the pericardial , pleural, or peritoneal cavities. Aortic insufficiency, and myocardial infarction summary of common complications The nature of complications depend on site. (most serious complications: dissections of the aorta from the aortic arch). 1-Cardiac tamponade. 2- Aortic insufficiency. 3-Myocardial infarction. 4-Renal, mesenteric, or iliac arteries, causing critical vascular obstruction 5-Compression of spinal arteries may cause transverse myelitis. 6-Thrombo-embolism Clinical classification of Aorta dissections Dr. Michael DeBakey (vascular surgeon) DeBakey type I = Type A (proximal) Ascending & Descending aorta, with extensive aorta dissection DeBakey type II = Type A (proximal) involves Ascending aorta, in isolation. DeBakey type III = Type B (distal ( dissections arise beyond the take off of the great vessels (distal to subclavian) -. DeBkey’s Classification of dissections Type I Type II Type III Aortic dissection management Aortic Dissection- management the mortality is at least 50% at 48 hours, and 90% within 1 week. I. Reducing blood pressure: immediate aim to control the propagating hematoma by reducing II. Surgical repair (plication of aorta wall) is feasible if the process affects the proximal aorta. NB: However thrombosis with organization and fibrosis may be regarded as a cure. •The end